Surgical and Prosthetic Considerations With Immediate Implant Placement
Mark Bishara, DDS; and Gregori M. Kurtzman, DDS, MAGD
Abstract
Immediate implant placement can pose challenges surgically and, ultimately, restoratively. Yet immediate placement has become the standard when adequate bone is present to achieve primary stability and site infection is minimal. To avoid prosthetic complications and ensure the implant is encased in bone after healing, proper planning must consider that implant placement does not necessarily need to follow the trajectory of the root socket. As discussed in this article, maxillary anterior sites have potential issues related to the “triangle of bone” that are not encountered in molar sites and demand different approaches to ensure treatment success. Additionally, this article addresses decision-making on molar sites in regard to implant diameter, as well as the rationale for platform switching.
Immediate placement of dental implants has become common practice for a variety of reasons. It shortens treatment time and aids in the maintenance of hard tissue that may resorb after healing of the extraction site. Immediate placement also decreases the number of procedures required to complete treatment, with comparable success rates to delayed placement.1 Important factors to consider with immediate dental implant placement as a treatment option include: presence of a complete buccal plate, ability to achieve primary stability of the implant in the extraction socket, implant design, crestal width of the socket, the potential gap between the implant and buccal crestal aspect of the socket, and the patient’s tissue biotype.
Atraumatic extraction is a key element for immediate dental implant placement to maintain an intact socket at the crestal aspect. Raising a flap compromises the blood supply to the buccal plate.2 Flapless techniques may cause less bone resorption crestally because periosteal blood supply is maintained,3 and they reduce postoperative patient discomfort.4 An intact buccal wall is important for preventing esthetic complications (ie, recession related to crestal resorption), especially in the esthetic zone.5 Ideally, maintaining a minimum of 2 mm of buccal wall thickness has been recommended to ensure stability of the restoration in both the short and long term.6
Challenges With Immediate Implant Placement
Achieving primary stability is typically the main challenge with immediate implant placement. The osteotomy preparation is often undersized to allow the threads of the implant to better engage the bone, usually in the apical area below the extracted tooth’s apex. However, anatomical limitations (eg, maxillary sinus, inferior alveolar nerve, etc) must be considered. In certain cases, using a wider-body implant may allow better engagement of the perimeter bone of the socket.
After the implant is placed, a gap between the implant and buccal aspect of the crest may be present. Tarnow has reported7 that a blood clot will fill the gap at the time of surgery and convert to bone as healing progresses, even when the gap is up to 4 mm wide. Ferrus8 demonstrated that filling the gap with a biomaterial of choice improves marginal bone-to-implant contact (BIC), minimizes soft-tissue recession, and improves the hard-tissue healing process.
The width of the implant selected for the site will depend on the dimensions of the tooth being replaced and the available space that can house the implant in the bone. A dental implant of 3 mm to 3.5 mm in diameter is adequate for central and lateral incisors; for canines, 4 mm in width is recommended; premolars, 3.5 mm to 4 mm; and molars, 4 mm to 5 mm.9
Tissue biotype also plays an important role in long-term prosthetic success. Patients with a thin biotype may require soft-tissue augmentation either at the time of placement or sometime later before restoration of the implant.10 Immediate provisionalization of the implant can help maintain soft-tissue contours and prevent loss of papilla that is present at the time of extraction. Replacing lost papilla can be challenging, especially in the esthetic zone.
Maxillary Anterior
Immediate implant placement in the anterior needs to follow the so-called “triangle of bone.”11 Healthy teeth in the maxillary anterior may present with a fenestration or dehiscence. When implants are placed following the trajectory of the extraction socket, it may leave the buccal aspect of the implant either without osseous coverage or with only a thin bone covering. A natural undercut is present in the premaxilla, which can create challenges to implant placement similar to those associated with the extraction socket (Figure 1). A natural tendency for an inexperienced practitioner may be to follow the extraction socket because doing so simplifies the surgical process.
However, to ensure complete encapsulation of the implant in bone and adequate thickness of the buccal plate, the implant trajectory needs to be tipped palatally (Figure 2). Realignment of the trajectory provides the added benefit of the implant’s apical portion being in bone, thereby increasing primary stability. A pilot drill is used to redirect the osteotomy two-thirds to three-quarters down the palatal wall of the socket. The angle of the bur will depend on whether a cement- or screw-retained crown will be used, implant design, and abutment/implant connection. Multiunit abutments may be used to correct implant angulation if a screw-retained prosthesis is planned, but doing so may create esthetic complications related to the interarch space available, depth of the implant, and thickness of soft tissue at the crest.
