Post-Traumatic Treatment of Maxillary Incisors By Immediate Dentoalveolar Restoration with Long-Term Follow-Up
Abstract:
Replacing both missing maxillary anterior teeth is particularly challenging, especially in compromised sockets. This case report describes the management of an 18-year-old female patient, who suffered avulsion of both maxillary central incisors at 7 years of age. This multidisciplinary implant technique, called Immediate Dentoalveolar Restoration (IDR), included extraction of the injured teeth and a single procedure for immediate implant placement and restoration of the compromised sockets after root fracture and periapical lesion development were detected during orthodontic treatment. Successful esthetic and functional outcomes and reestablishment of the alveolar process after bone reconstruction were observed during the 3-year follow-up period. The predictable esthetic outcomes and soft- and hard-tissue stability that can be achieved following IDR are demonstrated.
Clinical studies have demonstrated that 16% to 30% of children and adolescents experience multiple events of dental alveolar trauma.1 Usually occurring in the maxillary anterior teeth, dental traumatic events can lead to esthetic, functional, and phonetic problems.2 Partial or complete root fracture can be a significant complicating factor in traumatic dental injuries.3 Whereas the prognosis is generally favorable for a vertical root fracture,3 bone loss may occur in the case of longitudinal root fracture due to the spread of bacteria and damage of the periodontal tissues.4
Longitudinal root fractures are a main cause of complications after endodontic therapy.2 Removing the root has been suggested.5 Quick decision-making is mandatory to stop rapid bone loss once the fracture communicates with the oral environment. The prognosis depends on the timing and surgical approach, residual bone volume, amount of buccal bone wall available to support the facial mucosa, and presence of residual infection.6 In some cases, the socket may be compromised, usually with loss of the buccal bone wall, which is important for the stability of soft-tissue contour in the esthetic zone.6-8
The aim of this long-term follow-up report is to suggest the use of a surgical-periodontal/implant technique—Immediate Dentoalveolar Restoration (IDR)—as an alternative to orthodontic forced eruption for treating bone defect problems in the esthetic area around a fractured tooth. The case is depicted in Figure 1 through Figure 17.
Clinical Report
Preoperative Information
An 18-year-old female patient referred to the dentistry clinic at the University of Sagrado Coração (Bauru, São Paulo, Brazil) showed a root fracture of the maxillary right central incisor. The patient had a history of avulsion of both maxillary central incisors at 7 years old, both of which were reimplanted. When the patient was 10 years old, endodontic necrosis was diagnosed during orthodontic treatment. Reduction of the pulp chambers was observed at the reimplanted incisors, and endodontic treatment was performed. Following endodontic treatment of teeth Nos. 8 and 9, the patient was monitored, and orthodontic treatment was performed over the course of 4 years. There was a history of abscesses and drainage in the buccal pathway in the apical region of tooth No. 8, which caused bone loss in the buccal wall region of this tooth. During this period, endodontic retreatments of teeth Nos. 8 and 9 were attempted twice, but without success.
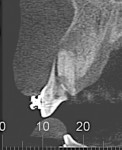
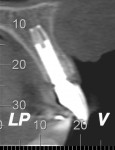
When the patient was 18 years old, root fracture of tooth No. 8 occurred, which was an indication for extraction (Figure 1 and Figure 2). Six months later, tooth No. 9 was also designated for extraction due to recurrent periapical lesions (Figure 4 and Figure 5). The following treatment plan was established: extraction of teeth Nos. 8 and 9 and performance of IDR at two different times (Figure 3 through Figure 11); placement of two ceramic abutments and all-ceramic crowns (Figure 12 through Figure 15); and continued orthodontic treatment to finalize the case.
Surgical and Prosthodontic Treatments
The patient was administered 1g of amoxicillin and 8 mg of dexamethasone 1 hour before surgery. She was instructed to rinse her mouth with 0.12% chlorhexidine solution for 30 seconds immediately before surgery. Local anesthesia was administered. The tooth, No. 8, was removed as atraumatically as possible by periotomes, with care taken to maintain the integrity of the remaining bone walls and papillae. Afterwards, the socket was checked and carefully curetted to remove the granulation tissue and remaining periodontal connective tissue.
Immediate implant placement was performed through 3-dimensional (3-D) positioning of the implant, as described by Buser et al.9 Measurements from the most apical bone level to the defect socket and the mesio-distal defect socket were assessed to determine the anatomical shape of the defect. After primary stability of the implant was confirmed (> 35 Ncm), a provisional crown was placed by using veneers that were previously created with a light-curing resin. The ideal emergence profile was established on the provisional prosthesis. Free space was maintained to accommodate the soft tissues, promote a thicker and more stable future gingival tissue margin on the implant, and improve the gingival contour.
Infiltrative anesthesia of 2% mepivacaine with norepinephrine was performed in the maxillary tuberosity, specifically through a crestal incision made at the center of the edge of the maxillary tuberosity, behind the distal face of the last molar. The incision was deepened along the entire length of the incision until the bone tissue was scratched. There was no need for a relaxing incision due to the size of the access area available.
