Digital Workflow as an Aid to Complex Multidiscipline Dental Treatment for Improved Esthetics
Abstract: Complex treatment frequently requires the often challenging task of cohesively melding multiple disciplines of dentistry. The use of a digital workflow aids in simplifying the flow of treatment from start to finish, allowing the clinician to design esthetic outcomes and occlusion first virtually, communicate these esthetic designs to the patient, and then transmit digital files to chairside milling and printing devices as well as to dental laboratories for permanent restoration fabrication. In the complex implant case presented, the benefits of a digital workflow, including efficient soft-tissue management and streamlined fabrication of custom abutments—keys to achieving the patient’s desired esthetic goals—are demonstrated.
Fred A. Puccio, DDS; and Gregori M. Kurtzman, DDS
Patients often present with restoration goals that require complex care utilizing treatment in multiple areas of dentistry. A digital workflow can simplify the restorative process, allowing the use of virtual smile design to preview the proposed end-result of the patient's expressed esthetic goals and to plan the treatment steps, including creation of provisional restorations and final prosthetics.1,2 Smile design is a facially generated process used to develop an esthetic smile that blends with that particular patient's face.3,4
The use of intraoral scanning instead of traditional analog impressions has paved the way for the digital workflow to provide an easier, more streamlined process than conventional methods.5 It permits communication of the scan files to software for smile design and with laboratories for design and fabrication of the various restorative elements, including orthodontic aligners, surgical guides, implant custom abutments, provisional prosthetics, and final crowns. Practitioners who print and/or mill in-office are able to further accelerate the digital workflow process. Additionally, the digital workflow has been reported to increase patient overall case satisfaction.6,7
The following case presentation illustrates the benefits of a digital workflow of a complex case that incorporated multiple areas of dental care to achieve the patient's desired esthetic goals.
Case Presentation
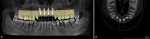
A 65-year-old male patient presented for a comprehensive examination and expressed interest in improving his smile. He stated that his "front teeth are too big and long." He also commented on his lack of gum display. Radiographs were taken, and it was noted that teeth Nos. 8 through 10 had prior endodontic treatment, and single crowns were present on teeth Nos. 6 and 9 through 11. A ceramic three-unit bridge was present on teeth Nos. 6 through 8 (Figure 1). The connector between Nos. 6 and 7 was fractured. A large post was noted in tooth No. 8 with no evident tooth structure coronally, and there appeared to be restorative material around the coronal aspect of the post. A fracture was noted on tooth No. 10 at the apical end of the post present in the tooth. The patient was scheduled to return to discuss a treatment plan after evaluation of the clinical findings.
Treatment Plan
The patient returned to review the proposed treatment plan. Tooth No. 8, one of the abutment supports of the ceramic bridge on Nos. 6 through 8, had a fracture at the gingival margin (Figure 2). The treatment plan was discussed and would include aligner orthodontics to open the vertical dimension of occlusion (VDO), as the bite had collapsed over time, and achieve proper canine guidance. Extraction of the residual root at No. 8 along with extraction of teeth Nos. 9 and 10 would be performed, with placement of a provisional bridge at Nos. 6 through 11 during treatment. Implants would be placed at sites Nos. 7 through 10.
Following implant integration, the implants would be restored. Custom abutments would be placed on the implants at uncovery, and lithium-disilicate crowns (IPS e.max® CAD, Ivoclar, ivoclar.com) would be placed on Nos. 6 through 11 as provisional restorations to enable soft-tissue remodeling and allow the patient to "test-drive" the esthetics before fabrication and placement of final ceramic crowns. In addition, porcelain veneers would be placed on teeth Nos. 4, 5, 12, and 13 to complete the smile and balance the negative space in the buccal corridors. Teeth whitening would be done on the lower arch with composite resin bonding to restore worn incisal edges on teeth Nos. 22 through 27.
The patient agreed to the planned treatment, and both arches were scanned with an intraoral scanner (Primescan, Dentsply Sirona, dentsplysirona.com) in preparation for the initiation of treatment.
