Retrofitting a Crown Supporting a Removable Partial Denture Using “Biogeneric Copy” to Replicate Tooth’s Preoperative Condition
Dhaval Patel, DDS
Abstract:
When a crown that supports a removable partial denture (RPD) needs to be replaced, patients often balk at having to wait several weeks for laboratory production to be completed before receiving the new restoration. Moreover, the fit of the lab-produced unit may not always be satisfactory. CEREC® CAD/CAM technology provides a design method known as Biogenetic Copy, which allows a clinician to replicate the preexisting size, shape, and form of a tooth chairside. As this case report demonstrates, using this method to retrofit a crown under an existing RPD prosthesis can result in a predictable, accurate, durable, and esthetic same-day restorative solution.
Computer-aided design/computer-aided manufacturing (CAD/CAM) technology has brought significant benefit to the dental industry.1,2 It not only enables clinicians to deliver same-day restorations, but also allows them to “think outside the box” and perform procedures that in the past were extremely rare in dentistry. One such application is manufacturing a crown on a tooth that supports a removable partial denture (RPD).
It is quite common for dental patients to have partial dentures. When one of the teeth that is supporting the RPD needs a crown, it is often difficult for the dentist to convince the patient to have the RPD sent out to a laboratory for 2 to 3 weeks along with the final impression. Patients simply don’t want to be without their partial denture for that length of time. Additionally, there is no guarantee that the fit of the lab-made crown supporting the RPD will be precise. As many dentists can attest, the fit can be “hit or miss.” There may be instances when the partial denture does not adequately fit around the newly produced crown, requiring the patient to have to get a new RPD and causing significant distress and frustration.
A solution to this type of situation involves CEREC® (Sirona Dental, www.sirona.com) CAD/CAM technology. CEREC software provides a design method known as Biogeneric Copy, a technique with which the clinician can produce an exact replica of the preexisting size, shape, and form of the tooth to be restored. This technique is demonstrated in the following case report.
Case Report
A 68-year-old female patient presented with the chief complaint of sensitivity to cold and sweets on the upper right side of her dentition. Tooth No. 4 had an existing amalgam restoration with a mesial marginal ridge fracture (Figure 1). Radiographic evaluation was within normal limits. It was determined that this tooth needed a crown due to the fracture, recurrent decay, and the fact that it was supporting the removable partial denture. The RPD had a rest seat on the distal aspect of tooth No. 4 and two clasps on the buccal and lingual aspects of the same tooth (Figure 2 and Figure 3).
Prior to using CEREC technology, the author found that there were two major drawbacks to performing this procedure. First, patients were typically very reluctant to part with their partial denture for a 2- to 3-week period; they found it difficult to function without it, especially if the RPD involved anterior teeth. Second, the fit of the final restoration to the RPD was almost always problematic.
In the present case, the author was able to confidently tell the patient that he could make her crown that same day with, in his opinion and based on his experience, a material that was strong enough to support the partial denture and a fit that would rival what the laboratory could produce. After having options explained to her, which also took into consideration her desire for a limited timeframe for completion, the patient agreed to receive a CAD/CAM-generated that would be fabricated in the clinician’s office immediately using CEREC Omnicam (Sirona).
Tooth Preparation
Tooth No. 4 was prepared for a full-coverage crown. It is important to note that care should be taken to remove enough tooth structure in all areas of the tooth to allow adequate thickness of material for the new crown. If not enough tooth structure is removed, the software will give a minimal thickness warning, and adding any more material to what was copied could lead to adjustments that may result in an improper fit of the RPD around the restoration. This would defeat the purpose of this design method.
After completing the preparation, the RPD was placed back in the patient’s mouth to check the reduction and make sure there was enough room for the crown (IPS e.max®, Ivoclar Vivadent, www.ivoclarvivadent.com) (Figure 4).
Scanning and Designing Process
For this case, making a copy of the existing tooth (ie, via Biogeneric Copy) was chosen as the design method. Biogenetic Copy is one of the fabrication modes of CEREC Omnicam software. It allows the operator to duplicate exactly the morphology and contours of an existing tooth or restoration, including rests, by having the computer overlay the “before” and “prep” pictures of any tooth in the mouth.
Prior to tooth No. 4 being prepared for a crown, a scan of the tooth was taken along with the anterior teeth and placed in the folder called “Biogeneric Copy Upper.” After the tooth preparation was performed, tooth No. 4 was scanned again along with the anterior teeth and the scan placed in the folder called “Upper Arch.”
After margination and setting the insertion axis is done, the software brings the user to the step of the copy line. This step involves drawing a copy line around the tooth structure that is desired in the final restoration (Figure 5). In this case there was a rest seat on the distal aspect and Akers clasps on the buccal and palatal, so it was imperative that all of those surfaces were copied completely. The copy line was drawn accordingly, and all of these surfaces were copied (Figure 6). When the software proposes the final restoration, one can see how it reproduces everything inside the copy line to provide the clinician a restoration that is an exact replica of the preexisting tooth (Figure 7). At this time the clinician should resist the urge to change anything on the surfaces that will be in contact with any rests or clasps, as doing so could lead to adjustments and the RPD subsequently not fitting around the new restoration.
