Titanium-Reinforced Interdental Peaks As a Simple Method for Papilla Preservation
Abstract:
Esthetic failure within the esthetic zone can be caused by the presence of interdental black triangles due to the loss of interdental papillae. The position of the osseous crest represents the main determinant for the papilla height, and, therefore, interdental bone peaks should be preserved both during and following dental treatment. Osseointegrated titanium implants maintain bone levels at the site where they have been inserted, even when left non-loaded. This property of osseointegrated titanium implants can be applied to preserve interdental bone peaks. The technique described in this case report illustrates how small titanium bars were surgically inserted within the interdental osseous peaks in order to prevent bone resorption and maintain papilla height. Clinical measurements between a fixed reference point and the papilla tips were performed over a 12-month period. A positive gingival architecture was created and maintained even following multiple tooth extractions in the esthetic zone.
The esthetic appearance of a natural or restored smile is the result of the balance that exists between the gingival and dental components.1-3 In a condition of oral health, which is the most esthetically pleasing, the relationship between these two components produces gingival extensions or offshoots between adjacent teeth. These extensions, the interdental papillae, convey a festooned appearance to the gingival component. In periodontal healthy conditions, when the distance from the osseous crest to the contact point between adjacent teeth is 4 mm or less and the interproximal distance between adjacent roots is 2 mm or less, the tip of the interdental papillae completely fills the interdental space.4
Conversely, the absence of interdental papillae in a smile may be a sign of a pathological condition and causes the formation of interdental “black triangles” or “black holes.”5 Interdental black triangles not only deface the smile, but they also create discomfort for the patient by causing: food and bacterial plaque entrapment at the interdental spaces; altered speech due to air flowing in between open interdental spaces; and/or passage of saliva through open interdental spaces during speech.
The gingival and the interdental papillae do not have a predetermined shape, but resemble the shape and configuration of the underlying bone. Therefore, in order to have a festooned appearance of the gingiva (presence of interdental papillae), it is necessary to have a festooned anatomy of the underlying bone, resulting in interdental osseous peaks. When there are pathological conditions (periodontal disease) or following dental procedures, the bone resorbs, loses its festooning, flattens out, and recedes—even the gingiva flattens out and recedes, losing the interdental festooning and, therefore, the papillae. As a result, the teeth appear longer, root portions uncover, and interdental black triangles become evident.
The main interdental papillae height determinant is represented by the underlying bone crest (osseous peaks),4,6-8 which plays a fundamental role.9,10 It is, therefore, of utmost importance to prevent iatrogenic resorption of the interdental osseous peaks. Interdental bone resorption can occur due to procedures such as tooth extraction (single or multiple), substitution of missing teeth by means of dental implants (single or multiple), and periodontal surgery, as well as uncontrolled restorative steps (ie, tooth preparation) causing biologic width encroachment.
In the scientific literature, long-term predictable techniques for the preservation of interdental osseous peaks and papillae are not available, even though special emphasis has been frequently been placed on this subject. Authors have suggested specific surgical techniques aimed at reconstructing the papillae,8,11 sophisticated surgical procedures for the preservation or for the regeneration of the papillae with questionable short-term success,12,13 injections of hyaluronic gel to treat papillae deficiencies,14 meticulous preservation of interdental bone peaks through atraumatic dental procedures,15 and avoidance of the papillae during surgical procedures when possible, in order to prevent undesired retractions.16-18 At the current time, the preservation of interdental bone peaks, and, therefore, of the papillae, through the surgical insertion of a biocompatible material has not been described.
