The Use of 3-Dimensional Imaging in Dentoalveolar Surgery
Abstract
In the past decade, many different cone-beam volumetric tomography (CBVT/CBCT) machines have been introduced to the dental market with varying features. While medical-grade CT is still considered the “gold standard” for CT accuracy and diagnosis, CBCT, because of its convenience, lower radiation, and smaller machine footprints, has become more commonplace in dental surgical offices. This article discusses the use of CBCT technologies along with proprietary implant software programs in dentoalveolar surgery.
Dentists have traditionally used 2-dimensional (2-D) radiographic images (ie, bitewing, periapical, occlusal, panoramic, and cephalometric radiographs) to diagnose and treat patients. While doing so, they have needed to understand and work within the limitations of these technologies. For many years, oral and maxillofacial surgeons, based on their in-hospital training and experience in treating facial trauma and pathology, have used CT scan imaging for 3-dimensional (3-D) patient evaluation, but the visualization of these images was always in a 2-D format, printed on plain films or viewed in 2-D on a computer screen.
Historically, prior to the early 2000s, most CT scan imaging was performed in hospital-based or private radiology facilities on medical-grade helical CT scanners. Initially, these scanners were single-slice, slow-running machines. These technologies have advanced to the currently available multi-slice machines—128 or more slices per second—capable of scanning the heart between beats. Because of the lack of familiarity and comfort with hospital-based facilities, the lack of training in interpreting the images, and the perceived limited cost-benefit ratio considering the increased radiation of CT scans, these technologies were not widely adopted by the general dental community. In 1998, the NewTom 9000 (Quantitative Radiology [QR srl], www.qrverona.it) was the first machine specifically designed for dentistry that reported using cone-beam volumetric tomography (CBVT/CBCT).1 The machines were compact, easy to fit into the limited space of a dental office, and produced good 3-D images with lower radiation doses.2-4 However, because of the lower radiation, the images had somewhat less definition.
Since that time, many different CBCT machines have been introduced to the dental market by multiple manufacturers with varying features and costs. Medical-grade CT is still considered the “gold standard” for CT accuracy and diagnosis. Recently, adaptive statistical iterative reconstruction (ASIR) software products have been introduced that can allow up to a 50% reduction in the radiation dose of medical-grade CT scans while maintaining image quality.5-8 It is important to also understand that there are different average deviations for all CBCT scanners.9,10 This article discusses the use of these technologies along with proprietary implant softwares in dentoalveolar surgery; it is not a discussion of the differences between CBCT and medical-grade CT. This article will use the term “CT” synonymously for both CT and CBCT technologies. The choice of which technology to use is the decision of the treating clinician.
Dental 3-D Software Emerges
Articles discussing the use of Dentascans for the evaluation of the maxillary and mandibular bone for dental implants began to appear in the literature in the late 1980s.11-14 3-D dental software was introduced by Columbia Scientific Inc. (CSI) in 1988. The software was designed to create reformatted cross-sectional images of the alveolar ridges from CT data. In 1991, the ability to place graphical implants virtually onto CT images was introduced by CSI in a combination software package called ImageMaster-101®. Two years later CSI released the first version of Sim/Plant®, software that enabled placing “virtual” implants of the exact dimensions of commonly used implants on the CT images and visualizing a patient’s axial, cross-sectional, and panoramic views on one screen. SimPlant 6.0® hit the market in 1999, adding the technology to create 3-D reformatted images.15 After CSI was purchased by Materialise® (www.materialise.com) in 2001, SurgiGuide® technology for dental implant placement through surgical guides was introduced in 2002. Then in 2005, NobelBiocare (www.nobelbiocare.com) unveiled the NobelProcera®/NobelGuide™ technology and recently followed that up with a redesigned version of the software, NobelClinician®. Software programs from other manufacturers, including EasyGuide™ (Keystone Dental Inc., www.keystonedental.com), Straumann® coDiagnostiX (Straumann USA LLC, www.straumann.us), VIP™ Software (BioHorizons, www.biohorizons.com), ImplantMaster™ (IDent, www.ident-surgical.com), and others, are now available as well.
Using CT data, new stereolithographic modeling technologies by companies such as Medical Modeling (www.medicalmodeling.com), Materialise, and others have opened new avenues to the dental clinician to use exact one-to-one models of a patient’s bony anatomy for 3-D diagnosis and treatment planning. Discussions of the expanded use of these new technologies in dentistry, endodontics, implant dentistry, and oral and maxillofacial surgery are now frequently found in the literature.16,17
Although proprietary 3-D “virtual” software products were originally developed for the evaluation of a patient’s anatomy for the planning and placement of dental implants, these technologies can be used to provide the surgeon with valuable preoperative information prior to performing an oral surgical procedure. Having more information going into a surgery can only facilitate and expedite a better surgical outcome and minimize surgical trauma and the potential risks and complications to the patient. The advanced imaging provided by CT scanning can provide better clinical evaluation, case planning, surgical planning, and surgical execution in non-implant-related dentoalveolar surgery cases.
