Impacted Mandibular “Double” Third Molar: Fusion or Gemination? A Case Report
Abstract: Dental fusion is defined as an abnormality in tooth shape caused by developmental tooth disturbances that produce an intimate union of dental tissues. This case report discusses treatment of a mandibular impacted "double" third molar in a 21-year-old patient that could have been related to either gemination or tooth fusion. Radiological examination allowed for careful analysis of the tooth's shape and root development, relation to the inferior alveolar nerve, and 3-dimensional position. After evaluation of therapeutic options and risks, and with the patient's consent, the authors opted to extract the tooth in question. Such favorable conditions as the incomplete development of the roots and the relatively young age of the patient, combined with the use of an antibiotic and antiseptic prophylaxis as well as a standard surgical approach, enabled a successful result to be achieved with no related complications.
Dental abnormalities comprise several pathological variants that can be classified by four different tooth variables: position, number, shape, and structure.1 Among these, shape anomalies are prevalent in daily dental practices and can be challenging to address. Shape anomalies can be further identified as (1) fusion, (2) gemination, (3) concrescence, (4) root dilaceration, (5) dens invaginatus, (6) dens evaginatus, and (7) taurodontism.2 The first three anomalies involve the fusing together of at least two teeth, while the latter four anomalies usually involve an individual tooth.
Concrescence is the union of two teeth at the cementum level and constitutes 1.4% of all dental anomalies.2 Fusion is defined as the union of two separate contiguous dental germs, resulting in the appearance of one tooth fewer than the normal count in the dentition.3 Gemination is an attempt of a single tooth germ to divide and does not affect the standard tooth count.2 The overall prevalence of fusion and gemination in both dentitions (primary and permanent) is reported to be 0.5% to 1%. When referring to only the permanent dentition, fusion and gemination are less common with a prevalence of 0.2% to 0.05%.4
This article presents a case report of a mandibular "double" third molar. The article describes and analyzes the clinical decision-making process related to the diagnosis and treatment of the following shape abnormalities: concrescence, fusion, and gemination.
Case Presentation
Clinical and Radiographic Evaluation
A 21-year-old female patient presented to the authors' dental clinic complaining of pain and discomfort in the mandibular left third molar region. She did not report any significant medical history of chronic conditions or dental disease. A comprehensive intraoral examination revealed no evidence of periodontitis or caries. Additionally, the mandibular left third molar was not visible clinically.
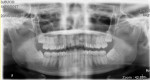
A panoramic radiograph revealed a mandibular left impacted third molar with three roots and an abnormally large crown size (Figure 1). The unusual tooth morphology suggested that this was a case of fusion between the third molar and a supernumerary tooth (ie, a fourth molar).
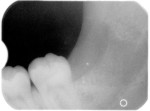
To determine the risks-benefits and treatment plan, the situation necessitated that the relationship between the roots of the third molar and the inferior alveolar nerve (IAN) be investigated. Cone-beam computed tomography (CBCT) was utilized to accurately identify the IAN position relative to the malformed third molar. The IAN ran lingual to molar roots (Figure 2). Additionally, CBCT imaging was used to calculate the overall mesiodistal crown length, which was determined to be 15.56 mm.
After a discussion of treatment options with the patient, it was agreed that the mandibular left third molar would be extracted. Pharmacological therapy without surgery was excluded due to the likelihood of symptom recurrence, and coronectomy was also excluded because of the minimal risk of nerve injury associated with the procedure. The patient was scheduled for exodontia surgery, and approval for the treatment was documented.
Surgical Procedure
The patient was instructed to use a chlorhexidine gluconate mouthrinse (0.12%) before the surgery. Local anesthesia was administered via the IAN and long buccal nerve block utilizing two cartridges of 3% mepivacaine plus vasoconstrictor, and profound local anesthesia was confirmed. A sulcular incision was made from the distal aspect of tooth No. 19 to the distal aspect of tooth No. 18, with a crestal incision extending posterior to the ascending mandibular ramus, and a full-thickness envelope flap was elevated. Specifically, a distal-relieving incision continued 45 degrees obliquely from the distobuccal cusp of tooth No. 18 to the mandibular ramus (Figure 3).
After a mucoperiosteal flap was elevated, the impacted third molar and the surrounding bone were exposed. Third molar removal was achieved by performing a vestibular ostectomy with a contra-angle handpiece and round carbide bur. After third molar luxation, the mesial portion of the dental crown was first sectioned with a contra-angle handpiece and fissure carbide bur and removed. The residual part of the third molar was removed using an elevator (Figure 4).
Sodium chloride irrigating solution (0.9%) was then applied to the area, and alveolar curettage was performed (Figure 5). The flap was replaced and closed with a 4-0 silk suture.
