Composite Versus Ceramic for Large Posterior Restorations
Better distribution of occlusal forces and enamel-like wear properties offer advantages in some cases
Jihyon Kim, DDS
The intact tooth is a biomechanical marvel. The brittle, corrosion-resistant enamel and fracture tough dentin are fused along the dentinoenamel junction, which acts as a crack-stopping mechanism, distributing stresses to resist crack propagation. As a functional system, the whole is greater than the sum of its parts.
Advances in adhesive materials and methods have enabled us to better mimic the biomechanics of dental hard tissues and achieve dentin bond strengths close to the microtensile bond strength at the dentinoenamel junction.1 The preservation of healthy tooth volume is directly related to tooth longevity and should be a primary consideration in restoration, especially considering the longer average life expectancies of patients today.2 Because partial-coverage restorations facilitate minimally invasive, defect-driven preparations, the use of less conservative techniques must offer compelling advantages.
Regarding cuspal replacement, ceramic options have been favored over composite resin. The prevailing bias is that the material properties and esthetics of modern ceramics exceed those of composites and are better suited for large restorations. That may have been true with earlier generations of composite resin, but newer materials and methods are challenging the status quo. The flexural strength and fracture toughness of bondable ceramics closely mimic those of enamel, and these materials perform best when successfully bonded.3 However, composite resin matches the elastic modulus of dentin, making it an ideal dentin replacement. Although composite is confidently used for smaller intercuspal restorations, many clinicians believe that it is too weak for large restorations. Challenging these reservations, several clinical studies have demonstrated high success rates and long survival times in cases where direct composite was used for cuspal coverage.4-6 Others have shown comparable performance between milled ceramic and composite occlusal veneers in erosion cases,7 and many question the narrative that restorations involving cuspal coverage with composite suffer from higher failure rates than ceramic ones.8 These studies suggest that direct or indirect composite resin restorations may be a valid option for cuspal coverage.
Making a Case for Composite
All restorations have a limited life span. Therefore, a restoration that maintains the functionality of a tooth while protecting it from biologic damage and ensuring future restorability should be considered a restorative success. Considering that material fatigue/failure will eventually occur, attempts to contain the mode and extent of failure would be more rational than those to prevent it. When unanticipated early material failure occurs, the pressure to meet conventional parameters for success typically triggers a reactive preference for stronger materials. But is stronger better?
Increasing the thickness of a restoration in an attempt to gain strength leads to the sacrifice of sound tooth structure. In addition, a stiffer material may be able to withstand greater occlusal forces, but the transfer of those unfavorable forces to the underlying tooth or periodontium may result in avoidable biologic damage. The familiar scenario of an intact full-coverage, post-and-core restoration separated from a tooth that is damaged beyond repair is a catastrophic failure. In these cases, instead of being contained to the restoration, the failure is transferred to the tooth. The optimal material choice for occlusal replacement and control of failure should consider the patient and clinical presentation as well as the skill of the operator. Almost all indirect restorations begin with a direct foundation or base. Success starts from the bottom up with a solid adhesive layer that seals the dentin, protects the pulp, and contributes to the structural integrity of the tooth.
A well-bonded composite resin restoration can work in harmony with the natural dentition and may be the preferred material in cases involving structurally compromised teeth or occlusal wear.9 Although the specific clinical scenario determines whether a particular material property is a benefit or weakness, a direct restorative option enables maximum preservation of tooth volume, which might be critical to longevity. To some clinicians, the elastic modulus of composite resin may seem suboptimal for cuspal coverage in the posterior region; however, it permits a more favorable distribution of occlusal stresses rather than concentrating them into the tooth.10-11 Furthermore, the enamel-like wear properties of composite resin make it less abrasive to opposing dentition, and when compared with ceramics, any marginal breakage or chipping of composite can be more easily repaired.12-14 Composite restorations can also be easily adjusted or modified, which can be advantageous in managing and rehabilitating wear cases.