Paradigm Shift
Substituting a missing tooth with a titanium implant represents a successful technique made possible by the high compatibility of pure titanium and its alloys with bone. Several weeks after surgical placement, the bone–metal interface matures, leading to the process defined as osseointegration,19,20 which conveys stability to the implant, which can then be restored. Implants placed in the jaws of patients who have lost their teeth not only allow for the insertion of artificial teeth anchored to the bone, but also avoid further bone resorption over time at the site where they have been placed, even when left non-loaded. A retrospective, clinical, split-mouth study reported that submerged non-loaded implants showed less bone loss than their neighboring functional implants over a period of 12 years.21 Well-functioning, non-loaded fixtures can be observed routinely in patients restored with maxillofacial prostheses retained by extraoral implants, and the reported survival rates are high.22,23 This important characteristic of commercially pure (CP) titanium, its alloys, and other biocompatible materials (ie, zirconium) could be used to prevent the resorption of interdental bone peaks.
Technique and Armamentarium
The titanium-reinforced interdental peaks (TRIP) system requires the surgical insertion of bars made of any biocompatible material, such as titanium (pure or alloy), within the thickness of interdental bone. Ideally, the surgical insertion should be performed before any dental procedure that may cause interdental osseous peak resorption (eg, tooth extraction, implant placement, periodontal surgery, etc). Following insertion, the biocompatible bar osseointegrates, preserving the original height of the interdental bone peaks over time.
Once the osseointegration process of the bar is completed, the pre-planned dental procedure such as tooth extraction and implant placement can proceed, with reduced risk for interdental peak resorption followed by retraction of the papilla. Depending on the clinical situation, an immediate protocol may be used as well, for which the planned dental procedure would be performed immediately after bar insertion and during the same appointment.
The size of the biocompatible bar can vary according to the size of the receiving interdental bone peaks. The prototype has the following dimensions: 0.5-mm width x 1-mm height x 5-mm length. Length, width, and height can all vary according to the indications.The armamentarium for the surgical insertion of the bars includes: piezosurgical unit or sonic handpieces and calibrated tips; caliper with the same dimensions of the bar, for the intra-operatory check of the osteotomy size; biocompatible bars; chisel for the deep insertion and primary stabilization of the bar; surgical mallet; and collagen resorbable membranes to cover the bone graft over the osteotomies.
Indications
The TRIP system can be used in both pre-extraction and post-extraction clinical situations. Four main indications can be described:
1) Preservation of interdental bone peaks between multiple ovate pontics (pre-extraction): Following an extraction (Figure 1[a]) a ridge defect is created with an incidence of 91%.24 The defect can be combined vertically and horizontally (55.8%), horizontally (2.9%), or vertically (32.8%). Therefore, conventional tooth extractions can cause flattening of the residual ridge with resorption of interdental bone (Figure 1[b]). Once the final prosthesis with multiple ovate pontics is inserted, the resorption of the interdental peaks occurring over time will cause the formation of black triangles (Figure 1[c]).
Using the TRIP system, biocompatible bars are surgically inserted within the osseous peaks before the extractions are done (Figure 1[d]). Following completion of the osseointegration process, or during the same appointment (immediate protocol), the teeth are extracted. The biocompatible bars should prevent, as is the case with root-form titanium implants, the resorption of the interdental bone peaks (Figure 1[e]). Once the final prosthesis is delivered, the preservation of the interproximal bone height will prevent the formation of interdental black triangles by preserving the papilla (Figure 1[f]).
2) Preservation of interdental bone peaks between adjacent implants (pre-extraction): When replacing extracted teeth with adjacent implants, the bone loss (ridge deformity) caused by the extractions (Figure 2[a and b]) will be increased by the bone loss caused by the presence of the fixtures. A 1.5-mm lateral component to bone loss is usually recorded around each implant.25 Therefore, an inter-implant distance lower than 3 mm will cause the flattening of the inter-implant bone (osseous peak), resulting in the formation of interdental black triangles due to the loss of the interdental papillae (Figure 2[c]).
With the TRIP system, as described in the first indication, biocompatible bars are surgically inserted within the osseous peaks before the extractions are done (Figure 2[d]). Following completion of osseointegration, or during the same appointment (immediate protocol), the teeth are extracted, while the biocompatible bars should prevent the resorption of the interdental bone peaks (Figure 2[e]). The implants can then be placed according to either an immediate or delayed protocol, while the biocompatible bars should counteract the lateral component of bone loss occurring around each implant, preserving the interdental papillae and preventing the formation of interdental black triangles (Figure 2[f]).
