Management of a Malpositioned Implant in the Anterior Maxilla
Catherine DeFuria, DMD; Hans-Peter Weber, DMD, Dr. Med. Dent.; Yukio Kudara, CDT, MDT; and Panos Papaspyridakos, DDS, MS, PhD
Abstract
The surgical and prosthodontic management of patients with multiple missing teeth in the anterior maxilla can be challenging. The purpose of this clinical report is to illustrate the 2-year outcome after immediate implant placement in unintentional close proximity with the adjacent root. Following uneventful healing, the definitive implant rehabilitation was done with a modified monolithic zirconia framework and porcelain veneers bonded to the framework. The patient’s satisfaction with the functional and esthetic outcomes remained high throughout the observation time, with no symptoms or biologic and technical complications.
Prosthodontic rehabilitation of multiple missing teeth in the maxillary esthetic zone represents one of the most challenging clinical situations in implant dentistry.1,2 When using multiple implants, at least 3 mm of space should exist between adjacent implants and 1.5 mm between an implant and adjacent teeth.3,4 Interdental space limitations or inadequate planning may lead to implant-to-root proximity less than the suggested 1.5 mm. Orthodontic studies have considered the proximity of the orthodontic miniscrew and its contact with the dental root as the most important risk factor for failure of the miniscrew, with tooth devitalization and external root resorption also being essential issues.5-7 Recent studies have reported on the outcomes of implants placed touching the tooth or root fragments, with mixed results.8,9
Site development prior to implant placement in the anterior maxilla can be performed surgically and prosthodontically. Guided-bone regeneration (GBR), socket preservation, block grafts, connective tissue grafts, root-submergence technique, and pink ceramics have been used separately or in combination to enhance the outcomes of implant therapy in the esthetic zone.10-12
Newer materials are being used in fixed implant prosthodontics, namely zirconia and lithium disilicate, and can be layered or monolithic. To compensate for the increased porcelain chipping rate with porcelain-fused-to-zirconia implant prostheses, monolithic zirconia has been introduced.13 Recently, few studies have reported preliminary favorable outcomes with full-arch implant rehabilitation.14-17 Not enough data exist regarding patients with partially edentulous cases.
Hence, the purpose of this clinical report is to illustrate the 2-year outcome after immediate implant placement with unintentional root proximity. Following uneventful healing, the definitive restoration was done with a screw-retained monolithic zirconia framework with pink ceramics and porcelain veneers adhesively bonded to the zirconia framework.
Clinical Report
Case History
A healthy 32-year-old Caucasian female presented to the postgraduate prosthodontic clinic of Tufts University School of Dental Medicine in Boston, Massachusetts, seeking implant treatment (Figure 1 and Figure 2). Findings from comprehensive clinical and radiographic examinations revealed anterior maxillary partial edentulism due to fractured left central incisor. The right lateral incisor was previously endodontically treated and restored with a porcelain-fused-to-metal (PFM) crown, with receded margins and recurrent marginal caries, while the presence of cervical resorption was confirmed. The right central incisor was restored with a cement-retained PFM single-implant crown (Replace Select, Nobel Biocare, nobelbiocare.com) with mucosal recession, due to an excessively facial implant placement. The left central incisor was fractured, and the retained root tip had recurrent caries. The left lateral incisor had been previously restored with the use of a porcelain veneer. No other significant findings were noted in the remaining dentition.
After a diagnostic workup, the treatment options were presented to the patient, and the decision was made to restore the failing right lateral and left central incisors, as well as the missing right central incisor with a 3-unit implant fixed dental prosthesis (FDP) supported by two implants. In addition, crown lengthening and porcelain-laminate veneers were proposed for the restoration of the canines; however, the patient refused this option due to financial limitations.
Surgical Procedures
Prior to the implant surgical appointment, the patient had an emergency appointment for the right lateral incisor that had fractured equigingivally (Figure 3). The fractured right lateral incisor was decoronated, the left central incisor remaining root tip was also decoronated, and the old right central incisor PFM implant crown was removed. A screw-retained interim FDP was fabricated, supported by the osseointegrated left central incisor implant, with cantilever extension for right lateral and left central incisors (Figure 4) and adjusted to be out of occlusion during excursive movements.