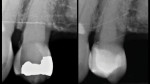
Composite offers multiple restorative modalities. The most conservative option is direct placement, which has no requirements for path of draw and insertion (Figure 1 through Figure 4). The ability to make the restorative material fit the needs of the tooth facilitates maximal conservation of tooth structure. When a tooth is severely compromised, this can be critical in restoring and extending its functionality. Alternatively, restoring with composite resin using a semi-direct technique offers the advantage of a single visit while also mitigating any polymerization shrinkage concerns associated with large composite restorations. Lastly, indirect methods using polymer blocks are also possible. When compared with ceramic materials, polymer blocks are faster to mill, place less strain on milling burs, more easily achieve fine margins, and offer favorable mechanical resistance and reparability. The ability to work with 0.5-mm minimal thicknesses can also be an advantage in occlusal wear cases.7
Factors for Clinical Success
Common composite restorative failures include secondary caries, marginal deficiencies, postoperative sensitivity, marginal ridge fracture, and wear.15 All of these failures can be attributed, by varying degrees, to issues with adhesion and/or curing. When polymerization shrinkage results in debonding of the dentin hybrid layer, it can contribute to sensitivity, marginal gaps, and the risk of secondary caries. The mechanical properties of dental composites, such as wear and fracture resistance, are dependent upon proper curing and degree of conversion.
Adhesive dentistry is technically challenging, and knowledge regarding how to properly use the chosen materials is essential to producing optimal outcomes. Beyond patient and material variables, restorative success with composite resins greatly depends on the operator's technique and ability to achieve predictable resin bonding. The successful management of polymerization shrinkage stress and prevention of debonding is critical to connecting the resin to the tooth and reconnecting the tooth to itself for it to function as a unified whole.
There are many techniques and materials available to optimize the resin bond (Figure 5 through Figure 9). Among other factors, moisture control and time are the variables that have the greatest impact on adhesion success. Isolation is key to achieving predictable results with any adhesive technique, and the use of a rubber dam is ideal. Allowing time for the unstressed maturation of the bond to dentin is an important investment to achieve the bond strength necessary to resist debonding of the overlying composite due to polymerization shrinkage stress. The dentin hybrid layer seals the dentin, protects the pulp, and is the connection between the restoration and tooth. This first resin layer, which is common to both direct and indirect restorative techniques, is the most important to long-term success.16
With semi-direct or indirect restorative methods, the polymerization shrinkage of the restorative material occurs while it is disconnected from the dentin hybrid layer. These options are recommended for situations in which direct techniques would be too challenging. In the extraoral semi-direct technique, the composite restoration is fabricated using a model, conversion is maximized with a postcuring heat treatment, and then the restoration is bonded to the tooth (Figure 10 through Figure 12).
An indirect technique may be preferred for clinicians who are less comfortable performing stress-reduced direct or semi-direct techniques. In addition, the mechanical properties of some polymer blocks exceed those of direct composite materials. They can achieve a higher degree of conversion and possess filler content with minimal porosities and gaps because they are manufactured under optimal conditions.
Regardless of the modality used, immediate dentin sealing can improve the bond strength of resin to dentin by 400%.17 Simple steps to improve the esthetics and wear resistance of composite resin include warming, shaping, and polishing. Research indicates that warming composite resins may improve their microsurface hardness—an important factor in material wear.18 Like most brittle materials, composite resin is stronger under compression than tension; therefore, creating rounded marginal ridge contours can reduce areas of tension and the potential for chipping. Finally, finishing and polishing that results in a highly polished surface improves the wear resistance and longevity of the restoration as well as reduces the tendency for biofilm to accumulate.19-20
Conclusion
With modern restorative materials and methods, it is very possible to maintain the dental health and function of our patients for their entire lifetimes. Adhesive protocols have freed clinicians from the need to rely on mechanical retention concepts, making restoration over repair possible. Conservative partial coverage restorations should be prioritized over more aggressive options, and the opinion that composite resin is less suited for cuspal coverage should be revisited. Composite resin offers multiple restorative modalities, which provides clinicians with several options based on skill level, preference, and patient needs. Ultimately, the clinical presentation and the goal of minimizing biologic damage to preserve tooth function and longevity should guide material selection.
About the Author
Jihyon Kim, DDS
Director
Injection Overmolding Institute
Seattle, Washington
Private Practice
Seattle, Washington
References
1. Urabe I, Nakajima S, Sano H, Tagami J. Physical properties of the dentin-enamel junction region. Am J Dent. 2000;13(3):129-135.
2. Simonsen RJ. New materials on the horizon. J Am Dent Assoc. 1991;122(7):24-31.
3. Fleming GJP, Addison O. Adhesive cementation and the strengthening of all-ceramic dental restorations. J Adhes Sci Technol. 2009;23(7-8):945-959.
