Is Residual Bone Height an Absolute Indicator for Simultaneous Implant Placement in Lateral Wall Sinus Grafting?
Lanka Mahesh, BDS, MS; Gregori M. Kurtzman, DDS, MAGD, DICOI; and Sagrika Shukla, MDS, DICOI
Abstract
Placement of an implant in the posterior maxilla often relies heavily on a variety of procedures that increase the vertical dimensions of available bone. With numerous bone graft substitutes now available and recent advancements having been made in technique, the question arises of whether residual bone height still remains an absolute indicator for simultaneous implant placement in lateral wall sinus grafting. In addition to reviewing the literature, the authors present a case in which a direct sinus lift procedure was performed with simultaneous implant placement. The case report demonstrates how implants can be placed in a severely atrophic posterior maxilla and be successful.
For implant placement, the posterior maxilla is the most problematic and difficult-to-treat intraoral area.1 Nonetheless, sinus grafting surgeries have become an integral part of implant treatment procedures, as thousands of patients annually undergo sinus augmentation to allow implant placement.1 Placing an implant in the posterior maxilla often relies heavily on various procedures that increase the vertical dimensions of available bone. Pommer and colleagues2 state that the minimum requirements to allow implant placement are bone that is at least 10 mm in height and 3 mm to 4 mm in diameter. Fortunately, a variety of options are available to modulate the quality and quantity of bone available, thus overcoming the intrinsic limitations of dental implant placement in this region.
Both anatomical structures and mastication contribute to the long-term survival rates of endosseous dental implants in the posterior maxilla.1 However, many other variables also contribute to implant success, the foremost of which is the quality and quantity of residual bone present.3 In 1987, Misch3 developed a classification for the treatment of the edentulous posterior maxilla based on the amount of bone available below the antrum and the ridge crest, indicating the following treatment plan: SA1, adequate vertical bone for implants (ie, 12 mm) and no manipulation of the sinus is required; SA2, 0 mm to 2 mm less than the ideal bone height and may require surgical correction; SA3, only 5 mm to 10 mm of bone below the sinus; and SA4, less than 5 mm of bone below the sinus.
All the surgical protocols follow these guidelines. Implant placement with or without sinus augmentation or direct sinus lift with simultaneous implant placement depend on residual bone availability, which is done according to the aforementioned surgical protocol. With various bone graft substitutes now available and recent advancements having been made in technique, the question arises of whether residual bone height still remains an absolute indicator for simultaneous implant placement in lateral wall sinus grafting.
Case Report
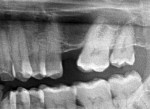
A 44-year-old man presented with a missing maxillary left first molar and wanted the tooth replaced. A complete blood count indicated that the patient, who was a nonsmoker, had no systemic disease. Radiographic imaging showed an atrophic maxilla with 2 mm of bone available between the crest and the sinus floor (Figure 1). A direct sinus lift procedure with simultaneous implant placement was planned.
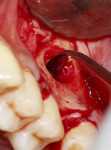
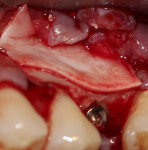
During surgery, after sufficient local anesthesia was achieved, a full-thickness mucoperiosteal flap was elevated in the region of interest and a lateral window was prepared using an SLA Kit (Neobiotech, neobiotechus.com) (Figure 2). Gentle elevation of the osseous window (Figure 3) and sinus membrane was achieved using sinus curettes (Figure 4). Osseous graft material was introduced into the elevated sinus, with 1 cc of cerabone® (botiss biomaterials GmbH, botiss.com) being placed into the antrum. Approximately 75% of the graft material was placed before implant placement (Figure 5) to ensure that the implant would be surrounded by graft material without voids. The graft material used in this case is derived from the mineral phase of bovine bone and has a strong resemblance to human bone with regard to chemical composition, porosity, and surface structure. The porous network in the bone graft material particles enables a fast penetration and adsorption of blood and serum proteins and serves as a reservoir for proteins and growth factors as the graft matures.4
An osteotomy was created at the crest, through the native bone of the ridge and into the graft material. A Bioner Top DM implant 9 (Bioner, bioner.es), 4 mm x 11.5 mm, was inserted into the prepared site (Figure 6). The remaining bone graft material was packed over the implant to completely cover the lateral window on the ridge (Figure 7).
A resorbable membrane (Jason®, botiss biomaterials) was placed over the lateral osseous window of the grafted site (Figure 8). This membrane uses porcine percardium and consists of collagen. Porcine pericardium offers such advantages as low membrane thickness, easy manipulation (wet or dry), slow degradation because the type III collagen content provides a long-term barrier, and high tear resistance.5 The site was closed using resorbable 3-0 cytoplast sutures (Osteogenics Biomedical, osteogenics.com). A periapical radiograph was taken to document the graft and simultaneous implant placement (Figure 9).