The density of the buccal crest is lower than that of the palatal crest, making this bone more susceptible to resorption after implant placement. A factor that can influence resorption is pressure from the implant on the thin bone at placement. Thus, it is recommended that the implant be placed leaving a 2-mm to 3-mm gap at the crest from the buccal plate.12 When implants are placed in contact with the buccal crest—filling the socket with an implant of comparable size to the root just extracted—resorption of the thin buccal crest occurs, leading to soft-tissue recession and esthetic complications.
Posterior Considerations
Smith and Tarnow have classified extraction sockets in the posterior into three types, helping to guide treatment. Illustrated in Figure 3, these classifications aid clinicians in determining whether or not to place an implant at the time of extraction.13
Type A socket: The socket has sufficient septal bone to surround the entire implant, and primary stability is supplied entirely by the septum (Figure 3, left).
Type B socket: The septal bone partially surrounds the implant, enough to achieve a minimal torque value, although sometimes the implant may need to be placed slightly apical (3 mm to 5 mm) to achieve primary stability (Figure 3, center).14
Type C socket: The shape of this type of socket resembles an hourglass, where the thickened area corresponds to the furcation (Figure 3, right). The problem in placing immediate implants in this type of site is that engagement with the socket will require a wide-body implant (7 mm to 9 mm width) to achieve primary stability with the buccal and lingual walls. This type of socket may be better managed using a staged surgical approach, grafting the socket at extraction, and placing the implant at a later date.
A typical type B socket in a lower molar site presents with adequate bone in the furcation area after extraction (Figure 4). Initial osteotomy preparation is created with a pilot drill in the center of the furcal bone (Figure 5). A round surgical bur may be used to create a pilot point to keep the pilot drill from redirecting into one of the root spaces. The osteotomy may then be expanded with wider osteotomy drills to an adequate width for implant placement (Figure 6). This may lead to an implant that achieves primary stability but that is not fully contained within the septal bone, and grafting of the voids in the socket may be required.
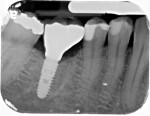
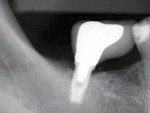
Figure 7 and Figure 8 radiographically illustrate implant placement in a type B socket.
In a typical type A socket in maxillary molar sites the implant will be in contact circumferentially with bone at the crest (Figure 9). Although the implant will be fully contained within the septal bone (Figure 10), prosthetic issues may materialize such as food traps and hygiene difficulties because of the variance between the implant and mesial–distal space of the extracted molar (Figure 11).
Wide-body dental implants designed for immediate molar replacement aid in replicating the missing tooth (Figure 12). They better engage the palatal mesial–distal socket walls at placement, improving primary stability. As in the anterior region, the implant should be kept 2 mm to 3 mm away from the buccal plate to minimize potential crestal resorption during healing. Wide-body implants may be used in regions of thin septal bone or anatomical limitation (eg, conical rooted molars such as type C sockets, sinus limitations, nerve proximity). Additionally, these implants more closely approximate the missing tooth dimensionally, allowing better restorative contours and limiting potential food traps interproximally (Figure 13).
In recent years “super-wide” implants (8 mm or wider) have been used in immediate molar extraction sites (Figure 14). These implants maximize initial contact with the extraction socket walls, essentially obliterating the socket and providing better initial stability. Because these implants have high BIC, shorter implants can be used, which allows placement with minimal or no auxiliary procedures, such as sinus augmentation, and avoidance of the inferior alveolar nerve. These implants maximally fill the space, so potential interproximal food traps can be greatly minimized, allowing the patient to perform better homecare (Figure 15).
Achieving primary stability in thin septal bone using narrow or standard-size implants has a degree of difficulty. Often, the osteotomy must be extended further apically to allow sufficient primary stability. This extension may be difficult to achieve due to anatomical limitations, including proximity of the inferior alveolar nerve canal or maxillary sinus. In extraction sockets of multi-rooted teeth, placing the dental implant in distal (Figure 16) or mesial (Figure 17) root spaces should be avoided, because this creates a cantilever effect on the resulting crown with associated off-axis loading as well as subsequent food-trap susceptibility (Figure 18 and Figure 19). Implants are best loaded centrally, and placement of the implant should be directed to the center of the socket, regardless of the root spaces present in the extraction socket (Figure 20). Doing so may require use of a wider-body implant that is able to engage the perimeter bone for initial stability, without having to rely on deeper placement.
