Evaluation of Enamel and Dentinal Cracks Using Methylene Blue Dye and the Operating Microscope
Glenn A. van As, DMD, BSc
The operating microscope became a staple of the endodontic discipline with its introduction by Apotheker in 1981.1 Since the late 1980s and early 1990s, when Carr, Ruddle, Arens, Buchanan, and others integrated it into both standard and surgical endodontic therapy, it has become a routine part of the armamentarium in the discipline. The tremendous improvement in visual acuity through enhanced levels of magnification (2X to 20X) and coaxial shadow-free illumination has allowed for improvements of treatment outcomes in the field of endodontics.2-17
During the rest of the 1990s and the early years of the this millennium, the microscope (Figure 1) gained a new foothold in general practice, particularly with dentists interested in doing molar endodontics, prosthodontics, and cosmetic procedures.18-35 Clinicians from microscope-centered practices almost always note two things when first using the operating microscope routinely for restorative procedures: an alarming amount of new and recurrent decay, and an overwhelming number of crack lines—mostly around existing restorations, most notably amalgams.36
Studies by Guertsen et al37 looking at the prevalence of cracked teeth found that these teeth were the third most common cause of tooth loss in industrialized countries, primarily affecting maxillary molars and premolars as well as mandibular molars.
Visualization of these cracks is difficult using the naked eye or low levels of telescopic loupes unless the crack is fairly well advanced, with a large or darkly stained fracture line. Early cracks are often called incomplete fractures, whereas late-stage fractures are called complete (where cuspal fracture has occurred or the tooth has split vertically). In many instances, treatment of these incomplete but "end-stage" symptomatic cracks involves cuspal coverage and endodontics on teeth with short-term chewing sensitivity combined with full-coverage restorations in teeth with thermal sensitivity. Unfortunately, because of the difficulty in the past in visualizing the early and asymptomatic fracture lines that often are lightly stained enamel and dentin cracks, they can be missed until they become fairly advanced, symptomatic, or complete in nature.
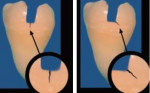
In general, there are two basic varieties of dentinal fractures: oblique and vertical. The most commonly seen fractures in dentin, which often occur under existing amalgam restorations, are the oblique fractures. These fractures run in the floor of the preparation, undermining the cusps; they run in a more horizontal direction, and they are often the precursors to a fractured cusp. When they become symptomatic, many patients will complain of a sharp and intense, but generally short-term, sensation while chewing foods, particularly when they apply lateral pressure to the cusp or cusps that are involved. In the literature, Fennis et al found that oblique complete fractures are more common on molars than premolars (79% to 21%) and occur on the maxillary buccal cusps (66% to 34%) and the mandibular lingual cusps (75% to 25%).38 Vertical fractures run mesial to distal on the tooth and may be the precursors to a split tooth. These more dangerous, vertically oriented cracks may result in devastating fractures, with pulpal and/or periodontal breakdown. The vertical fractures may progress into a split tooth that is completely fractured and unrestorable (Figure 2A and Figure 2B).
Guidelines for using magnification
In 2003, Clark, in his landmark article39 on the detection and evaluation of early enamel and dentinal cracks with the operating microscope, provided guidelines for the "recognition, visualization, classification, and treatment of cracked teeth based on the routine use of x16 magnification." This article marked the first time that someone tried to provide order to the often-bewildering variety of fractures that can be encountered in posterior teeth viewed under the microscope, particularly under existing amalgam restorations. Many of these fracture lines were present on teeth that were not symptomatic, but the fractures were still detectable with the operating microscope at magnifications of 12X to 14X and above. There now existed an exciting possibility of treating cracked teeth with cuspal coverage restorations that would, hopefully, prevent further progress of the crack before symptoms manifested.37,40,41
Historically, dentistry has been driven by a symptoms-based approach to the treatment of cracks, where the microscopic details pertaining to the size and location of the crack were not visible to the naked eye. The patient presented with a complaint of chewing or thermal sensitivity and the clinician set about trying to determine which tooth was the culprit. The crack was localized by having patients bite on cotton rolls or hard plastic instruments to isolate individual cusps, which could be cracked. Traditionally, cracks have been detected by transillumination, using caries-detector dyes, alternating between hydrated and dry views, and using methylene blue dye.