On the day of the surgical procedure, local infiltration with articaine HCl 4% with epinephrine (1:100,000) was completed, and the root tip of the left central incisor was atraumatically extracted without a flap reflection. An intact socket remained with no fenestrations or dehiscences and a buccal plate of approximately 1-mm thickness. Drilling of the implant bed was then performed according to the standard protocol with the aid of a surgical template. A 3.5-mm-diameter and 11.5-mm-long dental implant (Replace Select, Nobel Biocare, nobelbiocare.com) was immediately placed into the extraction socket with good primary stability. A healing abutment was positioned, and 0.5-gram sterile cancellous granules of xenograft (Bio-Oss®, Geistlich Pharma, geistlich-pharma.com) were placed around the implant, followed by suture placement.
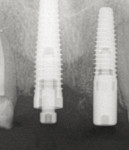
Following the immediate implant placement, the cantilevered screw-retained interim FDP was retightened. Findings from the post-placement periapical radiograph revealed an unexpected proximity of the implant to the adjacent root (Figure 5). The patient was informed of the potential risk for devitalization and/or external root resorption of the left lateral incisor.8,9 After the discussion with the patient, the decision was to leave the implant in place and monitor the status with frequent follow-up visits.
At the next visit and after completion of the endodontic retreatment of the right lateral incisor, submergence of the root tip was performed with a surgical round bur No. 4 in a semilunar motion to the level of the alveolar crest (Figure 6).
Prosthodontic Procedures
After uneventful healing for 3 months, successful osseointegration of the left central incisor was confirmed, while the left lateral incisor had no pathologic signs or symptoms. The decision was taken to proceed with implant fixed provisionalization (Figure 7).
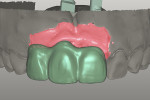
After an 8-month period of soft-tissue conditioning and observation, the patient presented for the definitive impressions. Impression copings were connected to the implants and splinted together with dental floss and visible light-polymerizing acrylic resin (Triad Gel, Dentsply Caulk, dentsply.com), prior to the impression.18 The cast of the interim FDP and the definitive implant cast were digitally scanned with a laboratory scanner (Activity 880 scanner, Smart Optics, smartoptics.de). The generated standard tesselation language (STL) files were overlapped, and the files were imported into a computer-aided design (CAD) software program (Exocad DentalCAD, Exocad Gmbh, exocad.com) coupled with the use of a computer-aided manufacturing (CAM) milling unit (Tizian™ Cut Eco plus, Schutz Dental Group, sdginnovations.com). A trial prosthesis was milled from prefabricated polymethyl methacrylate (PMMA) blocks (ZCAD Temp-Fix 98, Harvest Dental Products).
At the next clinical visit, the PMMA prosthesis try-in was performed (Figure 8). Due to the fact that the screw-access channel was on the facial aspect of the right central incisor, the decision was made to fabricate a monolithic zirconia framework with facial cutback for the cementation of three porcelain laminate veneers.19 At the laboratory, the framework was milled from zirconia monoblocks (Katana HT zirconia block, Kuraray Noritake, kuraraynoritake.com). Mutually protected occlusion with anterior guidance was the prescribed occlusal scheme (Figure 9 and Figure 10). At the following clinical visit, the screw-retained maxillary zirconia framework and the veneers were tried in (Figure 11).
Bonding to Zirconia Procedures
At the final insertion appointment, the internal surfaces of the lithium-disilicate veneers (IPS e.max®, Ivoclar Vivadent, ivoclarvivadent.us) were etched for 20 seconds with 4.9% hydrofluoric acid, rinsed with water for 1 minute, and air-dried with oil-free air. Then, a 10-methacryloyloxydecyl dihydrogen phosphate (MDP)-containing bonding/silane coupling agent mixture (Clearfil™ Ceramic Primer, Kuraray Europe, kuraraydental.com) was applied on both the zirconia framework and etched surfaces of the veneers for 60 seconds before adhesive cementation. Furthermore, self-adhesive resin cement (Clearfil SA Cement, Kuraray Europe) was used for the cementation procedure. The veneers not involving the facial screw-access hole were then bonded extraorally (Figures 12 and Figure 13).20 Oral-hygiene instructions were given to the patient so she could clean around the implant FDP. Adequate space had been provided, and the patient was instructed on how to clean the interface between the pink porcelain and the gingiva with proxy brushes and floss through the designated space.