Platform Switching
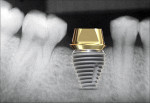
Traditionally, an abutment was used that matched the width of the implant; however, this presented a challenge restoratively, especially when wider-diameter implants were used (Figure 21). For better management purposes, the concept of platform switching was developed. Platform switching refers to placing abutments of a narrower diameter on an implant of wider diameter (Figure 22). This strategy enables thicker gingival tissue at the abutment–implant connection, which improves soft-tissue stability and restorative esthetic results.15 It is believed that crestal bone loss is decreased with platform switching.16
The depth of implant placement depends on the region of the mouth and the specific site. At the crestal bone level for a molar, the implant will be deep enough to create a proper emergence profile for the restoration. If platform switching is planned and a super-wide implant is being used, the implant may need to be placed subcrestally to enable development of a proper emergence profile (Figure 23). If the dental implant is placed level with the crest or supracrestally, it may be difficult to establish a natural-appearing emergence profile of the ensuing restoration, partly because of limitations in the available interarch space.
Figure 24 radiographically illustrates an actual case using platform switching with a super-wide-body implant.
Conclusion
Implant dentistry is a restorative-driven treatment with a surgical aspect. The practice becomes especially challenging when immediate implant placement is planned and the clinician needs to work with the extraction socket present. With proper surgical planning, complications in the restorative phase of treatment can be minimized or even eliminated, and natural-appearing restorations can be provided that are easy to maintain by the patient with homecare.
Author’s Note
Figures 11, 13, 15 through 17, and 20 through 23 are images of radiographs with illustrations of implants and/or abutment heads superimposed over the radiograph. They are for illustrative purposes only and do not depict actual cases.
Acknowledgements
Illustrations created by Dr. Gregori M. Kurtzman
About the Authors
Mark Bishara, DDS
Private Practice
Bowmanville, Ontario, Canada
Gregori Kurtzman, DDS, MAGD
Private Practice
Silver Spring, Maryland
References
1. Romanos G, Froum S, Hery C, et al. Survival rate of immediately vs delayed loaded implants: analysis of the current literature. J Oral Implantol. 2010;36(4)315-324.
2. Oh TJ, Shotwell J, Billy E, et al. Flapless implant surgery in the esthetic region: advantages and precautions. Int J Periodontics Restorative Dent. 2007;27(1):27-33.
3. Mazzocco F, Jimenez D, Barallat L, et al. Bone volume changes after immediate implant placement with or without flap elevation. Clin Oral Implants Res. 2017;28(4):495-501.
4. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004(19 suppl):43-61.
5. Funato A, Salama MA, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27(4):313-323.
6. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5(1):119-128.
7. Tarnow DP, Chu SJ. Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft or membrane: a case report. Int J Periodontics Restorative Dent. 2011;31(5):515-521.
8. Ferrus J, Cecchinato D, Pjetursson EB, et al. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Impl Res. 2010;21(1):22-29.
9. Li T, Hu K, Cheng L, et al. Optimum selection of the dental implant diameter and length in the posterior mandible with poor bone quality—a 3D finite element analysis. Appl Math Model. 2011;35(1):446-456.
10. Kan JY, Rungcharassaeng K, Morimoto T, Lozada J. Facial gingival tissue stability after connective tissue graft with single immediate tooth replacement in the esthetic zone: consecutive case report. J Oral Maxillofac Surg. 2009;67(11 suppl):40-48.
11. Ganz SD. The triangle of bone—a formula for successful implant placement and restoration. Implant Soc. 1995;5(5):2-6.
12. Greenstein G, Cavallaro JS. Managing the buccal gap and plate of bone: immediate dental implant placement. Dent Today. 2013;32(3):70-77.
13. Smith RB, Tarnow DP. Classification of molar extraction sites for immediate dental implant placement: technical note. Int J Oral Maxillofac Implants. 2013;28(3):911-916.
14. Schwartz-Arad D, Chaushu G. Placement of implants into fresh extraction sites: 4 to 7 years retrospective evaluation of 95 immediate implants. J Periodontol. 1997;68(11):1110-1116.
15. Deng F, Xu J, Luo Z, et al. Comparison between platform-switching and traditional implant-abutment connections in esthetic areas: a clinical retrospective study. Clin Oral Implants Res. 2014;25(suppl 10);565.
16. Sesma N, Garaicoa-Pazmino C, Zanardi PR, et al. Assessment of marginal bone loss around platform-matched and platform-switched implants—a prospective study. Braz Dent J. 2016;27(6):712-716.