3) Preservation of interdental bone peaks between teeth and implants (pre-extraction): Interdental bone loss following the placement of a single implant adjacent to natural teeth is not as critical as it is in other clinical conditions if socket preservation and atraumatic extraction techniques are used to prevent or reduce alveolar bone resorption that would subsequently lead to morphological changes of the post-extractive ridge.26 In such clinical situations, interdental bone peak height is usually maintained by the presence of the adjacent natural teeth, and the preserved bone peaks are responsible for stabilizing the position of interdental soft tissues.27 Nevertheless, after extraction of a tooth, some bone loss (ridge deformity) can still occur, causing an interdental black triangle formation due to soft-tissue retraction once the single implant is restored.8,28 Clinical observations have confirmed that soft-tissue retraction is even more pronounced in conditions of thin versus thick soft-tissue phenotype.27
Similar to the two previous indications, with the TRIP system biocompatible bars are surgically inserted within the osseous peaks before the extraction of the tooth. Following completion of osseointegration, or during the same appointment (immediate protocol), the tooth is extracted and the biocompatible bars should prevent the resorption of the interdental bone peaks. The implant can then be placed, according to either an immediate or delayed protocol, while the biocompatible bars should counteract the lateral component of the bone loss around the fixture, preserving the interdental papillae and preventing the formation of an interdental black triangle.
4) Preservation of iatrogenic interdental bone peaks created for multiple ovate pontics, or adjacent implants, site development (post-extraction): In edentulous ridges, flattening of both osseous and gingival architecture is observed (Figure 3[a]). In order to create the illusion of interdental papillae in combination with ovate pontics or adjacent implants, the clinician might recontour the soft tissue and underlying bone with a bur29 (Figure 3[b]). Then, a provisional fixed partial denture is relined in direct contact with the newly shaped ridge until complete healing occurs or implants are surgically inserted. Once the final multiple ovate pontics or implant-supported restoration is delivered, the iatrogenic interdental osseous peaks may resorb over time, causing the retraction of the interdental papillae and the formation of interdental black triangles (Figure 3[c]).
Again, using the TRIP system, biocompatible bars are first inserted surgically within the bone of the edentulous ridge according to the desired position of the new papillae (Figure 3[d]). Following completion of the osseointegration process, or during the same appointment (immediate protocol), the clinician then recontours the ridge so that the provisional can be relined or the implants can be inserted (Figure 3[e]). Once the final restoration is delivered, the biocompatible bars should prevent the resorption of the newly formed osseous peaks over time, preventing the formation of interdental black triangles by preserving the interdental papillae (Figure 3[f]).
Case Report
A 68-year-old woman was treated for severe localized adult periodontitis affecting the esthetic zone. Her chief complaint was the presence of spaces between her teeth and the unpleasant shape of the anterior maxillary dentition. The periodontal disease had disrupted the osseous and gingival architecture, causing tooth migration, supraeruption, mobility, flaring, and diastemas (Figure 4). Periapical radiographs showed severe bone loss and an unfavorable crown-to-root ratio (Figure 5).
The treatment plan consisted of extracting four maxillary incisors and replacing them with a fixed partial denture with four ovate pontics. The challenge involved recreating the osseous-gingival architecture where it was lost and preserving it where it was still present. In order to meet that goal, the TRIP system was used. No medical and dental contraindications were present. This pre-extraction clinical situation represented a Type 1 indication.
Diagnostic Phase
In order to correct the supraeruption of the maxillary incisors, an esthetic template (vacuum-formed) with tooth-colored acrylic resin (Jet Kit, Lang Dental Manufacturing Co., Inc., www.langdental.com) was fabricated to assess the correct incisal edge position in the face of the patient. The information was then transferred to a modified mounted study cast in order to finalize a diagnostic wax-up. The modifications made to the study cast consisted of the simulation of the extractions and the shaping of the extraction sockets to reproduce ideal ovate pontic sites and restore a positive gingival architecture flattened by the periodontal disease (Figure 6 and Figure 7).