Orthodontics, Provisional Bridge, Implant Planning
Additional digital scans were also captured using the iTero™ Element™ 5 intraoral scanner (Align Technology, Inc., itero.com) and exported to the Invisalign Doctor Site (Align Technology, Inc., invisalign.com), and teeth Nos. 7 and 8 were digitally added using ClinCheck® software (Align Technology, Inc.) (Figure 3). Aligners (Invisalign) were fabricated to achieve the established goals of increasing the VDO and better positioning the posterior teeth esthetically. Orthodontic treatment with the aligners was completed over a 40-week period.
Both arches were scanned again (Primescan) and a six-unit temporary bridge from Nos. 6 through 11 was designed (Primescan chairside CAD/CAM) (Figure 4) and milled (CEREC® Primemill, Dentsply Sirona) using a polymethyl methacrylate (PMMA) block prior to the extractions. The residual root at No. 8 and teeth Nos. 9 and 10 were extracted with the patient under local anesthetic, and socket preservation was achieved by grafting with allograft putty (RegenerOss®, ZimVie, zimvie.com) in preparation for implant placement following a 3-month maturation period. Teeth Nos. 6 and 11 were prepared for crowns for a six-unit provisional bridge, which was inserted intraorally and luted in with temporary cement (TempBond™, Kerr, kerrdental.com) (Figure 5).
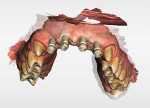
After 3 months of maturation of the allograft putty bone graft with the surrounding host tissues, it was determined that implant placement could be initiated. The provisional bridge was removed to allow scanning (Primescan) of the upper and lower arches for design and fabrication of a surgical guide for implant placement (Figure 6). Using a biocopy of the existing temporary bridge, the clinician designed teeth proposals for teeth Nos. 8 through 10. Accurate proposals with emergence and tooth positions and proportions were needed to aid in the implant planning. A cone-beam computed tomography (CBCT) scan (ORTHOPHOS XG 3D, Dentsply Sirona) of the patient was obtained. The model scans with the teeth proposals were merged with the CBCT and imported into implant planning software (SICAT Implant, SICAT GmbH & Co. KG, sicat.com). Implants were virtually placed at sites Nos. 7 through 10 with respect paid to the available osseous anatomy. Special attention was placed on the distances between the implants themselves and the natural teeth Nos. 6 and 11 to allow for the optimum esthetic result (Figure 7), as tissue development is dependent on proper implant placement.8 A classical surgical guide that was based on the implant planning was then designed (SICAT) and milled with metal guide sleeves in place to be used with the implant system guided kit (Astra Tech Implant System® EV, Dentsply Sirona).
Implant Placement and Restorative Phase
Upon presenting for the implant surgical appointment, the patient reviewed and signed consent forms, and local anesthetic was administered. The surgical guide was tried in to verify its fit on the maxillary dentition adjacent to sites Nos. 7 through 10 (Figure 8 and Figure 9). A flapless approach using tissue punches was utilized. Osteotomies were performed through the surgical guide to accommodate 3.6 mm x 13 mm straight implants (Astra Tech EV) at each of the four sites (Nos. 7 through 10). Cover screws were placed, and a radiograph was recorded to document the implant placement positions (Figure 10). The provisional bridge was reinserted and luted in with temporary cement (TempBond).
After 3 months of implant healing and integration, the patient returned for the start of the restorative phase of implant treatment. Local anesthetic was administered, and the surgical guide was inserted intraorally to identify the location of the covered areas over each implant. An all-tissue dental laser (Waterlase iPlus®, Biolase, biolase.com) was used through the surgical guide to uncover the cover screw at each implant. Scan bodies (Atlantis IO FLO, Dentsply Sirona) were placed on each implant (Figure 11), and the arch was scanned (Primescan). Healing abutments were placed on each implant (Figure 12). The provisional bridge was modified to allow it to seat over the healing abutments and was luted in with temporary cement (TempBond), and the patient was dismissed. The scans of the arch with scan bodies and the biocopies of the provisional prosthesis were transmitted to the implant and scan body manufacturer (Atlantis/Dentsply Sirona) via CEREC® AC Connect software (Dentsply Sirona) for fabrication of custom titanium gold-colored implant abutments (Figure 13).