The Benefits of 3-D
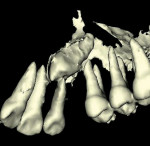
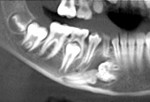
The removal of impacted wisdom teeth and supernumerary teeth and the surgical exposure of impacted teeth for orthodontic-aided eruption into the mouth are a few of the more common dentoalveolar surgical procedures that a dental surgeon encounters. Using conventional 2-D radiographs, the preoperative assessment of the position of these teeth can be difficult. Assessing the relationship of these teeth to vital structures such as the inferior alveolar nerve, mental foramen, incisive canal and nerve, maxillary sinus, inferior border of the mandible, floor of the mouth, and adjacent teeth can be problematic using conventional periapical and panoramic radiographs with no ability to evaluate the sites in three dimensions.
Using 2-D radiographs, the buccal-lingual assessment of the position of a mandibular third molar related to the inferior alveolar nerve can be particularly difficult and unpredictable due to anatomic variations of the mandibular canal.18,19 Going into surgery, the clinician usually is unaware of the true position of the mandibular canal buccal-lingually, because its position has not been found to be more buccal or more lingual.20 Frequently, the surgeon relies on panoramic radiographic signs such as third-molar root darkening, narrowing or diversion of the mandibular canal, root curvature, and the degree of interruption of the “white lines” outlining the mandibular canal to assess the proximity of the mandibular canal to the roots of a third molar.21-23 The reported overall incidence of inferior alveolar nerve injury related to third-molar removal has ranged from 0.5% to 8%,24-26 and the incidence of permanent injury to the mandibular nerve has been reported to be less than 1%.26-28 In circumstances where the surgeon is unsure of the proximity of the mandibular canal as it relates to the position of a third molar, it may be beneficial to better assess that relationship by viewing the anatomy in 3-D with a CT scan.29-31 The assessment of the position of impacted maxillary canine teeth is another circumstance in which a 3-D evaluation can be helpful diagnostically.32
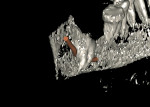
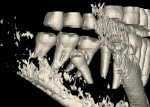
Additionally, all proprietary implant-planning softwares have the ability to virtually “draw” the position of the inferior alveolar nerve. Most of the softwares have the added ability to alter the sensitivity of the software to Hounsfield units and Isovalues. Using these techniques, the clinician can manipulate the 3-D reformation images to remove the surrounding bone, leaving images of teeth and nerves (Figure 1 through Figure 11).
Evaluation of Pathology
The evaluation of pathology of the mouth and jaws is another area in which a 3-D evaluation can be helpful to the surgeon. These problems often require extensive evaluation of the extent, location, and radiographic and anatomic characteristics, as well as the proximity of the lesion to teeth and vital structures. Frequently, their removal results in small or large bony and soft-tissue defects. Depending upon their size and severity, such defects can occasionally be unesthetic for patients.
The use of CT scans in the diagnosis of maxillofacial pathology is common. CT scans are frequently used to localize and measure the extent of the pathologic lesion, evaluate the involvement of teeth and surrounding vital structures, plan surgical approaches and procedures, and evaluate the size and contours of preoperative or postoperative deformities. They are also used in determining the volume of bone necessary for reconstructive procedures.
The evaluation of CT data of maxillofacial pathologic lesions in the 0.5-mm to 1-mm cross-sectional, axial, and panoramic views, as well as in the 3-D image reformations provided by proprietary implant software programs, can provide the clinician with important diagnostic information for visualization of lesions, surgical planning, and defect reconstruction. One-to-one stereolithographic model fabrication from CT data can be used to identify the extent of pathology and surgical excisions, create bone-cutting guides that can be used at the time of surgery, pre-bend stabilization bone plates, and outline bone volumes for reconstruction and grafting. This can all be done preoperatively, thus minimizing surgical time, surgical trauma, and patient morbidities, while maximizing esthetic and functional outcomes (Figure 12 through Figure 23).
Image Credit
Figures 1, 2, 4, 7, 8, 10, 11, 12, 19, 20, 21, 22, and 23 reprinted with permission from Orentlicher G et al. J Oral Maxillofac Surg. 2010;68(8):1933-1959.
References
1. Mozzo P, Procacci C, Tacconi A, et al. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998;8(9):1558-1564.
2. Mah J, Hatcher D. Three dimensional craniofacial imaging. Am J Orthod Dentofac Orthop. 2004;126(3):308-309.
3. Hashimoto K, Arai Y, Iwai K, et al. A comparison of a new limited cone beam computed tomography machine for dental use with a multi-detector row helical CT machine. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2003;95(3):371-377.
4. Sukovic P. Cone beam computed tomography in craniofacial imaging. Orthod Craniofac Res. 2003;6(suppl 1):31-36.
5. Flicek KT, Hara AK, Silva AC, et al. Reducing the radiation dose for CT colonography using adaptive statistical iterative reconstruction: A pilot study. AJR Am J Roentgenol. 2010;195(1):126-131.