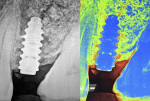
The postoperative healing period was uneventful. A cone-beam computed tomography (CBCT) scan taken at 5 months to check the 3D fill of the graft around the implant revealed a well-integrated implant and good maturation of the bone graft (Figure 10). Apart from the CBCT, histological evidence is a time-tested method to validate bone graft maturation; however, in patients who have an implant placed simultaneously, as did this patient, a trephine core biopsy was deemed unnecessary. The implant cover screw was uncovered using a tissue punch, and impressions were taken for the implant restoration. Following conventional protocols,3 a screw-retained porcelain-fused-to-metal crown was fabricated and placed.
A periapical radiograph taken 2 years after restoration (Figure 11) showed stable crestal bone levels and the entire implant, including the apical portion, surrounded by dense bone.
Discussion
The posterior maxilla poses various clinical challenges. After tooth extraction, up to 25% bone loss occurs in the initial 6 months, and bone continues to resorb in the absence of a tooth or implant in the site.6 The maxillary sinus increases with age and its increased pneumatization7,8 makes implant placement difficult, especially when the site has been edentulous for a period of time. With various modifications of the traditional sinus lifting procedures and bone grafting, however, this treatment has become not only an easy procedure but a predictably successful9-12 method of tooth replacement with an implant.
The Report of the Sinus Consensus Conference of 199610 clearly stated that in a class A scenario (residual bone height > 10 mm), classical implant protocol could be followed. When a class B (7 mm to 9 mm residual bone height) was present, simultaneous implant placement along with bone-added osteotome sinus floor elevation could be done. With a class C (4 mm to 6 mm residual bone height), a lateral approach involving a grafting material with immediate or delayed implants is advocated. Finally, with a class D (1 mm to 3 mm residual bone height), a lateral approach involving a bone grafting material and delayed implant placement is recommended.10
In the present case report, the ridge was only 2 mm in height and atrophic and, therefore, was both class D and in the SA4 category of the Misch3 classification. Consequently, ideal treatment would be a lateral approach involving a bone grafting material and delayed implant placement. The literature suggests that, in ridges with lower heights (< 10 mm), a two-phase procedure is recommended.10,13,14 In 2010, however, Lambert and coworkers15 suggested that simultaneous implant placement and sinus grafting procedures could be performed on severely atrophic ridges, which decreased morbidity, costs, and the total time of treatment considerably, showing it to be a more desirable treatment option. The present case was consistent with many studies done in which similar surgical protocols were followed with success rates of 90% to 95%.7, 14-17
In a study, Peleg and colleagues14 reported a 100% success rate of 55 hydroxyapatite-coated implants placed in 20 simultaneous sinus lifts in patients with only 1 mm to 2 mm of residual bone. Manso and Wassal,16 in a 10-year longitudinal study, reported on 160 implants placed in severely atrophic posterior maxilla, concluding that advanced posterior maxillary resorption with extensive expanded sinus (SA4) can be safely treated by a simultaneous sinus lift approach and implant insertion with survival and success rates up to 98.05% and 94.85%, respectively. Chiapasco and coworkers,7 after performing 9,052 sinus lifts in different categories of ridge resorption, stated that maxillary sinus floor elevation and grafting with autogenous particulated bone via a lateral approach is a safe and predictable procedure that also allows implant placement in severely resorbed posterior maxillae. In another study, Peleg and coworkers17 evaluated atrophic posterior maxillae for which only the simultaneous approach was used in a 9-year longitudinal study with 2,123 implants placed and reported a survival rate of more than 97% (44 implants failed).
Considering recent scientific advancements, the authors suggest that residual bone height is not an absolute contraindicator for simultaneous implant placement in lateral wall sinus grafting, which was clearly not the case in previous decades. Since the publication of a sinus lift procedure in 1980 by Boyne and James,18 implant surfaces, grafting materials, and sinus lift procedures have advanced considerably.19 Reviewing the literature, the results of sinus lift procedures are difficult to compare because different graft materials were used; many publications lacked well-defined criteria for the success rates of reconstructive procedures; and well-defined parameters of the initial clinical situation were rarely presented.7
In a systematic review, however, Wallace and Froum19 determined the efficacy of sinus augmentation procedures and compared the results. They reported that the survival of implants in augmented sinuses via a lateral window procedure varied from 61.7% to 100%, with an average survival rate of 91%. Further, they reported that sinuses augmented with particulate showed a higher survival rate compared with sinuses augmented with bone blocks and that the survival rate increased when the lateral window was covered with a membrane.19 In the present study, however, the authors wish not to comment on bone graft substitutes because the emphasis of this case report is that implants can be placed in a severely atrophic posterior maxilla and still be successful.7,9-14,20
Conclusion
Though not a case series demonstrating consistent reproduction of results, this single case report showed successful implant placement in a severely atrophic posterior maxilla and that residual bone height is not an absolute indicator for simultaneous implant and grafting procedures. The main criteria for simultaneous implant placement are the surface treatment on the implant, the primary stability of the implant, and the vascularity of the area.