The diagnostic wax-up not only was used to fabricate the provisional restoration to be inserted intraorally after the extractions, but also provided spatial indications as to the positions (mesio-distally) of the five titanium bars, as indicated by the blue vertical lines drawn on the diagnostic cast (Figure 8).
Surgical Phase
An intrasulcular incision from teeth Nos. 5 through 12 was performed to expose the interdental bone. As shown in the radiographs (Figure 5), the osseous architecture had been flattened by the periodontitis.
A piezosurgical unit (Mectron s.p.a, www.mectron.com) and tips were used for the osteotomies. A special caliper with the shape and dimensions of the titanium bars was used to verify the size of the osteotomies. The titanium bars carried into place by pliers were seated into the sites (Figure 9) before being pushed deeply with a chisel and surgical mallet. As a result, all titanium bars obtained primary stability (Figure 10).
The sites were then covered with granulated osteoconductive material (Bio-Oss®, Geistlich Pharma AG, www.geistlich-na.com) and strips of resorbable membranes (Bio-Gide®, Geistlich Pharma AG). The flap was then sutured with a 4-0 Vicryl Plus thread (Johnson and Johnson Intl., www.jnj.com).
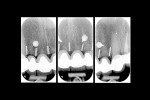
Following the insertion of the titanium bars, intraoral radiographs were taken to verify the correct positioning (Figure 11).
Extractions and Provisionalization
Three months after insertion of the interdental titanium bars, the maxillary incisors were extracted. A provisional fixed partial denture with four ovate pontics was relined into the extraction sockets grafted with osteoconductive material (Bio-Oss), and inserted.
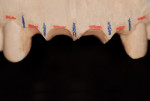
Two weeks after the extractions, the gingival component had already regained a sharp positive architecture (Figure 12). The challenge would have been preserving it over time.
Data Recording
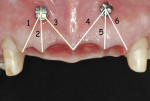
One month after the extractions with insertion of the provisional fixed partial denture, measurements were recorded to assess changes in papilla height over time. Two orthodontic transcortical titanium screws (Spider Screw®, Ortho Technology, www.orthotechnology.com) were symmetrically inserted apically between teeth Nos. 7-8 and 9-10, respectively. These screws served as reference points. The distance was measured with a digital caliper (Mitutoyo America Corp., www.mitutoyo.com) from the center of the head of the spider screw to the tip of each papilla (Figure 13).
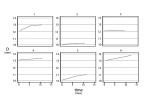
Distances (D) were measured in six different locations at 1 month (baseline-T0), 6 months from baseline (T1), and 12 months from baseline (T2) (Figure 14). All measurements began 5 minutes after removal of the provisional fixed partial denture. Each value was the mean of three measurements for each papilla made by three different blind operators. Mean distances (D) are reported in Table 1.
An estimated panel linear regression model was created with fixed effects, where the mean papilla height (D) was regressed over time to identify the presence of either a decreasing or increasing trend. The model was estimated by grouping the observations into the six different locations (Table 1), disregarding location 3 because it was highly correlated with location 4. Model estimates showed a significant (P value = 0.001) and positive regression coefficient (coefficient = .0497) for the variable time, indicating an increasing trend over a 12-month interval (growth of the papilla). This increasing trend is also evident from the data depicted in Figure 15.
The same model was also estimated by disregarding location 4 instead of 3. The results were similar (P value = 0.004, coefficient = .0453) and reached the same conclusions.
This analysis, being based on a small sample of observations on a single individual, had only a descriptive meaning and the results were encouraging, but no definitive conclusions can be drawn from it.
After the first 12-month data collection, radiographic and clinical follow-up with measurements taken from the fixed reference points were carried out up to 24 months, when the cortical screws were removed. Data recorded at 24 months (distance [D]) were comparable to those recorded at 12 months with no changes in papilla height.