One week later, the patient expressed her satisfaction with the esthetics and function. A nightguard was delivered to protect the prostheses from porcelain chipping and parafunctional activity. The 2-year clinical recall and radiographic examination showed a stable and pleasant outcome (Figures 14 and Figure 15), and the patient remained satisfied.
Discussion
This clinical report illustrates the 2-year outcome following prosthodontic rehabilitation with a monolithic zirconia framework and bonded porcelain laminate veneers of an immediately placed implant in unintentional root proximity. The implant proximity to the adjacent root of the left lateral incisor was noted radiographically due to the mesial divergence of the apex of the left lateral incisor. Due to the periapical radiograph being only a 2D representation of the actual situation and superimposition a possibility, the decision was taken to observe, even though the surgeon reported different tactile sensitivity during implant insertion. A cone-beam computed tomography (CBCT) scan was proposed to assess the 3D implant location, but the patient persistently refused due to her concerns regarding her pregnancy and for personal reasons, thereafter. Clinical case-series studies have reported on the outcomes of implants placed touching the tooth or root fragments, with conflicting results.5-9 The decision was made to not remove the implant and observe, which led to uneventful rehabilitation for the 2-year clinical and radiographic follow-up.
Due to the facial placement of the right central incisor implant, screw retention would lead to a facial screw-access channel, thus compromising the esthetic outcome. The right central incisor implant had been placed years ago without consideration of ideal 3D implant positioning.19 The decision was made to fabricate a screw-retained framework and subsequently bond porcelain veneers to the framework to enhance the esthetics and avoid the facial screw-access placement. A previous clinical report by Magne et al20 illustrated how to bond a veneer on an implant substructure for a single-crown scenario. A meta-analysis reported that increased adhesion could be expected after physicochemical conditioning of zirconia. When tested using macro- and micro-tensile tests, it was found that MDP-based resin cements tend to present better bonding results than those of other cement types.21 In regard to the bonding technique, the combination of chemical and mechanical pretreatment is crucial for achieving durable bonding to zirconia ceramics. The cement choice was not revealed as a determining factor affecting the bond quality after aging conditions.21 In the present treatment, a self-adhesive resin cement was used for the bonding procedure. A limitation of the present clinical report is the short follow-up. More clinical studies are required before the above protocol can be routinely used.
A combination of surgical and prosthodontic techniques was used for the management of this case, namely root submergence and pink gingival ceramics. The root-submergence technique was used for the pontic site and facilitated the maintenance of alveolar-ridge volume, enhancing the symmetry in the lateral incisor areas and maintaining horizontal (buccal) contours.12 The submergence was performed to maintain horizontal contours, not vertical height. Papilla was lost regardless and was replaced with the pink porcelain.
However, maintaining vertical height of the ridge was not possible, andhence the incorporation of pink gingival ceramics in the patient’s fixed prosthesis to achieve more harmonious tooth proportions was used as an alternative to extensive soft-tissue and/or GBR augmentation procedures.12
The rationale for using gingiva-shaded ceramics instead of GBR was that the patient had a low-to-moderate smile line, which had been assessed during the treatment-planning phase and subsequent implant-fixed provisionalization. Hence, the transition line between the patient’s own gingiva and prosthetic ceramic gingiva would not be obvious.
About the Authors
Catherine DeFuria, DMD
Clinical Instructor
Division of Postgraduate Prosthodontics
Tufts University School of Dental Medicine
Boston, Massachusetts
Hans-Peter Weber, DMD, Dr. Med. Dent.
Professor and Chairman
Division of Postgraduate Prosthodontics
Tufts University School of Dental Medicine
Boston, Massachusetts
Yukio Kudara, CDT, MDT
Technical Instructor and Chief Laboratory Technician
Division of Postgraduate Prosthodontics
Tufts University School of Dental Medicine
Boston, Massachusetts
Panos Papaspyridakos, DDS, MS, PhD
Assistant Professor
Division of Postgraduate Prosthodontics
Tufts University School of Dental Medicine
Boston, Massachusetts
Summary
The 2-year outcome after immediate implant placement in unintentional close proximity with the adjacent root is report. Although this approach cannot be recommended for routine use, under the limitations of the present case report, the outcome was acceptable. The definitive implant rehabilitation was done with a screw-retained monolithic zirconia framework and porcelain veneers bonded to the framework.
