Mönckeberg Arteriosclerosis of the Facial Vasculature Presentation on CBCT: A Case Report
Karen Berrigan, DMD, MS; Sabita Rao, DMD; John R. Francis, DDS, MS; Douglas W. Beals, DDS, MS; and Vijay Parashar, BDS, DDS, MDSc
Abstract: Mönckeberg arteriosclerosis, also known as Mönckeberg sclerosis or Mönckeberg medial calcinosis, is a well-documented phenomenon in medicine due to its association with a number of serious systemic conditions and aging. This article presents a unique case of Mönckeberg arteriosclerosis in the oral facial region demonstrated clearly on cone-beam computed tomography (CBCT). The reporting of Mönckeberg arteriosclerosis in dental literature is uncommon even though the radiographic features of the head and neck on plain film and CBCT are unique to the condition. As dentistry and medicine strive to move toward an integrated one-health model, it will be important for dental practitioners to recognize this condition during dental radiographic evaluation. A practitioner's understanding of the potential medical implications and the need for appropriate referral to a medical colleague could be lifesaving for a dental patient.
Mönckeberg sclerosis (MS), a distinct pathological condition, was first reported by German pathologist J.G. Mönckeberg in 1903.1 Its reporting in the dental literature is rare with many of the articles illustrating this entity as incidental findings on plain film radiographs.1-4 The following case report highlights some of the more interesting radiographic features of MS visualized using cone-beam computed tomography (CBCT).
MS is characterized by the deposition of calcium in the form of crystalline hydroxyapatite in the tunica media layer of medium- and small-sized muscular arteries.1 The arteries most affected are those of the lower extremities.3 There have also been isolated case reports of the condition affecting the facial, coronal, and cerebral arteries.1,2,4
While the exact etiology of MS remains largely unknown, previous literature does support its association with a number of factors. MS has been detected more frequently in patients with specific medical conditions, including type 2 diabetes mellitus, hyperlipidemia, chronic kidney disease, and end-stage renal failure.1,5 Other systemic conditions that have positive correlations with MS are chronic inflammatory conditions, such as systemic lupus erythematous and disorders of calcium and phosphate metabolism.1,5 Some authors have also described vitamin K deficiency and medications that inhibit vitamin K (eg, warfarin) as having a role in the etiology of MS.6 This is particularly relevant in patients who have chronic kidney disease and take warfarin or other vitamin K antagonist anticoagulants to prevent atrial fibrillation.6,7 In many of these patients changes to the arterial blood vessels occur because of an alteration in the regulation of calcium and phosphate homeostasis, leading directly to vascular smooth muscle cell changes.5 Contrastingly, MS has also been found to occur in individuals in the absence of any medical condition and is thought to be due possibly to aging.1
The pathological significance of MS has been reported with different commentaries. Some authors believe the condition has minimal clinical significance, while others cite evidence for changes in the physiology and functioning of affected arteries.4,5,7 Such changes result from the loss of elastic fibers in the medial layer, which then leads to arterial stiffness3,5 and ultimately impaired perfusion increasing the risk of peripheral vascular disease, cardiovascular, renal, and cerebral morbidities and mortalities.1,2,4,5,7,8
MS is usually recognized as an incidental finding on plain film radiographs and can be confirmed by histological diagnosis or hemodynamic studies.2,7 A feature that distinguishes this type of vascular calcification from other vascular calcifications, such as atherosclerosis, is the exclusive, pathological calcification of the medial layer.1,3 The calcification is diffuse and circumferential without any decrease in the diameter of the arterial lumen.5,7 The medial lesion calcifies early in its development and no inflammatory molecular cascades are involved. This early calcification and lack of inflammatory response distinguishes it from lesions of atherosclerotic origin.1,3,5
Because there have been previous reports of this condition presenting in the head and neck region in a population of patients that are at risk of cardiovascular and cerebral complications, it is relevant and valuable for a dental practitioner to be able to recognize and identify this type of condition on dental radiographs.1,3,7 This recognition is important so that appropriate steps may be taken to ensure a timely referral to the patient's medical physician for further investigation and management.