Radiographic Control
Radiographic evaluation of the titanium bars before the extractions and at 6 and 12 months after the extractions did not show significant changes (Figure 16).
Restorative Phase
Final impressions were made to create a master model. The ovate pontic sites were refined and shaped in the stone to reproduce ideal gingival contours. Particular attention was paid with respect to the interdental spaces occupied intraorally by the titanium bars (interdental peaks).
A final wax-up was cut back to fabricate the metal framework that was tried intraorally before being layered with porcelain. The porcelain ovate pontic profiles were built up to be convex in all directions and highly polished. The final fixed partial denture was tried in the mouth to verify the intensity of the pressure exerted over the ovate pontic sites (Figure 17).
Soft-tissue blanching was temporarily observed while the patient was biting over cotton rolls. Interdental floss could pass underneath the pontics smoothly without resistance, and it was decided to proceed with the final cementation (Figure 18). Postoperative radiographic control showed a correct interdental positioning of the bars and absence of bone resorption (Figure 19).
Discussion
The TRIP system is based upon the same biological principles that are the foundation of modern implant dentistry. A few weeks after surgical placement, bone and titanium will establish a contact leading to osseointegration of the bars.19,20 In order to increase the bone–metal contact surface, the bars can be roughened according to different surface treatment techniques already available and used for root-form implants.
The role of the TRIP system is that of preserving the interdental bone from resorption. This property of titanium (as a biocompatible material) can be observed routinely for non-loaded extraoral implants supporting maxillofacial prostheses (eg, ear prostheses).22,23 In those clinical conditions, a transdermal implant component creates a communication between the endosseous implant (body), the bone crest, and the external environment. Intraorally, transmucosal components of dental implants (implant collar or abutment) create a communication between the implant and the oral flora. The microgap at the implant head–abutment interface can therefore accumulate bacterial plaque, which may cause inflammation.30,31 The latter might lead to complications. Conversely, with the TRIP system, the bars are meant to be inserted in a closed environment, unexposed. This submerged status presents a more favorable condition for the long-term preservation of osseointegration.
If the tip of an interdental bar should become exposed over time, it would still be useful in supporting the papilla, acting as a soft-tissue scaffold, and being tissue friendly and well tolerated, as is observed for titanium transmucosal root-form implant components.
In the patient situation presented here, the flap was raised generously because multiple periodontally involved sites were being impacted by the titanium bars’ insertion. On the other hand, the surgical technique for the placement of the inserts can be minimally invasive, especially for a periodontally healthy patient. Given the small dimensions of the bar, the insertion can be performed by only raising the buccal half of the papilla tip to the extent that the interdental osseous peak becomes exposed, or by creating a vertical incision along the length of the papilla and opening a vertical envelope flap to expose the bone.
The surgical insertion of the titanium interdental bars should ideally be at least 1-mm deep into the osseous peak thickness, or at least right below the buccal cortical plate, while the tip of the bar should be placed even with the highest point of the osseous peak. For that reason, the thickness of the bar should be kept to the minimum, allowing for a deep insertion of the bar without causing deformation. The bars used for this patient situation were 0.5-mm thick.
Clinically, the full thickness of an osseous peak can be assessed using a wax caliper and subtracting the buccal and palatal soft-tissue thickness, which is measured by sounding to bone with a periodontal probe. Once the bar is covered with a bone graft and a membrane, no grey discoloration of the soft interdental soft tissues should be detectable. The greyish color of the titanium could cause a discoloration problem if the titanium bar were to become partially exposed due to buccal bone resorption. For that reason, the use of white biocompatible inserts, such as zirconium bars, is being considered for clinical studies and clinical application.
For this patient, measurements were performed clinically with an electronic caliper from a fixed reference point to the papilla tips, and three blind operators performed each measurement three times. A more calibrated approach utilizing measurements made from standardized x-rays could have provided more accurate data and is, therefore, recommended for both future and ongoing studies with the TRIP system.