Although transillumination is the most popular method used, its intensity of light illuminates all cracks and makes subtle cracks invisible. Methylene blue dye is superior to caries-indicator dyes because it pools much better. This dye is very dark and is very useful for both extra- and intra-coronal cracks. As Clark mentioned in his article, there are some negative results from using methylene blue; the plaque will stain profusely, as it does with dentin that has been treated with sodium hypochlorite. Methylene blue dye stains all cracks and does not differentiate between early cracks, which may not be stained well either before or after the dye is used, and the stain can alter the dentist’s ability to differentiate the cracks. Methylene blue dye is extremely effective, however, for educating patients about cracks and vital for documentation, as many of the cracks in dentin are extremely difficult to photograph. The ability to photograph these extensive cracks is especially important in gaining approval from insurance dental plans for cuspal coverage restorations for the teeth.42-44
Protocol for using Methylene blue dye and the microscope
Clark suggested that to inspect cracks with the microscope, all posterior teeth should be polished with coarse pumice slurry, completely dried, and then methylene blue dye should be applied with a disposable applicator tip. The dye will stain clothing and countertops, so extreme care must be taken to prevent it from coming into contact with these items. The author has found that the unidose packaging of Vista Blue™ (Vista Dental Products, Racine, WI) is a way of limiting the risk of staining to clothing. It is an adequately sized brush tip that can be used for a single patient and disposed of without fear of sterilization issues.
Documenting fractures using magnification
Early detection of enamel and dentinal cracks became possible with the operating microscope because of the magnification and illumination possible, but the documentation of such fractures remained difficult. The ability to capture early cracks with digital photography was necessary for at least two reasons. First, when dealing with cracks on asymptomatic teeth, patients need to be educated as to why extracoronal restorations may be required when the existing restoration seems to be faring well. The ability to demonstrate visually from a digital photograph that is magnified at 2X to 20X and displayed on a large monitor is incredibly helpful in educating patients on the need for cuspal coverage on these teeth. Second, most insurance plans require proof that full-coverage restorations are needed on teeth that previously had minimally sized restorations but also had a devastating array of severe fracture lines. Radiographically, the teeth in question often seem to be restored in a conservative fashion without evidence of decay or fractures. It is only at the end stage of development that these fracture lines become evident radiographically. It became obvious that a system for enhancing and documenting these "sleeping giant" fractures was essential in both educating patients and insurance companies to the problems that are present in these teeth.
The author has developed a system of documenting these fracture lines that starts with taking preoperative photographs before placing a rubber dam. After the rubber dam is placed, the tooth is pumiced with a slurry of prophylaxis paste and then evaluated both visually and photographically. Then the enamel cracks are dyed, before the restoration is removed. The dye is left to sit for 10 to 15 seconds and then rinsed off. Cracks in the enamel are very evident after methylene blue dye placement and give the clinician an idea of the underlying pathological cracks. Often the actual extent and final direction of the cracks is not conclusive until the restoration has been removed and the floor of the preparation has been evaluated after dye placement. Photographs at low and high power of cracked portions of the tooth are taken. The existing restorations, if they are present (often these are amalgam), are now removed and the dentinal surface is evaluated, both dry and moist, to see the final extent and direction of the fractures present. It is, at times, obvious from the initial methylene blue dye placement on the enamel cracks where the final fractures will exist, but at times the direction and extent of the dentin cracks can be surprisingly different from what was postulated before the removal of the restorations.
Clark mentioned in his article that dentin cracks fall into two basic categories. Oblique fracture lines run along the floor of the preparation, undermining the cusps of enamel, and are often found on symptomatic teeth that are sensitive to chewing for short periods of time. The author’s clinical experience has shown that these cracks are less likely to create pulpal problems than the precursor to vertical root fractures, which are vertical cracks. Oblique fractures are often best treated with cuspal coverage restorations, and can often be found in asymptomatic teeth when the existing restorations are present. These fractures are precursors to cuspal fractures and the patient should be advised of their presence. The author will often suggest cuspal coverage in the form of extracoronal restorations as the preferred treatment, although some literature suggests that a bonded intracoronal restoration also may provide a solution.37
According to Clark, the more ominous type of fracture is vertical in direction. Vertical fractures run in a mesial to distal direction and are more commonly associated with thermal sensitivity in addition to chewing sensitivity. These fractures are more commonly associated with teeth that either have or will develop irreversible pulpitis and should be treated expeditiously with full-coverage restorations. On these teeth, the author will often cement the final restoration provisionally for a period of 2 to 3 months to evaluate whether the tooth requires endodontics when symptoms are not present initially or are mild in nature. Vertical fractures can be found in teeth that are not symptomatic and still vital. They are a precursor to a complete vertical fracture and should be treated quickly and comprehensively to avoid devastating fractures that would result in the need for extraction.
Occasionally, these fractures are visible running mesial to distal through the floor of the pulp chamber during endodontic access. If this is the case, the prognosis for the tooth is severely jeopardized. Should interproximal probings be increased on either side of the tooth in conjunction with the discovery of a vertical fracture running along a pulpal floor, then the current thought is that an extraction of the tooth and replacement with an implant is the best alternative.