Case Report
An 89-year-old male patient presented to Midwestern University College of Dental Medicine, Glendale, Arizona, with a chief complaint requesting extraction of his remaining four mandibular anterior teeth and fabrication of a lower denture. At his initial appointment, he presented with a panoramic dental radiograph from an outside general dental office. He presented with a full maxillary denture and no mandibular prosthesis. The exact number of years he had worn his maxillary denture was unreported as was use of a mandibular prosthesis. Due to moderate alveolar ridge loss, it was estimated the patient had been completely edentulous in the maxillary arch for many years. There was no report of lifelong routine dental care.
His medical history included arthritis in his hands, back, and shoulders; dizziness and occasional fainting when getting up too quickly; high blood pressure; and removal of kidney stones two months prior. He had no history of alcohol or drug abuse, no other reported medical conditions, and a BMI of 25.8, putting him slightly in the overweight category. His medications included benazepril 10 mg, atorvastin 40 mg, and a history of allergies to sulfa and tetracycline. His initial vital signs were blood pressure 134/75 mm Hg and resting heart rate 70 beats per minute.
An initial comprehensive evaluation revealed root caries on teeth Nos. 22, 23, and 26 with a retained root tip at the area of No. 25 in addition to an edentulous maxilla with moderate loss of alveolar bone height. There was no report of a previous mandibular partial denture. Radiographic evidence of woven bone remodeling was noted in multiple mandibular posterior socket sites.
His original panorex from a local private office was of moderate quality and showed no evidence of arterial sclerosis. Definitive imaging of his mandibular anterior region was poor, and after his clinical examination it was decided to capture digital periapical radiographs of Nos. 22 through 26 using a Progeny® dental x-ray system (Preva DC Intraoral X-Ray, Midmark, midmark.com) with a DentiMax (dentimax.com) intraoral sensor at a setting of 7 mA, 60 kVp, and 0.100 seconds. The periapical radiographs revealed root caries, significant loss of alveolar bone height, and a periapical radiolucency at No. 23; all teeth were deemed nonrestorable. There was no evidence of MS in the peripical radiographs.
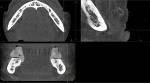
Because of the possibility of future implant placement, a CBCT dental scan was obtained of the mandibular arch using a 3D Accuitomo system (J Morita, morita.com) at 8 mA, 90 kVp, and 17.5 seconds.The scan was reconstructed at a size of 0.25 mmand interpreted by a board-certified oral and maxillofacial radiologist. Radiographic interpretation revealed partially edentulous dentition with generalized mild to moderate horizontal bone loss, multiple sites of bone remodeling in the mandibular arch, carious teeth Nos. 22, 23, and 26 with a retained root tip of No. 25. Incidental findings revealed bilateral radiopacities with a tortuous course inferior and buccal to the mandibular body. These opacities were positioned at the areas consistent with the right and left facial arteries, which represent MS. In addition, smaller and fainter calcifications also representing MS were identified within the floor of the mouth, possibly representing lingual arteries (Figure 1). MS was also noted adjacent to the mandibular body (Figure 2 and Figure 3). Prompt recognition with appropriate referral for follow-up care may assist this patient to evaluate for further preventative measures.
Three comprehensive dental treatment plans and alternatives were recommended. These options included no treatment; extraction of all remaining dentition and fabrication of a conventional tissue-supported denture replacement for the mandibular arch; or extraction of all remaining dentition, placement of endosteal implants, and fabrication of an implant-supported mandibular overdenture. After a CBCT was captured and treatment alternatives, risks, and benefits were reviewed, the patient preference was a mandibular implant-retained overdenture.