In this particular clinical situation, the baseline (T0) clinical measurement of the papilla height was established at 1 month after the iatrogenic creation of a new positive gingival architecture with ovate pontics. In fact, the preoperative gingival architecture had been already disrupted by the periodontal disease. In future studies, if conducted on patients with healthy papillae, the baseline (T0) papilla height should be recorded before tooth extractions. Nonetheless, the results showed not only the preservation over a 12-month period of what was achieved with the ovate pontics immediately after the extractions, but also some growth of the papillae, most likely due to the lateral compression exerted by the ovate pontics.6
In addition, for this patient the healing phase was characterized by the presence of a thick tissue phenotype, for which, at 1 year postoperative, the coronal displacement of the gingival margins was more pronounced.32
Following the removal of the cortical screws used as a fixed reference point, clinical-visual evaluation of papilla height for this patient continued up to 36 months through recall appointments scheduled every 3 months. No black triangles due to papilla retraction were noticed or recorded visually. Moreover, non-standardized routine radiographic examinations, normally used to monitor bone levels at root-form titanium dental implants, did not show appreciable bone loss around the interproximal titanium bars.
Several sophisticated techniques have been described in order to preserve alveolar bone—either buccal or interproximal. Some techniques advocated root extraction by drilling out tooth structure at the time of implant placement,15 others advocated the placement of titanium root-form implants either close to or in direct contact with retained root fragments.33 The TRIP system approach, utilizing sterile biocompatible inserts placed in healthy bone, appears to be less technique-sensitive and less exposed to the risk of infection.
Conclusions
Even though controlled prospective in-vivo investigations and more data are needed in order to demonstrate the long-term efficacy of the technique presented, the TRIP system, which is based upon the biological principles of osseointegration, may be a promising solution for the preservation of interdental papillae.
DISCLOSURE
Titanium bars were supplied free of charge by Bio Implant srl (Italy), www.bioimplant.it. An international patent is pending for the TRIP system presented in this article.
ACKNOWLEDGMENTS
The authors wish to thank Prof. Roberto Rocci, University of Rome-Tor Vergata, for his helpful advice on the data description presented in this paper.
ABOUT THE AUTHORS
Jacopo Castelnuovo, DDS, MSD
Affiliate Assistant Professor, Graduate Prosthodontics, University of Washington, School of Dentistry, Seattle, Washington; Private Practice, Rome, Italy
A. Burcin Sonmez, DDS, MSc
Resident, PhD Program, Department of Oral and Maxillofacial Sciences, University of Rome-La Sapienza, School of Dentistry, Rome, Italy; Private Practice, Rome, Italy
John C. Kois, DMD, MSD
Director, Kois Center, Seattle, Washington
REFERENCES
1. Rufenacht CR. Structural Esthetic Rules. Fundamentals of Esthetics. 1st ed. Chicago, IL: Quintessence Publishing Co Inc; 1990:127.
2. Frush JP, Fisher RD. The dynesthetic interpretation of the dentogenic concept. J Prosthet Dent. 1965;8(4):558-581.
3. Lombardi RE. The principles of visual perception and their clinical application to denture esthetics. J Prosthet Dent. 1973;29(4):358-382.
4. Cho HS, Jang HS, Kim DK, et al. The effects of interproximal distance between roots on the existence of interdental papillae according to the distance from the contact point to the alveolar crest. J Periodontol. 2006;77(10):1651-1657.
5. Sharma AA, Park JH. Esthetic considerations in interdental papilla: remediation and regeneration. J Esthet Restor Dent. 2010;22(1):18-28.
6. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
7. Chang LC. Factors associated with the interdental papilla height between two maxillary central incisors: a radiographic study. J Periodontol. 2012;83(1):43-49.
8. Choquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
9. van der Velden U. Regeneration of the inderdental soft tissues following denudation procedures. J Clin Periodontol. 1982;9(6):455-459.