References
1. Morton D, Chen ST, Martin WC, et al. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int J Oral Maxillofac Implants. 2014;29(suppl):216-220.
2. Krennmair G, Seemann R, Weinländer M, et al. Implant-prosthodontic rehabilitation of anterior partial edentulism: a clinical review. Int J Oral Maxillofac Implants. 2011;26:1043-1050.
3. Tarnow D, Elian N, Fletcher P, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74(12):1785-1788.
4. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
5. Asscherickx K, Vande Vannet B, Wehrbein H, Sabzevar MM. Success rate of miniscrews relative to their position to adjacent roots. Eur J Orthod. 2008;30(4):330-335.
6. Kuroda S, Yamada K, Deguchi T, et al. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2007;131(suppl 4):S68-573.
7. Kim SH, Kang SM, Choi YS, et al. Cone-beam computed tomography evaluation of mini-implants after placement: is root proximity a major risk factor for failure? Am J Orthod Dentofacial Orthop. 2010;138(3):264-276.
8. Szmukler-Moncler S, Davarpanah M, Davarpanah K, et al. Unconventional implant placement part III: implant placement encroaching upon residual roots - a report of six cases. Clin Implant Dent Relat Res. 2015;17(suppl 2):e396-e405.
9. Langer L, Langer B, Salem D. Unintentional root fragment retention in proximity to dental implants: a series of six human case reports. Int J Periodontics Restorative Dent. 2015;35(3):305-313.
10. Kuchler U, von Arx T. Horizontal ridge augmentation in conjunction with or prior to implant placement in the anterior maxilla: a systematic review. Int J Oral Maxillofac Implants. 2014;29(suppl):14-24.
11. Thoma DS, Buranawat B, Hämmerle CH, et al. Efficacy of soft tissue augmentation around dental implants and in partially edentulous areas: a systematic review. J Clin Periodontol. 2014;41(suppl 15):S77-S91.
12. Papaspyridakos P, Amin S, El-Rafie K, Weber HP. Technique to match gingival shade when using pink ceramics for anterior fixed implant prostheses. J Prosthodont. 2016 Apr 1[Epub ahead of print].
13. Papaspyridakos P, Lal K. Computer-assisted design/computer-assisted manufacturing zirconia implant fixed complete prostheses: clinical results and technical complications up to 4 years of function. Clin Oral Implants Res. 2013;24(6):659-665.
14. Cheng CW, Chien CH, Chen CJ, Papaspyridakos P. Complete-mouth implant rehabilitation with modified monolithic zirconia implant-supported fixed dental prostheses and an immediate-loading protocol: a clinical report. J Prosthet Dent. 2013;109(6):347-352.
15. Mehra M, Vahidi F.Complete mouth implant rehabilitation with a zirconia ceramic system: a clinical report. J Prosthet Dent. 2014;112(1):1-4.
16. Altarawneh S, Limmer B, Reside GJ, Cooper L. Dual jaw treatment of edentulism using implant-supported monolithic zirconia fixed prostheses. J Esthet Restor Dent. 2015;27(2):63-70.
17. Venezia P, Torsello F, Cavalcanti R, D’Amato S. Retrospective analysis of 26 complete-arch implant-supported monolithiczirconia prostheses with feldspathic porcelain veneering limited to the facial surface. J Prosthet Dent. 2015;114(4):506-512.
18. Papaspyridakos P, Lal K. Simple technique to transfer occlusal vertical dimension and articulate a definitive implant cast for a full arch implant prosthesis. J Prosthet Dent. 2008;100(4):320-322.
19. Papaspyridakos P. Implant success rates for single crowns and fixed partial dentures in general dental practices may be lower than those achieved in well-controlled university or specialty settings. J Evid Based Dent Practice. 2015;15(1):30-32.
20. Magne P, Magne M, Jovanovic SA. An esthetic solution for single-implant restorations - type III porcelain veneer bonded to a screw-retained custom abutment: a clinical report. J Prosthet Dent. 2008;99(1):2-7.
21. Ozcan M, Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 2015;17(1):7-26.