The implant/scan body manufacturer virtually designed the abutments and communicated with the clinician for approval of the virtual design (Figure 14). The abutments were then milled from titanium and gold coated and returned to the clinician. Once the custom abutments were designed and approved the practitioner obtained a core file from the manufacturer. This file can be exported back into the intraoral scanner (Primescan) or other CAD/CAM system for the design and manufacture of the temporary or permanent restorations. This core file is a virtual model with the custom abutments virtually seated as designed. In this case, the clinician 3D-printed (Primeprint, Dentsply Sirona) a Geller model to aid in adjusting and finishing the provisional restorations to help further develop the tissue prior to creation of the permanent restorations (Figure 15). A Geller model incorporates spaces to receive an individual die at each unit planned for fixed prosthetic units on the arch. The model, which was printed using model resin, was fabricated to have removable individual dies for each abutment (Nos. 7 through 10) and planned crown on the natural canines (Nos. 6 and 11) to aid in the fabrication of the planned provisional ceramic crowns (Figure 16).
Before receiving the custom abutments, the clinician used the core file sent from Atlantis (Figure 17, A and B) to design virtual crowns for each of the six anterior teeth (Figure 17, C). The core file gets imported back into the chairside software of the intraoral scanner (Primescan). Once the six crowns were designed, they were sent to the mill (Primemill) for milling of each individual crown (Figure 17, D). The crowns were milled from IPS e.max® CAD LT blocks (Ivoclar) in shade A2 on the Primemill, then glazed in a sintering oven (CEREC® SpeedFire, Dentsply Sirona). Final adjustments were made and finished on the previously printed Geller model (Figure 18).
The custom abutments were returned from the lab, and the patient was appointed. The healing abutments were removed, and the custom abutments were inserted at the appropriate sites. The implant screws were torqued to 25 Ncm and the access holes covered with Teflon tape and composite resin (Figure 19 and Figure 20). The individual provisional lithium-disilicate crowns were then inserted on Nos. 6 through 11 and luted in with temporary cement (TempBond) (Figure 21). These provisional crowns would facilitate soft-tissue maturation, particularly around the implant restorations prior to fabrication of the final restorations.
Final Restorations
The patient returned 6 weeks later for the final restorative phase. No inflammation was noted on the gingival tissue, which appeared healthy. The provisional crowns were removed and the arch was scanned (Primescan), and the scans were transmitted to the lab for fabrication of the final ceramic restorations. Teeth Nos. 4, 5, 12, and 13 were prepared for porcelain veneers. The patient was temporized again until the final restorations were completed.
The final restorations consisted of IPS e.max pressed crowns (Ivoclar) on natural teeth Nos. 6 and 11 and implants Nos. 7 through 10, and IPS e.max pressed veneers (Ivoclar) on teeth Nos. 4, 5, 12, and 13. The restorations were luted in with adhesive cement (Variolink® Esthetic DC and LC, Ivoclar). The lab provided an esthetic result that afforded the satisfied patient a youthful smile (Figure 22 and Figure 23).
Discussion
In cases involving complex treatment plans where various areas of dental care are required to achieve the patient's desired goals, planning is often the key to success. In such cases, clinicians should begin with the end in mind. Digital workflows aid in this process by allowing the clinician to design esthetic outcomes and occlusion first virtually, communicate these esthetic designs to the patient, and then transmit digital files to chairside milling and printing devices as well as to various labs for permanent restoration fabrication.
Soft-tissue management is an important aspect of achieving these desired esthetic goals. It becomes even more important when teeth will be replaced by implants or implants will be placed in edentulous spaces. Soft-tissue management requires multiple steps to develop supporting gingiva to ensure that papillae are present and a natural esthetic result is achieved. This also may require osseous grafting to develop proper bony contours to support the soft tissue. When failing teeth are to be extracted, socket grafting may be a more prudent approach than immediate implant placement, as the osseous anatomy is developed to a more ideal state.