The patient was discharged after being provided with postoperative instructions. These included amoxicillin (1 g), one tablet every 8 hours for 5 days; specific diet and dental hygiene measures; chlorhexidine gluconate mouthrinse (0.12%) every 12 hours starting the day after surgery until suture removal, which occurred after 10 days; and anti-inflammatory therapy with paracetamol 1000 mg for pain control starting from the day of surgery.
Follow-up
No complications appeared, either at suture removal or at long-term follow-up. Clinical and radiographic follow-up showed healing of both soft and hard tissues (Figure 6) that was determined to be within normal limits for post-extraction of a third molar tooth.
Discussion
Many dental abnormalities, such as supernumerary teeth and anatomical malformations, are commonly encountered in clinical practice. However, some abnormalities, such as fusion or gemination, are seen less often.5 Furthermore, shape anomalies can be difficult to recognize with standard imaging and clinical examination.6 As such, this case report seeks to highlight decision-making and learning gleaned from this case's evaluation and treatment to aid other clinicians who may encounter such abnormalities.
Having knowledge of normal and abnormal anatomical features and being able to provide a correct diagnosis are crucial so that the most suitable surgical or nonsurgical treatment options may be administered. It is well-established that an overall treatment plan and the complexity of individual therapies, like endodontic treatment or dental extractions, can be influenced by abnormal tooth size or shape.5 Hence, it is important to analyze the clinical and radiological differences between similar developmental anomalies of teeth, such as gemination and fusion.
In the present case, after a primary radiological analysis, the authors focused on three possible dental abnormalities: concrescence, gemination, and tooth fusion (Table 1). An examination of the panoramic radiograph showed that the union of the teeth involved not only the cementum, but also the dentin and enamel. This finding did not support a diagnosis of concrescence, in which the fusion is characterized exclusively by a union of only cementum.7 Moreover, the mandibular third molar region is an unusual area for the occurrence of concrescence, as this dental anomaly is typically found in the maxillary molar region, with a particular predilection for upper third molars.8 Thus, concrescence was excluded from the differential diagnosis.
Gemination was also considered as a possible cause of the abnormality. The term "gemination" refers to a developmental tooth anomaly characterized by a double crown, usually not totally separated crowns, with a shared root and pulp space.9 This partial "double tooth" is related to a disturbance during odontogenesis, in which the tooth germ is partially cleaved.10 In this case, the mandibular left third molar was characterized by two fused crowns that shared a pulp chamber and root canals. These anatomical features aligned with gemination; therefore, the authors did not exclude gemination from the differential diagnosis.
Finally, the third hypothesis was analyzed: a fusion between the mandibular left third molar and a supernumerary fourth molar. Tooth fusion is an anomaly represented by a "double tooth" caused by the union of two adjacent dental germs.9 Its anatomical characteristics lead to two main variants: (1) a "double tooth" with a double crown sharing a pulp chamber and root canals, and (2) a "double tooth" with a double crown with two different pulp chambers and separated canals.11 The first variant presents with clinical anatomy that is indistinguishable from that seen in gemination; therefore, this fusion variant was also included in the differential diagnosis.
To determine if one cause of the "double tooth" presentation in this case could be identified, the analysis of other factors, such as the overall number of teeth present and the patient's radiological history, was used and can be critical to distinguish tooth fusion from gemination. In many cases, counting the number of teeth can make clear which anomaly the clinician is facing. A standard number of teeth is more compatible with a diagnosis of gemination, while a reduced number of teeth usually indicates a case of tooth fusion.12 Nevertheless, fusion or gemination involving a supernumerary tooth complicates the diagnostic framework.11 For example, in this case, the presence of a hypothetical supernumerary tooth and subsequent fusion did not allow a diagnosis based on a standard number of teeth, because the large abnormal tooth could have resulted from either a fusion between the third molar germ and a supernumerary germ or a division of the third molar germ.
Thus, examination of all previous panoramic radiographs allows the clinician to observe tooth bud formation and assess at which germ stage the "double tooth" presented. Without regular radiological follow-up, however, a definite diagnosis cannot be made.11 In the present case, the absence of available regular radiographic records throughout the patient's childhood and adolescence did not allow the clinicians to determine the ultimate cause of the "double tooth."