An appropriate chisel was selected to harvest the graft material. Specifically, the width of the chisel was chosen to be 2 mm greater than the width of the bone defect to be reconstructed. The cortico-cancellous bone graft harvested from the donor region was manipulated to reproduce the shape of the socket defect using a rounger. The bone sliver was carefully adapted, with the cortex turned toward the buccal direction, achieving primary stabilization of the graft. The IDR technique was previously described in detail by Rosa et al.10 The gaps were completely filled with bone marrow harvested from the tuberosity to achieve secondary stabilization of the graft. The provisional crown was installed onto the implant, and the donor region was sutured with simple stitches.
Postoperatively, the patient received 500 mg of amoxicillin (three times a day for 7 days) and 4 mg of dexamethasone (once a day for 3 days), and was advised to rinse her mouth carefully with chlorhexidine solution (twice a day for 14 days).
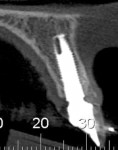
The same procedure was used for tooth No. 9. Six months after the second procedure, definitive restorations fabricated from zirconia-ceramic were placed for both central incisors. The patient was clinically and radiographically followed every 6 months. Figure 12 through Figure 15 show the occlusal and buccal clinical aspect at 3 years follow-up, and Figure 16 and Figure 17 show the tomographic follow-up of the buccal plate bone.
Discussion
Immediate loading after tooth extraction in a region with undamaged support tissue is a well-established approach in the literature.11,12 Preventing bone loss and maintaining gingival esthetics are factors that impact the success of immediate implant placement.13,14 Clinicians rate immediate implant placement in compromised sockets as either advanced or complex in terms of its difficulty level.15 The goal of this case report was to demonstrate that esthetically pleasing soft- tissue contours can be achieved and mucosal recession prevented through a single surgical rehabilitation of a central incisor root fracture with a compromised socket.
Although a conservative approach may be used to preclude extraction of the fractured tooth, the prognosis of teeth with root fractures, especially vertical root fractures, is often poor.2 Therefore, a dental implant is considered the treatment of choice.2,16 However, the fresh socket after tooth extraction should be carefully evaluated before implant placement. Root fracture and possible contamination of gaps in a root fracture may lead to relatively rapid bone resorption, depending on the type, extent, and duration of the fracture.2
Some clinical studies have evaluated the success of immediate implants after the extraction of vertically fractured teeth, reporting similar survival rates compared to implants placed in healed sites.11 However, immediate implant placement after the extraction of a vertically fractured tooth may be challenging due to the presence of bone defects, infection, and/or inflammation. Implants have been successfully placed in infected sites without severe complications when thorough socket debridement was performed.2,11,12 The level of bone support and dimensions of the surrounding soft tissue are key factors in determining the esthetic outcome of the implant restoration.
Another determining factor for functional and esthetic success in managing complicated crown-root fractures is adopting a multidisciplinary approach involving surgery, periodontics, prosthodontics, endodontics, and orthodontics.1 Some treatment alternatives are available to restore bone loss in compromised sockets, such as delaying implant placement to achieve soft-tissue healing, ridge preservation and augmentation with a block bone graft, guided bone regeneration, and forced orthodontic eruption. However, the esthetic outcomes of these techniques are questionable. An alternative to soft- and hard-tissue augmentation is forced orthodontic eruption before implant placement, based on osteophysiologic and orthodontic principles.2 The increase in bone volume is related to the tension applied to the periodontal ligament during orthodontic treatment, which induces the deposition of new bone via osteoblastic activity where the periodontal attachment exists.5 This technique has several advantages, such as correcting isolated infra-bone defects, repositioning the gingival margin, and clinical crown lengthening. However, the orthodontic forced-eruption step increases the overall treatment time.
The present case report described an alternative technique for restoring bone defects after root fracture using a maxillary tuberosity bone graft associated with immediate implant placement in a single procedure through the IDR concept. This choice presented several advantages, such as reduced treatment time, high predictability, and excellent esthetic outcomes. According to some clinical studies, immediate and early post-extraction implants may help to maintain soft-tissue stability to achieve a satisfactory esthetic outcome.11,12,17
In the IDR approach, the bone defect is restored with autogenous bone from a maxillary tuberosity bone graft, which contains osteoprogenitor cells from the periosteal and endosteum cells of the maxillary tuberosity.18 The graft is easy to harvest and adapt to the receptor region due to the bone malleability.18 In addition to restoring the lost buccal bone plate, the bone graft impedes cell competition between the hard and soft tissues, thereby promoting effective bone and gingival healing. The trabecular nature of grafts harvested from the maxillary tuberosity suggests that such grafts have high revascularization capacity and release growth factors to the receptor site.19,20 Hence, these grafts must be transported rapidly to prevent the loss of their fundamental properties. However, the maxillary tuberosity also presents some disadvantages in terms of the limited quantity of available bone and difficulty of surgical access.18
Conclusion
Implant placement in esthetic areas, especially in compromised sockets, should be carefully evaluated and a treatment plan made quickly to prevent bone loss. In this case report, use of the IDR technique resulted in predictable esthetic outcomes and soft- and hard-tissue stability.