Material Selection
IPS e.max LT shade A2 was chosen to mill the crown.3 IPS e.max lithium-disilicate restorations offer excellent durability, featuring 360 MPa to 400 MPa of flexural strength.4,5 When fabricated to full contour, the monolithic structure is the most robust ceramic milled system tested to date.6,7 According to the manufacturer, the opalescence, translucency, and light diffusion properties of IPS e.max lithium disilicate were all designed to replicate natural tooth structure for beauty and undetectable restorations.8
Milling and Try-in
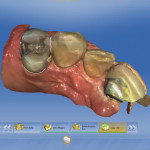
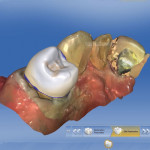
Using the CEREC inLab MC XL CAD/CAM milling machine (Sirona), it took approximately 6 minutes for the restoration to be milled. The sprue was removed and the restoration was tried in. Once the fit and occlusion were verified, the RPD was inserted to ensure proper fit around the new restoration. As can be seen in Figure 8 and Figure 9, the RPD fit the restoration in a manner that was identical to the way it fit the original tooth. After insertion, the restoration was finished and polished. At this point, it was in the blue stage and required a crystallization process to stain and glaze.
Staining, Glazing, and Cementation
In this case, it was noted during the planning stage that there was a definite change in chroma from the gingival to the incisal edge. The value shade of tooth No. 4 was A2 so this shade was selected. However, the gingival third was closer to A3; therefore, this third was stained with a darker A3 to achieve the gradation in color from the gingival third to the cuspal third.
Before bonding, the intaglio of the crown was etched with 4.5% hydrofluoric acid-etch for 20 seconds. The enamel at the margin was selectively etched for 15 seconds, washed, and dried. An adhesive resin dental cement (NX3 Nexus™, Kerr Dental, www.kerrdental.com) along with a self-etch, light-cure adhesive bonding system (OptiBond™ XTR, Kerr Dental) were used to cement the restoration. When the cement reached gel stage, the restoration was tack-cured for 2 seconds and excess cement was removed with an explorer. All surfaces were then light-cured for 20 seconds each. The proximal surfaces were flossed and any remaining cement was removed. Occlusion was checked and the margins were polished.
The RPD was then inserted, and it fit the same way as it fit around the original tooth and at the blue-stage try-in (Figure 10 and Figure 11). This fit was achieved without any adjustments on the milled restoration and was possible because of the Biogeneric Copy design method, which precisely duplicated the preoperative condition of the tooth.
Discussion and Conclusion
The CEREC Biogeneric Copy design method allows the clinician to achieve an exact copy of the preoperative condition of a tooth. An effective application for this design method is to use it to duplicate a tooth underneath a removable partial denture. In the author’s experience, patients have always been pleased to receive this kind of service and, as a result, have often become a good source of referrals for the practice. Retrofitting a crown under an existing removable partial denture prosthesis using chairside CEREC CAD/CAM technology has been shown to be predictable, accurate, durable, and esthetic.9-11 Being able to achieve this “same-day” with the CEREC Omnicam scanning process can be a pleasurable experience for the practitioner while, more importantly, serving the needs and wants of patients.
Disclosures
The author had no disclosures to report.
About the Author
Dhaval Patel, DDS
Faculty Member for Anterior and Posterior CEREC® CAD/CAM, and Advisory Board Member, PDS Institute, Irvine, California; Private Practice, Roseville, California
References
1. Poticny DJ, Klim J. CAD/CAM in-office technology: innovations after 25 years for predictable, esthetic outcomes. J Am Dent Assoc. 2010;141 suppl 2:5S-9S.
2. Shenoy A, Shenoy N. Dental ceramics: An update. J Conserv Dent. 2010;13(4):195-203.
3. McLaren EA, Chang Y. The 3D communication of shade: visual shade taking and the use of computerized shade-taking technology. Inside Dentistry. 2006;2(1):92-93.
4. Leung BT, Tsoi JK, Matinlinna JP, Pow EH. Comparison of mechanical properties of three machinable ceramics with an experimental fluorophlogopite glass ceramic. J Prosthet Dent. 2015;114(3):440-446.
5. Giordano R. Materials for chairside CAD/CAM-produced restorations. J Am Dent Assoc. 2006;137 suppl:14S-21S.
6. Guess PC, Vagkopoulou T, Zhang Y. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J Dent. 2014;42 (2):199-209.
7. Lin WS, Ercoli C, Feng C, Morton D. The effect of core material, veneering porcelain, and fabrication technique on the biaxial flexural strength and weibull analysis of selected dental ceramics. J Prosthodont. 2012;21(5):353-362.
8. IPS e.max® Lithium Disilicate. Ivoclar Vivadent website. https://www.ivoclarvivadent.us/emaxchangeseverything/lithium-disilicate/index.php. Accessed November 23, 2015.
9. Helvey GA. Retro-fitting an existing crown adjacent to a removable partial denture in a single visit. Inside Dentistry. 2009;5(3):34-41.
10. Marchack BW, Chen LB, Marchack CB, Futatsuki Y. Fabrication of an all-ceramic abutment crown under an existing removable partial denture using CAD/CAM technology. J Prosthet Dent. 2007;98(6):478-482.
11. Schoenbeck P. Retro-fitting a CEREC crown to a removable partial denture. Dent Today. 2008;27(3):110,112-113.