6. Silva AC, Lawder HJ, Hara A, et al. Innovations in CT dose reduction strategy: application of the adaptive statistical iterative reconstruction algorithm. AJR Am J Roentgenol. 2010;194(1):191-199.
7. Leipsic J, Labounty TM, Heilbron B, et al. Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. AJR Am J Roentgenol. 2010;195(3):655-660.
8. Sagara Y, Hara AK, Pavlicek W, et al. Abdominal CT: comparison of low-dose CT with adaptive statistical iterative reconstruction and routine-dose CT with filtered back projection in 53 patients. AJR Am J Roentgenol. 2010;195(3):713-719.
9. Liang X, Lambrichts I, Sun Y, et al. A comparative evaluation of Cone Beam Computed Tomography (CBCT) and Multi-Slice CT (MSCT). Part II: On 3D model accuracy. Eur J Radiol. 2010;75(2):270-274.
10. Loubele M, Maes F, Schutyser F, et al. Assessment of bone segmentation quality of cone beam CT versus multislice spiral CT: a pilot study. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2006;102(2):225-234.
11. Rothman SL, Chaftez N, Rhodes ML, Schwarz MS. CT in the preoperative assessment of the mandible and maxilla for endosseous implant surgery. Radiology. 1988;169(2):581.
12. Casselman JW, Deryckere F, Hermans R, et al. Denta Scan: CT software program used in the anatomic evaluation of the mandible and maxilla in the perspective of endosseous implant surgery. Rofo. 1991;155(1):4-10.
13. Villari N, Fanfani F. Diagnostic contribution of CT in implantology: use of a new Denta-Scan reconstruction program. Radiol Med. 1992;83(5):608-614.
14. Tal H, Moses O. A comparison of panoramic radiography with computed tomography in the planning of implant surgery. Dentomaxillofac Radiol. 1991;20(1):40-42.
15. SimPlant Israel website. About CSI. Available at: https://sites.google.com/site/simplantisrael/simplantsources. Accessed April 12, 2011.
16. Quereshy FA, Savell TA, Palomo JM. Applications of cone beam computed tomography in the practice of oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008;66(4):791-796.
17. Orentlicher G, Goldsmith D, Horowitz A. Applications of 3-dimensional virtual computerized tomography technology in oral and maxillofacial surgery: current therapy. J Oral Maxillofac Surg. 2010;68(8):1933-1959.
18. Klinge B, Petersson A, Maly P. Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants. 1989;4(4):327-332.
19. Koong B, Pharoah MJ, Bulsara M, Tennant M. Methods of determining the relationship of the mandibular canal and third molars: A survey of Australian oral and maxillofacial surgeons. Aust Dent J. 2006;51(1):64-68.
20. Ohman A, Kivijarvi K, Blomback U, Flygare L. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofac Radiol. 2006;35(1):30-35.
21. Blaeser BF, August MA, Donoff RB, et al. Panoramic radiographic risk factors for inferior alveolar nerve injury after third molar extraction. J Oral Maxillofac Surg. 2003;61(4):417-421.
22. Monaco G, Montevecchi M, Bonetti GA, et al. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc. 2004;135(3):312-318.
23. Sedaghatfar M, August MA, Dodson TB. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005;63(1):3-7.
24. Rood JP. Permanent damage to inferior alveolar and lingual nerves during the removal of impacted mandibular third molars. Comparison of two methods of bone removal. Br Dent J. 1992;172(3):108-110.
25. Sisk AL, Hammer WB, Shelton DW, Joy ED Jr. Complications following removal of impacted third molars: the role of the experience of the surgeon. J Oral Maxillofac Surg. 1986;44(11):855-859.
26. Bruce RA, Frederickson GC, Small GS. Age of patients and morbidity associated with mandibular third molar surgery. J Amer Dent Assoc. 1980;101(2):240-245.
27. Alling CC III. Dysesthesia of the lingual and inferior alveolar nerves following third molar surgery. J Oral Maxillofac Surg. 1986;44(6):454-457.
28. Wofford DT, Miller RI. Prospective study of dysesthesia following odontectomy of impacted mandibular third molars. J Oral Maxillofac Surg. 1987;45(1):15-19.
29. Maegawa H, Sano K, Kitagawa Y, et al. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(5):639-646.
30. Friedland B, Donoff B, Dodson TB. The use of 3-dimensional reconstructions to evaluate the anatomic relationship of the mandibular canal and impacted mandibular third molars. J Oral Maxillofac Surg. 2008;66(8):1678-1685.
31. Flygare L, Ohman A. Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig. 2008;12(4):291-302.
32. Walker L, Enciso R, Mah J. Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofacial Orthop.2005;128(4):418-423.
About the Authors
Gary Orentlicher, DMD
Private Practice
Scarsdale, New York
Marcus Abboud, DMD
Founding Chair, Department of Prosthodontics and Digital Dentistry
School of Dental Medicine
Stony Brook University Medical Center
Stony Brook, New York