10. Kois JC. Altering gingival levels: the restorative connection. Journal of Esthetic Dentistry. 1994;6(1):3-7.
11. Palacci P, Ericsson I, Engstrand P, Rangert B. Papilla regeneration technique. Optimal Implant Positioning & Soft Tissue Management for the Branemark System. Chicago, IL: Quintessence Publishing Co Inc; 1995:59-70.
12. De Castro Pinto RC, Colombini BL, Ishikiriama SK, et al. The subepithelial connective tissue pedicle graft combined with the coronally advanced flap for restoring missing papilla: a report of two cases. Quintessence Int. 2010;41(3):213-220.
13. Jaiswal P, Bhongade M, Tiwari I, et al. Surgical reconstruction of interdental papilla using subepithelial connective tissue graft (SCTG) with a coronally advanced flap: a clinical evaluation of five cases. J Contemp Dent Pract. 2010;11(6):49-57.
14. Becker W, Gabitov I, Stepanov M, et al. Minimally invasive treatment for papillae deficiencies in the esthetic zone: a pilot study. Clin Implant Dent Relat Res. 2010;12(1):1-8.
15. Yalcin S, Aktas I, Emes Y, et al. A technique for atraumatic extraction of teeth before immediate implant placement using implant drills. Implant Dent. 2009;18(6):464-472.
16. Takei HH, Han TJ, Carranza FA Jr, et al. Flap technique for periodontal bone implants. Papilla preservation technique. J Periodontol. 1985;56(4):204-210.
17. Cortellini P, Prato GP, Tonetti MS. The modified papilla preservation technique: A new surgical approach for interproximal regenerative procedures. J Periodontol. 1995;66(4):261-266.
18. Cortellini P, Prato GP, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Restorative Dent. 1999;19(6):589-599.
19. Albrektsson T, Jacobsson M. Bone-metal interface in osseointegration. J Prosthet Dent. 1987;57(5):597-607.
20. Meffert RM, Block MS, Kent JN. What is osseointegration? Int J Periodontics Restorative Dent. 1987;7(4):9-21.
21. Marcelis K, Vercuyssen M, Nicu E, et al. Sleeping vs. loaded implants, long-term observations via a retrospective analysis. Clin Oral Implants Res. 2012;23(9):1118-1122.
22. Wright RF, Zemnick C, Wazen JJ, Asher E. Osseointegrated implants and auricular defects: a case series study. J Prosthodont. 2008;17(6):468-475.
23. Karakoca S, Aydin C, Ylmaz H, Bal BT. Survival rates and periimplant soft tissue evaluation of extraoral implants over a mean follow-up period of three years. J Prosthet Dent. 2008;100(6):458-464.
24. Abrams H, Kopczyk RA, Kaplan AL. Incidence of anterior ridge deformities in partially edentulous patients. J Prosthet Dent. 1987;57(2):191-194.
25. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
26. Agarwal G, Thomas R, Mehta D. Postextraction maintenance of the alveolar ridge: rationale and review. Compend Contin Educ Dent. 2012;33(5):320-326.
27. Nisapakultorn K, Suphanantachat S, Silkosessak O, Rattanamongkolgul S. Factors affecting soft tissue level around anterior maxillary single-tooth implants. Clin Oral Implants Res. 2010;21(6):662-670.
28. Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of the interproximal papilla. J Periodontol. 2004;75(9):1242-1246.
29. Garber DA, Rosenberg ES. The edentulous ridge in fixed prosthodontics. Compend Contin Educ Dent. 1981;2(4):212-223.
30. Jansen VK, Conrads G, Richter EJ. Microbial leakage and marginal fit of the implant-abutment interface. Int J Oral Maxillofac Implants. 1997;12(4):527-540.
31. Subramani K, Jung RE, Molenberg A, Hammerle CH. Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants. 2009;24(4):616-626.
32. Pontoriero R, Carnevale G. Surgical crown lengthening: a 12-month wound healing study. J Periodontol. 2001;72(7):841-848.
33. Hürzeler MB, Zuhr O, Schupbach P, et al. The socket-shield technique: a proof-of-principle report. J Clin Periodontol. 2010;37(9):855-862.