Case Presentation
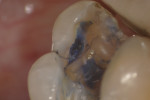
In this case, the patient had an asymptomatic maxillary left first molar with a conservative existing occlusal-lingual amalgam restoration that showed no signs of recurrent decay radiographically but, clinically, at high magnification demonstrated a gray shadow around the periphery of the amalgam, which is a sign of marginal leakage and recurrent decay. Several fractures were seen as well at higher magnifications on the occlusal surface. The tooth was photographed at low, medium, and high magnifications (Figure 3A; Figure 3B; Figure 3C) and then the rubber dam was placed. Initial application of methylene blue dye to the enamel cracks demonstrated substantial cracks on the occlusal surface and a pair of cracks on the mesial marginal ridge, one of which was large enough to house debris (Figure 4A; Figure 4B; Figure 4C). There was a substantial crack on the midbuccal of the tooth in an anatomic groove which, according to Clark, is a low-risk area for large fractures. Additional fractures ran across the transverse ridge connecting the mesial and distal pits and, in addition, ran up the mesial-lingual cusp from the mesial pit.
The amalgam restoration was removed and the tooth was again stained with methylene blue dye to show a dramatic and large vertical crack that runs from the mesial interproximal area to the mid-buccal groove (Figure 5A; Figure 5B; Figure 5C). Given the location, type, and degree of the fracture, combined with dentinal fractures in the rest of the tooth, a resin core build-up was completed, and the occlusion adjusted (Figure 6A; Figure 6B; Figure 6C). The patient was shown the photographs, which were sent away for insurance preauthorization for a full-coverage restoration, and the patient was advised of the definitive treatment plan for this tooth, which includes the possibility that endodontic therapy may be required should the tooth become symptomatic with signs of irreversible pulpitis. The existing buildup restoration provides an opportunity to evaluate pulpal response prior to the definitive restoration being placed, after the insurance predetermination of benefits is returned to the dental office for this patient.
Conclusion
As more clinicians recognize the value of high levels of magnification that are possible with the operating microscope, they will encounter the propensity of enamel and dentin cracks that are present. Many of these fractures are asymptomatic harbingers of the future and if detected with methylene blue dye and documented with the microscope earlier, the opportunity to treat these "sleeping giants" before they reach a later stage may become more prevalent. If this occurs, then the treatment of fractures in the dental profession will change from a "symptoms-based" approach to a "signs-based" approach, and perhaps the devastating effects of vertical and oblique fractures will become a thing of the past.
References
1. Apotheker H, Jako GJ. A microscope for use in dentistry. J Micosurg. 1981;3(1):7-10.
2. Carr GB. Microscopes in endodontics. J Calif Dent Assoc. 1992;20(11):55-61.
3. Carr GB. Common errors in periradicular surgery. Endod Rep. 1993;8(1):12-18.
4. Mounce R. Surgical operating microscope in endodontics: the paradigm shift. Gen Dent. 1995;43(4):346-349.
5. Feldman M. Microscopic surgical endodontics NY State Dent J. 1994;60(8): 43-45.
6. Ruddle CJ. Endodontic perforation repair: using the surgical operating microscope. Dent Today. 1994;13(5):49-53.
7. Ruddle CJ. Nonsurgical endodontic retreatment. CDA Journal. 1997;25(11): 769-799.
8. Tsesis I, Rosen E, Schwartz-Arad D, et al. Retrospective evaluation of surgical endodontic treatment: traditional versus modern technique. J Endod. 2006;32(5):412-416.
9. Schirrmeister JF, Hermanns P, Meyer KM, et al. Detectability of residual Epiphany and gutta-percha after root canal retreatment using a dental operating microscope and radiographs—an ex vivo study. Int Endod J. 2006;39(7): 558-565.
10. Sempira HN, Hartwell GR. Frequency of second mesiobuccal canals in maxillary molars as determined by use of an operating microscope: a clinical study. J Endod. 2000;26(11):673-674.
11. Schwarze T, Baethge C, Stecher T, et al. Identification of second canals in the mesiobuccal root of maxillary first and second molars using magnifying loupes or an operating microscope. Aust Endod J. 2002;28(2):57-60.
12. Gorduysus MO, Gorduysus M, Friedman S. Operating microscope improves negotiation of second mesiobuccal canals in maxillary molars. J Endod. 2001;27(11): 683-686.
13. de Carvalho MC, Zuolo ML. Orifice locating with a microscope. J Endod. 2000; 26(9):532-534.