A further complication, as seen in this case, is that the treatment plan to address the presence of a "double tooth" and the patient's reported symptoms depends on various factors, such as localization, whether the dentition is primary or permanent, whether the pulp chamber is connected or unconnected, whether or not there is supernumerary tooth involvement, and any problems associated with esthetics, eruption, or periodontics.10,13 For instance, the fusion of two permanent teeth in the anterior region could be the origin of esthetic and functional issues. Thus, a multidisciplinary treatment plan involving endodontic, orthodontic, and surgical interventions could be required.13
Nevertheless, in the present case, the mandibular left "double" third molar was not linked to esthetic or functional problems. The localization and position of the tooth, however, were factors that had to be taken into account. The lack of space in the arch, which prevented the tooth from erupting in a correct and functional position, and the symptoms of recurrent pain reported by the patient represented the indications for the extraction.14
One further consideration is the importance of careful surgical planning to address the complexity of the abnormality, with attention given to appropriate extraction techniques and instruments. Intrasurgical management involves actions taken during surgery to address any complications, such as tooth fracture or damage to adjacent structures. The tooth may require segmentation into multiple sections, contingent on its orientation and path of exit. In this case, the presence of the mandibular second molar and the surrounding alveolar bone impeded the egress route. Hence, to mitigate the risk of applying excessive force, which could potentially result in mandibular bone fracture, it may be imperative to employ a bur to excise the oversized crown and eventually partition the roots, thereby ensuring a minimally traumatic extraction process. The lever movements must be minimally invasive and sufficient only to dislocate the roots, without applying additional force. The provision of adequate anesthesia and postoperative care helps ensure patient comfort and an optimal outcome. Effective communication with the patient throughout the process is essential for informed decision-making and patient satisfaction.
Conclusion
As demonstrated in this case report, the diagnosis of gemination versus fusion was not possible without obtaining prior panoramic radiographs showing the main stages of tooth development during the patient's childhood and adolescence. In this case, however, based on patient symptoms and a risk-benefit analysis, an accurate diagnosis of the underlying pathophysiology of the "double tooth" would not have markedly influenced the treatment plan.
While there are many developmental dental abnormalities that are not often encountered in clinical practice and reports in the literature are scarce, an accurate radiological examination and an in-depth knowledge of dental anomalies should enable clinicians to treat these kinds of problems in a way that allows for maximum patient benefit and minimum risk.
About the Authors
Nadim Oliva, DDS, MSc
Specialist in Oral Surgery, University of Milan, Milan, Italy
Martina Casaburi, DDS
Resident in Oral Surgery, University of Bologna, Bologna, Italy
Silvano Mucllari, DDS
Resident in Oral Surgery, University of Milan, Milan, Italy
Ludovico Callerio, DDS
Dentist, Italian Stomatological Institute, Milan, Italy
References
1. Shokri A, Poorolajal J, Khajeh S, et al. Prevalence of dental anomalies among 7- to 35-year-old people in Hamadan, Iran in 2012-2013 as observed using panoramic radiographs. Imaging Sci Dent. 2014;44(1):7-13.
2. Guttal KS, Naikmasur VG, Bhargava P, Bathi RJ. Frequency of developmental dental anomalies in the Indian population. Eur J Dent. 2010;4(3):263-269.
3. Goutham B, Bhuyan L, Chinnannavar SN, et al. Prevalence of dental anomalies in Odisha population: a panoramic radiographic study. J Contemp Dent Pract. 2017;18(7):549-553.
4. Morris DO. Fusion of mandibular third and supernumerary fourth molars. Dent Update. 1992;19(4):177-178.
5. Bilge NH, Yeşiltepe S, Törenek Ağırman K, et al. Investigation of prevalence of dental anomalies by using digital panoramic radiographs. Folia Morphol (Warsz). 2018;77(2):323-328.
6. Zhu M, Liu C, Ren S, et al. Fusion of a supernumerary tooth to right mandibular second molar: a case report and literature review. Int J Clin Exp Med. 2015;8(8):11890-11895.
7. Consolaro A, Hadaya O, Miranda DAO, Consolaro RB. Concrescence: can the teeth involved be moved or separated? Dental Press J Orthod. 2020;25(1):20-25.
8. Gernhofer KJ. Concrescence of a maxillary second and third molar. J Calif Dent Assoc. 2009;37(7):479-481.
9. American Association of Endodontics. Glossary of Endodontic Terms. 10th ed. 2020. https://www.aae.org/specialty/clinical-resources/glossary-endodontic-terms/. Accessed March 25, 2024.
10. Ahmed HMA, Dummer PMH. A new system for classifying tooth, root and canal anomalies. Int Endod J. 2018;51(4):389-404.
11. Camargo AJ, Arita ES, Watanabe PC. Fusion or gemination? An unusual mandibular second molar. Int J Surg Case Rep. 2016;21:73-77.
12. Altug-Atac AT, Erdem D. Prevalence and distribution of dental anomalies in orthodontic patients. Am J Orthod Dentofacial Orthop. 2007;131(4):510-514.
13. Tuna EB, Yildirim M, Seymen F, et al. Fused teeth: a review of the treatment options. J Dent Child (Chic). 2009;76(2):109-116.
14. De Bruyn L, Vranckx M, Jacobs R, Politis C. A retrospective cohort study on reasons to retain third molars. Int J Oral Maxillofac Surg. 2020;49(6):816-821.