About the authors
Ariádene Cristina Pértile de Oliveira Rosa, DDS, MSc
PhD Student in Oral Implantology, Department of Implantology, São Leopoldo Mandic Dental Research Center, Campinas/SP, Brazil
Carlos Eduardo Francischone, DDS, MSc, PhD
Full Professor, Department of Implantology, São Leopoldo Mandic Dental Research Center, Campinas/SP, Brazil
Mauricio de Almeida Cardoso, DDS, MSc, PhD
Full Professor, Department of Orthodontics, University of Sagrado Coração, Bauru, São Paulo, Brazil
Ana Carolina Alonso, DDS
Student, University of Sagrado Coração, Bauru, São Paulo, Brazil
Leopoldino Capelozza Filho, DDS, MSc, PhD
Full Professor, Department of Orthodontics. University of Sagrado Coração, Bauru, São Paulo, Brazil
José Carlos Martins da Rosa, DDS, MSc, PhD
PhD in Oral Implantology, Department of Implantology, São Leopoldo Mandic Dental Research Center, Campinas/SP, Brazil
References
1. Sharma D, Garg S, Sheoran N, et al. Multidisciplinary approach to the rehabilitation of a tooth with two trauma episodes: systematic review and report of a case. Dent Traumatol. 2011;27(4):321-326.
2. Oz IA, Haytaç MC, Toroglu MS. Multidisciplinary approach to the rehabilitation of a crown-root fracture with original fragment for immediate esthetics: a case report with 4-year follow-up. Dent Traumatol. 2006;22(1):48-52.
3. Corbella S, Taschieri S, Samaranayake L, et al. Implant treatment choice after extraction of a vertically fractured tooth. A proposal for a clinical classification of bony defects based on a systematic review of literature. Clin Oral Implants Res. 2014;(25)8:946-956.
4. Yang SF, Rivera EM, Walton RE. Vertical root fracture in nonendodontically treated teeth. J Endod. 1995;21(6):337-339.
5. Amato F, Mirabella AD, Macca U, Tarnow DP. Implant site development by orthodontic forced extraction: a preliminary study. Int J Oral Maxillofac Implants. 2012;27(2):411-420.
6. Pieri F, Aldini NN, Marchetti C, Corinaldesi G. Esthetic outcome and tissue stability of maxillary anterior single-tooth implants following reconstruction with mandibular block grafts: a 5-year prospective study. Int J Oral Maxillofac Implants. 2013;28(1):270-280.
7. De Rouck T, Collys K, Cosyn J. Immediate single-tooth implants in the anterior maxilla: a 1-year case cohort study on hard and soft tissue response. J Clin Periodontol. 2008;35(7):649-657.
8. Fagan MC, Owens H, Smaha J, Kao RT. Simultaneous hard and soft tissue augmentation for implants in the esthetic zone: report of 37 consecutive cases. J Periodontol. 2008;79(9):1782-1788.
9. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(7 spec suppl):43-61.
10. da Rosa JC, Rosa AC, da Rosa DM, Zardo CM. Immediate Dentoalveolar Restoration of compromised sockets: a novel technique. Eur J Esthet Dent. 2013;8(3):432-443.
11. Caiazzo A, Brugnami F, Mehra P. Buccal plate preservation with immediate post-extraction implant placement and provisionalization: preliminary results of a new technique. Int J Oral Maxillofac Surg. 2013;42(5):666-670.
12. Cabello G, Rioboo M, Fábrega JG. Immediate placement and restoration of implants in the aesthetic zone with a trimodal approach: soft tissue alterations and its relation to gingival biotype. Clin Oral Implants Res. 2013;24(10):1094-1100.
13. Buser D, Halbritter S, Hart C, et al. Early implant placement with simultaneous guided bone regeneration following single-tooth extraction in the esthetic zone: 12-month results of a prospective study with 20 consecutive patients. J Periodontol. 2009;80(1):152-162.
14. Huynh-Ba G, Pjetursson BE, Sanz M, et al. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implant Res. 2010;21(1):37-42.
15. Buser D, Chappuis V, Bornstein MM, et al. Long-term stability of contour augmentation with early implant placement following single tooth extraction in the esthetic zone: a prospective, cross-sectional study in 41 patients with a 5- to 9-year follow-up. J Periodontol. 2013;84(11):1517-1527.
16. Wang HL, Shotwell JL, Itose T, Neiva RF. Multidisciplinary treatment approach for enhancement of implant esthetics. Implant Dent. 2005;14(1):21-29.
17. De Rouck T, Collys K, Cosyn J. Single-tooth replacement in the anterior maxilla by means of immediate implantation and provisionalization: a review. Int J Oral Maxillofac Implants. 2008;23(5):897-904.
18. Cicconetti A, Sacchetti B, Bartoli A, et al. Human maxillary tuberosity and jaw periosteum as sources of osteoprogenitor cells for tissue engineering. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(5):618.
19. Prolo DJ, Rodrigo JJ. Contemporary bone graft physiology and surgery. Clin Orthop Relat Res. 1985;200:322-342.
20. Goldberg VM, Stevenson S. Natural history of autografts and allografts. Clin Orthop Relat Res. 1987;225:7-16.