Virtual planning for implant positioning with guided surgical placement based on the patient's anatomy allows optimal implant positioning in coordination with the virtual smile design. Utilization of custom abutments with virtual planning then provides idealized bases for the planned crowns and helps achieve the desired esthetic goals.9,10
Such custom abutments allow development of emergence profiles and soft tissue to provide natural-looking esthetics. The case presented utilized lithium-disilicate glass-ceramic provisional restorations placed simultaneously with the custom abutments to develop the soft tissue prior to fabrication of the final restorations. Dental papillae immediately began to form once tissue pressure was applied by the abutments and temporaries. In the authors' experience, glass-ceramic with mechanically polished margins is better tolerated by the developing soft tissue than traditional provisional materials that are acrylic in nature. The CAD ceramic provisional restorations used in this case provided a smooth "glass-like" surface with which the gingiva was in contact to achieve non-inflamed, stable soft tissue. This approach also allows the patient to "test-drive" the esthetics that the final restorations will mimic. Patients can then offer input regarding any changes they desire or concerns they may have, which can be incorporated into the final restorations.
The lab-manufactured final crown and veneer restorations (New-Dent Aesthetics dental lab) were fabricated of IPS e.max (pressed) via electronic transmission of the photographs, STL files, core file, and 3D-printed models. The lab customized the restorations to blend in a beautiful, harmonious esthetic result.
Conclusion
Digital workflows aid in simplifying complex, multidisciplinary treatments from start to finish. The authors propose that digital dentistry is better, safer, and faster for patients. Additionally, working with digital dentistry suppliers that offer turnkey solutions that include all aspects of the digital treatment, ranging from orthodontic clear aligners, CAD/CAM chairside design and milling, CBCT, and implant planning and surgical guide fabrication, to 3D printing, allows a simple, seamless one-button workflow. Virtual design allows practitioners to custom-design the esthetics and let patients preview it and offer feedback to customize the look to meet their expressed esthetic goals.
ACKNOWLEDGMENT
The authors thank Laurence Passaro, CDT, and his team at New-Dent Aesthetics dental lab, New York, NY, for the final restorations in this case.
ABOUT THE AUTHORS
Fred A. Puccio, DDS
Clinical Adjunct Instructor, Department of Cariology and Comprehensive Care, Honors Aesthetics Clinic, New York University College of Dentistry, New York, New York; Certified Advanced Patterson Dental Digital Trainer; Private Practice, Wyckoff and Garfield, New Jersey
Gregori M. Kurtzman, DDS, MAGD
Former Assistant Clinical Professor, University of Maryland School of Dentistry, Baltimore, Maryland; Diplomate, International Congress of Oral Implantologists; Private Practice, Silver Spring, Maryland
REFERENCES
1. Coachman C, Bohner L, Jreige CS, et al. Interdisciplinary guided dentistry, digital quality control, and the "copy-paste" concepts. J Esthet Restor Dent. 2021;33(7):982-991.
2. Moshman AT. 3D printing technologies and protocols to enhance the dental workflow. Compend Contin Educ Dent. 2021;42(5):e1-e4.
3. Spear FM, Kokich VG. A multidisciplinary approach to esthetic dentistry. Dent Clin North Am. 2007;51(2):487-505, x-xi.
4. Thomas PA, Krishnamoorthi D, Mohan J, et al. Digital smile design. J Pharm Bioallied Sci. 2022;14(suppl 1):S43-S49.
5. Almalki A, Conejo J, Wünsche A, et al. Digital smile design and fabrication of CAD/CAM restorations in a complex esthetic case. Compend Contin Educ Dent. 2022;43(10):664-668.
6. Gollner MG. Digital transformation: analog expertise and digital optimization. Int J Comput Dent. 2022;25(4):407-419.
7. Guichet DL. Digital workflows in the management of the esthetically discriminating patient. Dent Clin North Am. 2019;63(2):331-344.
8. Zadeh HH. Implant site development: clinical realities of today and the prospects of tissue engineering. J Calif Dent Assoc. 2004;32(12):1011-1020.
9. Chu SJ, Tarnow DP, Tan JHP, Stappert CFJ. Papilla proportions in the maxillary anterior dentition. Int J Periodontics Restorative Dent. 2009;
29(4):385-393.
10. Hochman MN, Chu SJ, Tarnow DP. Maxillary anterior papilla display during smiling: a clinical study of the interdental smile line. Int J Periodontics Restorative Dent. 2012;32(4):375-383.