Discussion
Vascular calcifications are pathologic lesions that may be discovered as incidental findings on radiographs during medical and dental examinations.1-3 These lesions can be categorized into two distinct groups: those presenting in the tunica intima and those of the tunica media layers of a blood vessel wall. The lesions of the tunica intima are associated with atherosclerotic plaque accumulation and are inflammatory in nature, resulting in the narrowing of the blood vessel lumen.1 In contrast, lesions of the tunica media are associated with specific systemic conditions, including diabetes mellitus, end-stage renal disease, and disorders of calcium and phosphate metabolism. Lesions of the tunica media tend to have a greater incidence in males and are seen in advancing age.1,5
The lesions of the medial wall are considered a specific entity known as Mönckeberg arteriosclerosis (MS). The pathological basis of the lesion is an example of dystrophic calcification of the medial walls (tunica media) of small- and medium-sized arteries,1,2 although it has been reported that limitation to the medial walls is disputed.8 The tunica media of the arterial wall is composed of vascular smooth muscle and elastic fibers,1,5 which can undergo calcification as a result of deposition of hydroxyapatite.5,7 This calcification process has been tested and demonstrated to be linked to a reduction in proteins responsible for inhibition of medial wall calcification.5,7,9
Disease progression of MS from early-stage calcific deposits (stage 1) to final small bone formation (stage 4) is well documented.5 These medial wall calcifications result from a change in vascular smooth muscle cells into osteoblast-like cells, which are evident in the mineralization process.10 The mediators responsible for calcification are not considered inflammatory by nature.5 Some investigators, however, propose alternative mediators, including abnormal vascular smooth muscle cells with osteoblastic potential and protein modulators for bone mineralization.11
The prevalence of MS in a long-term study population exhibited 6.9% in females and 13.3% in males. Interestingly, these percentages did not increase with age.8,10 Other studies estimated MS at 0.5% of the population with 3:2 ratios of men to women.5 Increased incidence is seen in individuals with long-standing type 2 diabetes and end-stage renal disease.5
The clinical significance of MS is the active pathological calcification of the tunica media of blood vessels, leading to arterial stiffness that results in increased pulse pressure and reduced arterial compliance.1,8 The arterial stiffness is an independent predictor of cardiovascular mortality.6 This type of calcification is even more significant in patients with systemic diseases because it can exacerbate the pre-existing condition, further increasing the patient's risk of cardiovascular and cerebral complications. MS has also been reported in the development of peripheral artery disease in diabetic patients.7 In patients with chronic kidney disease, elevated levels of phosphate and calcium are key components in the development of the medial calcification.5,8
The arterial locations where MS has been identified varies with the most common being the lower extremities.4,11-13 Other reported arteries are ulnar and radial,14 facial,1 infraorbital,4 coronary,15 and temporal,12,15,16 and it has been seen rarely in soft tissues,4 although one such report of pharyngeal soft tissue was documented.9
Blood vessels that are affected by MS have very distinct radiographic features.1,2,17 Radiographically, MS is commonly described as having a ring-like, pipeline, or train track appearance.4,12 In contrast, vascular calcifications of atherosclerotic origin are reported to have a splotchy appearance.4 Dental radiographic evidence of MS had previously been detected in panoramic,1,18,19 periapical,18 and bitewing radiographs.1,19 In the present case the authors were able to clearly demonstrate MS, which was not originally evident on a copy of a plain film panorex captured in the patient's general dental office. Thus, dental radiographic evidence of MS has now been detected in CBCT images.
In the absence of the original plain film panorex, the copied panorex from the patient's general dentist rendered little radiographic detail. Two periapical radiographs of the mandibular anterior area were captured to assist in diagnosis of the patient's remaining dentition. Since the anterior area was not a location of the facial arteries, these two periapical images showed no evidence of MS. Periapical radiographs of the premolar and molar areas would be the most appropriate type of radiographs to show evidence of the facial arteries. A CBCT was required for comprehensive evaluation of the extent of alveolar bone loss and to evaluate for future implant sites. This scan provided the opportunity to recognize and inform the patient of his vascular calcifications.
This case report highlights many characteristics consistent with MS. The patient's history of renal compromise with recent removal of kidney stones, high blood pressure, high cholesterol, male gender, and advanced age are classic incidental findings associated with Mönckeberg arteriosclerosis.
Conclusion
MS has been widely researched in medical literature, and its incidental findings on dental radiographic examination warrants follow-up. In otherwise undiagnosed and asymptomatic patients, early detection should lead to further investigation thereby decreasing risk of serious future medical complications.
In this case report, bilateral calcifications in the facial arteries were described, and the authors believe these are the first to be reported using CBCT. The presence of these railroad or "train track" calcifications should alert the dental practitioner to the possibility of a more serious underlying systemic problem and referral to an appropriate medical specialist.