14. Buhrley LJ, Barrows MJ, BeGole EA, et al. Effect of magnification on locating the MB2 canal in maxillary molars. J Endod. 2002; 28(4):324-327.
15. Stropko JJ. Canal morphology of maxillary molars: clinical observations of canal configurations. J Endod. 1999;25(6):446-450.
16. Coutinho Filho T, La Cerda RS, Gurgel Filho ED, et al. The influence of the surgical operating microscope in locating the mesiolingual canal orifice: a laboratory analysis. Pesqui Odontol Bras. 2006;20(1):59-63.
17. Michaelides PL. Use of the operating microscope in dentistry. J Calif Dent Assoc. 1996;24(10):9.
18. van As GA. Magnification and the alternatives for microdentistry. Compend Contin Educ Dent. 2001;22(11):1008-1016.
19. van As GA. Using the surgical operating microscope in general practice. Contemporary Esthetics and Restorative Practice. 2000;4(1):34-40.
20. van As GA. Enhanced acuity through magnification: clinical application for increased visualization. Collaborative Techniques. 2001;1(2):40-42.
21. Martignoni M, Schonenberger A. Precision Fixed Prosthodontics: Clinical and Laboratory Aspects. Chicago, Illinois; Quintessence Publishing Co, Inc: 1990.
22. Sheets CG, Paquette JM. Enhancing precision through magnification. Dent Today. 1998;17(1): 44-49.
23. Sheets CG, Paquette JM. The magic of magnification. Dent Today. 1998;17(12):61-67.
24. Cruci P. An operating microscope in general dental practice. Dental Practice. 1999;37(9):1-5.
25. Friedman MJ, Mora AF, Schmidt R. Microscope-assisted precision dentistry. Compend Contin Educ Dent. 1999;20(8): 723-736.
26. Mora AF. Restorative microdentistry: A new standard for the twenty-first century. Prosthet Dent Rev. 1998;1(3):20.
27. Piontkowski PK. The renaissance of dentistry: An introduction to the surgical operating microscope. Dent Today. 1998;17(6):82-97.
28. Paquette JM. The clinical microscope: Making excellence easier. Contemporary Esthetics and Restorative Practice. 1999;3(10):12-20.
29. Christensen GJ. Magnification in dentistry: useful tool or another gimmick? J Am Dent Assoc. 2003;134(12):1647-1650.
30. Clark DJ. The big push to clinical microscopes for esthetic dentistry. Contemporary Esthetics and Restorative Practice. 2005;9(11): 30-33.
31. Clark DJ, Kim J. Optimizing gingival esthetics: A microscopic perspective. Oral Health. 2005;April: 116-126.
32. Clark D. Microscope enhanced aesthetic dentistry. Dent Today. 2004;23(11):96-101.
33. Garcia A. Dental magnification: a clear view of the present and a close-up view of the future. Compend Contin Educ Dent. 2005;26(6A Suppl):459-463.
34. van As GA. The use of extreme magnification in fixed prosthodontics. Dent Today. 2003;22(6):93-99.
35. van As GA. The role of the dental operating microscope in fixed prosthodontics. Oral Health. 2002;June: 11-25.
36. Friedman MJ, Landesman HM. Microscope-assisted precision (MAP) dentistry: a challenge for new knowledge. J Calif Dent Assoc. 1998;26(12):900-905.
37. Geurtsen W, Schwarze T, Gunay H. Diagnosis, therapy, and prevention of the cracked tooth syndrome. Quintessence Int. 2003;34(6):409-417.
38. Fennis WM, Kuijs RH, Kreulen CM, et al. A survey of cusp fractures in a population of general dental practices. Int J Prosthodont. 2002;15(6): 559-563.
39. Clark DJ, Sheets CG, Paquette JM. Definitive diagnosis of early enamel and dentin cracks based on microscopic evaluation. J Esthet Restor Dent. 2003;15(7): 391-401.
40. Geurtsen W. The cracked-tooth syndrome: clinical features and case reports. Int J Periodontics Restorative Dent. 1992;12(5): 395-405.
41. Patel DK, Burke FJ. Fractures of posterior teeth: a review and analysis of associated factors. Prim Dent Care. 1995;2(1):6-10.
42. Carr GB. Microscopic photography for the restorative dentist. J Esthet Restor Dent. 2003;15(7):417-425.
43. Behle C. Photography and the operating microscope in dentistry. J Calif Dent Assoc. 2001;29(10):765-771.
44. van As GA. Digital documentation and the dental operating microscope. Oral Health.2001;91(12):19-25.
About the Author
Glenn A. van As, DMD, BSc
Private Practice
North Vancouver
British Columbia, Canada