About the Authors
Lanka Mahesh, BDS, MS
Private Practice
New Delhi, India
Gregori M. Kurtzman, DDS, MAGD, DICOI
Private Practice
Silver Spring, Maryland
Sagrika Shukla, MDS, DICOI
Private Practice
New Delhi, India
References
1. Karacayli U, Dikicier E, Dikicier S. Dental implant placement in inadequate posterior maxilla. In: Turkyilmaz I, ed. Current Concepts in Dental Implantology. Rijeka, Croatia: InTech; 2015:105-125.
2. Pommer B, Zechner W, Watzek G, Palmer G. To graft or not to graft? Evidence-based guide to decision making in oral bone graft surgery. In: Zorzi A, Batista de Miranda J, eds. Bone Grafting. Rijeka, Croatia: InTech; 2012:159-182.
3. Misch CE. Contemporary Implant Dentistry. 3rd ed. St Louis, MO: Mosby; 2007:934-936.
4. Rothamel D, Schwartz F, Smeets R, et al. Sinus floor elevation using a sintered natural bone mineral. A histological case report study. Zzi. 2011;27(1):60-70.
5. Artzi Z, Wasersprung N, Weinreb M, et al. Effect of guided tissue regeneration on newly formed bone and cementum in periapical tissue healing after endodontic surgery: an in vivo study in cat. J Endod. 2012;38(2):163-169.
6. Bhaskar SN. Orban’s Oral Histology and Embryology. 11th ed. St Louis, MO: Mosby; 1992:239-259.
7. Chiapasco M, Zaniboni M, Rimondini L. Dental implants placed in grafted maxillary sinuses: a retrospective analysis of clinical outcome according to the initial clinical situation and a proposal of defect classification. Clin Oral Implants Res. 2008;19(4):416-428.
8. Kolhatkar S, Cabanilla L, Bhola M. Inadequate vertical bone dimension managed by bone-added osteotome sinus floor elevation (BAOSFE): a literature review and case report. J Contemp Dent Pract. 2009;10(3):81-88.
9. Wheeler SL, Holmes RE, Calhoun CJ. Six-year clinical and histologic study of sinus-lift grafts. Int J Ora Maxillofac Implants. 1996;11(1):26-34.
10. Jensen OT, Shulman LB, Block MS, Iacono VJ. Report of the Sinus Consensus Conference of 1996. Int J Oral Maxillofac Implants. 1998;13(suppl):11-45.
11. Rodoni LR, Glauser R, Feloutzis A, Hämmerle CH. Implants in the posterior maxilla: a comparative clinical and radiologic study. Int J Oral Maxillofac Implants. 2005;20(2):231-237.
12. Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006;17(suppl 2):136-159.
13. Chiapasco M, Zaniboni M. Methods to treat the edentulous posterior maxilla: implants with sinus grafting. J Oral Maxillofac Surg. 2009;67(4):867-871.
14. Peleg M, Mazor Z, Chaushu G, Garg AK. Sinus floor augmentation with simultaneous implant placement in the severely atrophic maxilla. J Periodontol. 1998;69(12):1397-1403.
15. Lambert F, Lecloux G, Rompen E. One-step approach for implant placement and subantral bone regeneration using bovine hydroxyapatite: a 2- to 6-year follow-up study. Int J Oral Maxillofac Implants. 2010;25(3):598-606.
16. Manso MC, Wassal T. A 10-year longitudinal study of 160 implants simultaneously installed in severely atrophic posterior maxillas grafted with autogenous bone and a synthetic bioactive resorbable graft [published erratum appears in Implant Dent. 2010;19(5):364]. Implant Dent. 2010;19(4):351-360.
17. Peleg M, Garg A, Mazor Z. Predictability of simultaneous implant placement in the severely atrophic posterior maxilla: A 9-year longitudinal experience study of 2132 implants placed into 731 human sinus grafts. Int J Oral Maxillofac Implants. 2006;21(1):94-102.
18. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38(8):613-616.
19. Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003;8(1):328-343.
20. Chen TW, Chang HS, Leung KW, et al. Implant placement immediately after the lateral approach of the trap door window procedure to create a maxillary sinus lift without bone grafting: a 2‑year retrospective evaluation of 47 implants in 33 patients. J Oral Maxillofac Surg. 2007;65(11):2324-2328.