About the Authors
Karen Berrigan, DMD,MS
Clinical Assistant Professor, Orthodontic Clinic, College of Dental Medicine - Arizona, Midwestern University, Glendale Arizona
Sabita Rao, DMD
Clinical Assistant Professor, Pediatric Dentistry, College of Dental Medicine - Arizona, Midwestern University, Glendale Arizona
John R. Francis, DDS, MS
Assistant Clinical Professor, Department of Surgery, College of Dental Medicine - Arizona, Midwestern University, Glendale Arizona
Douglas W. Beals, DDS, MS
Assistant Professor and Director of Clinical Faculty, College of Dental Medicine - Arizona, Midwestern University, Glendale Arizona
Vijay Parashar, BDS, DDS, MDSc
Professor, Oral and Maxillofacial Radiologist, College of Dental Medicine - Arizona, Midwestern University, Glendale Arizona
References
1. Tahmasbi-Arashlow MK, Barghan S, Kashtwari D, Nair MK. Radiographic manifestations of Mönckeberg arteriosclerosis in the head and neck region. Imaging Sci Dent. 2016;46(1):53-56.
2. Castling B, Bhatia S, Ahsan F. Mönckeberg's arteriosclerosis: vascular calcification complicating microvascular surgery. Int J Oral Maxillofac Surg. 2015;44(1):34-36.
3. Omami G. Monckeberg arteriosclerosis: a telltale sign. J Oral Maxillofac Surg. 2017;75(11):2383-2384.
4. Frazier JJ, Casian R, Benson BW. Mönckeberg medial calcinosis of the infraorbital arteries: a first case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(2):e31-e35.
5. Lanzer P, Boehm M, Sorribas V, et al. Medial vascular calcification revisited: review and perspectives. Eur Heart J. 2014;35(23):1515-1525.
6. Wahlqvist ML, Tanaka K, Tzeng BH. Clinical decision-making for vitamin K-1 and K-2 deficiency and coronary artery calcification with warfarin therapy: are diet, factor Xa inhibitors or both the answer? Asia Pac J Clin Nutr. 2013;22(3):492-496.
7. Ho CY, Shanahan CM. Medial arterial calcification: an overlooked player in peripheral arterial disease. Arterioscler Thromb Vasc Biol. 2016;36(8):1475-1482.
8. Micheletti RG, Fishbein GA, Currier JS, Fishbein MC. Mönckeberg sclerosis revisited: a clarification of the histologic definition of Mönckeberg sclerosis. Arch Pathol Lab Med. 2008;132(1):43-47.
9. Barra Couri CE, da Silva GA, Baddini Martinez JA, et al. Mönckeberg's sclerosis - is the artery the only target of calcification? BMC Cardiovasc Disord. 2005;5:34.
10. Byon CH, Chen Y. Molecular mechanisms of vascular calcification in chronic kidney disease: the link between bone and the vasculature. Curr Osteoporos Rep. 2015;13(4):206-215.
11. Pisani I, De Troia A, Allegri L, et al. Malignant Mönckeberg medial calcific sclerosis. Intern Emerg Med.2018;13(4):615-617.
12. Top C, Cankir Z, Silit E, et al. Monckeberg's sclerosis: an unusual presentation - a case report. Angiology. 2002;53(4):483-486.
13. Shanahan CM, Cary NR, Salisbury JR, et al. Medial localization of mineralization-regulating proteins in association with Mönckeberg's sclerosis: evidence for smooth muscle cell-mediated vascular calcification. Circulation. 1999;100(21):2168-2176.
14. Naha K, Shetty RK, Vivek G, Reddy S. Incidentally detected Monckeberg's sclerosis in a diabetic with coronary artery disease. BMJ Case Rep. 2012;2012:bcr2012007376.
15. Swami SY, Gadkari RU, D'Acosta G. Monckeberg's medial calcification in coronary arteries: three case reports. Ann Trop Med Public Health. 2014;7(1):80-82.
16. Castillo BV Jr, Torczynski E, Edward DP. Monckeberg's sclerosis in temporal artery biopsy specimens. Br J Ophthalmol. 1999;83(9):1091-1092.
17. Kadoya,Y Yanishi K, Matoba S. Rail-tracking calcification of lower limb arteries. Clin Case Rep. 2018;6(9):1921-1922.
18. Shahid K, Weng S, Cook L, Syed AZ. Detection of Monckeberg medial sclerosis on conventional dental imaging. J Mich Dent Assoc. 2017;99(3):40-42,68-69.
19. Kröger K, Stang A, Kondratieva J, et al. Prevalence of peripheral arterial disease - results of the Heinz Nixdorf recall study. Eur J Epidemiol. 2006;21(4):279-285.