4. da Veiga AMA, Cunha AC, Ferreira DM, et al. Longevity of direct and indirect resin composite restorations in permanent posterior teeth: a systematic review and meta-analysis. J Dent. 2016;54:1-12.
5. Borgia E, Baron R, Borgia JL. Quality and survival of direct light-activated composite resin restorations in posterior teeth: a 5- to 20-Year retrospective longitudinal study. J Prosthodont. 2019;28(1):e195-e203.
6. Deliperi S, Bardwell DN. Clinical evaluation of direct cuspal coverage with posterior composite resin restorations. J Esthet Restor Dent. 2006;18(5):256-267.
7. Schlichting LH, Resende TH, Reis K, et al. Ultrathin CAD-CAM glass ceramic and composite resin occlusal veneers for the treatment of severe dental erosion: an up to 3-year randomized clinical trial. J Prosthodont. 2022. doi: https://doi.org/10.1016/j.prosdent.2022.02.009.
8. Opdam N, Frankenberger R, Magne P. From ‘direct versus indirect' toward an integrated restorative concept in the posterior dentition. Oper Dent. 2016;41(S7):S27-S34.
9. Yip KH, Smales RJ, Kaidonis JA. Differential wear of teeth and restorative materials: clinical implications. Int J Prosthodont. 2004;17(3):350-356.
10. Yang H, Park C, Shin JH, et al. Stress distribution in premolars restored with inlays or onlays: 3D finite element analysis. J Adv Prosthodont. 2018;10(3):184-190.
11. Petropoulou A, Pantzari F, Nomikos N, et al. The use of indirect resin composites in clinical practice: a case series. Dentistry. 2013;3(3):173.
12. Shah K. Complex restoration of failing dentition with direct composites. Int J Dent Med Res. 2015;1:102-105.
13. Çulhaoğlu AK, Park J. A comparison of the wear resistance and hardness of two different indirect composite resins with a ceramic material, opposed to human enamel. Eur J Gen Dent. 2013;2(3):274-280.
14. Magne P, Belser UC. Porcelain versus composite inlays/onlays: effects of mechanical loads on stress distribution, adhesion, and crown flexure. Int J Periodontics Restorative Dent. 2003;23(6):543-555.
15. Manhart J, Chen H, Hamm G, Hickel R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004;29(5):481-508.
16. Alleman DS, Alleman DS, Deliperi S, et al. Decoupling with time: a solution to the problem of the hierarchy of bondability. Inside Dentistry. 2021;17(8):35-40.
17. Magne P, Kim TH, Cascione D, Donovan TE. Immediate dentin sealing improves bond strengths of indirect restorations. J Prosthetic Dent. 2005;94(6):511-519.
18. Dionysopoulos D, Papadopoulos C, Koliniotou-Koumpia E. Effect of temperature, curing time, and filler composition on surface microhardness of composite resins. J Conserv Dent. 2015;18(2):114-118.
19. Dionysopoulos D, Gerasimidou O. Wear of contemporary dental composite resin restorations: a literature review. Restor Dent Endod. 2021;46(2):e18.
20. Lopes GC, Vieira LC, Araujo E. Direct composite resin restorations: a review of some clinical procedures to achieve predictable results in posterior teeth. J Esthet Restor Dent. 2004;16(1):19-31.






![Fig. 3 Placement of stress-reduced direct composite restorations with polyethylene fiber. After the walls and cervical areas were completed on tooth No. 19, a polyethylene fiber material (Ribbond® Ultra, Ribbond) was lightly placed on top of a layer of microhybrid composite (CLEARFIL™ AP-X [A2], Kurarary Noritake) prior to being wetted with adhesive and imbedded into composite resin.](/media/thumbnail/97592/150x150)



![Fig. 7 After the resin coat was placed (CLEARFIL™ MAJESTY Flow [A2], Kuraray Noritake) and the dentin replacement was completed (CLEARFIL™ AP-X [A2], Kuraray Noritake), incorporating a fiber-reinforced composite (everX™, GC America), a mylar circumferential band (Transparent Matrix Band, Tor VM) was placed to perform the final enamel replacement layer.](/media/thumbnail/97596/150x150)