Peri-implantitis and the Effect of the Implant Surface at Placement
Scott D. Ganz, DMD; Dirk U. Duddeck, DDS; and Gregori M. Kurtzman, DDS, MAGD
Modern root-form endosseous dental implants have been used to successfully replace missing teeth for more than four decades. The implant industry has grown substantially during this time, with many hundreds of dental implant manufacturers providing components for clinicians around the globe. Increased acceptance of dental implants has greatly amplified the number of dental implants placed worldwide.
As the dental implant patient population continues to age, long-term follow-up after implant placement has become increasingly important due to various factors associated with the condition and maintenance of implants placed. Although dental implants exhibit a high success rate as a medical device, their life expectancy may be limited depending on the patient's changing health, use of medications, lifestyle changes, nutrition, occlusal/bite issues, loss of additional teeth, experiences of trauma, lack of sufficient keratinized soft tissue, loss of bony support, and oral hygiene habits. When loss of soft-tissue coverage and/or bone occurs, the resultant inflammation surrounding the implant is known as peri-implantitis.
Understanding the Disease
Peri-implantitis is a pathological process that occurs in hard tissues surrounding dental implants. It is characterized by inflammation of the soft and hard tissues adjacent to the implant leading to progressive loss of supporting bone around the implant and, when not treated early enough, eventual loss of the implant. Peri-implantitis may originate at implant placement or later after restoration of the implant, and progress slowly or in an accelerated manner.
As peri-implantitis has been more closely examined in recent years, the increase in reported incidence has been due not to growing case numbers, but to more frequent identification as practitioners come to understand the signs and symptoms associated with the disease.1 The histological and clinical conditions leading to the conversion from gingival inflammation to peri-implantitis are not completely understood.2 Clinically at the histologic level, sites that have peri-implantitis often have larger inflammatory lesions than sites around natural teeth that have periodontitis. Evidence suggests that progressive crestal bone loss around implants in the absence of clinical signs of soft-tissue inflammation is rare.2
Peri-implant disease is classified into two categories: peri-implant mucositis and peri-implantitis. Peri-implant mucositis is classified when inflammation is found only around the soft tissues adjacent to the dental implant, with no evidence of bone loss. Generally, peri-implant mucositis is a precursor to peri-implantitis and may be successfully treated to prevent progression to peri-implantitis. In peri-implantitis, the gingival inflammation has progressed, leading to deterioration of the bone supporting the implant. Peri-implantitis typically requires surgical treatment to stop its progression and repair the lost hard tissues. Therefore, the key is timely identification of peri-implant mucositis and early intervention to prevent its progression to the hard tissues supporting the implant.
As with natural teeth, implants require regular homecare to maintain the soft tissue, which acts as a barrier to deeper progression of inflammatory factors. Other risks factors for developing peri-implant disease include previous periodontal disease diagnosis, poor plaque control, smoking, and diabetes. Dental implants need to be routinely monitored as part of a comprehensive periodontal evaluation.1
The reported occurrence of peri-implant mucositis and peri-implantitis ranges in studies from 46% to 63% and 19% to 23%, respectively. Individuals who undertake regular personal homecare and professional maintenance therapy manifest reduced occurrences of these diseases compared with patients who have irregular supportive therapy.3-5 Thus, based on the literature, peri-implant diseases affect a significant number of patients who have implants. Therefore, it is necessary to understand diagnosis of these diseases and the risk factors that can be modified to reduce the potential for disease occurrence or progression.
Contributors to Peri-implant Disease
In examining the incidence of peri-implant diseases, reports have shown that 90% of peri-implant tissues had some form of inflammatory response, and the prevalence of peri-implantitis ranged from 28% to 51%.6
Evidence has shown that there is an increased risk of the development of peri-implantitis in patients who have a history of chronic periodontitis and poor plaque control skills and who fail to maintain regular maintenance care after implant treatment. Studies have reported that smokers have a high incidence of peri-implantitis (72.7%) compared to non-smokers (27.3%). Significantly higher richness of the microbiota was identified in patients with peri-implantitis who are smokers.7,8 Another significant variable is that patients with periodontitis demonstrated a 50% chance of having peri-implantitis.9,10 Patients who have inflammatory changes in the mouth associated with their remaining natural teeth are at a much greater risk of acquiring peri-implantitis because of the bacteria present that is causing the periodontal issues. Additionally, oral biofilm in periodontally involved patients may make them more immunologically sensitive to further insult from particles that are present around or on the implant surface.
Systemic diseases such as arterial hypertension, diabetes mellitus, osteoporosis, and cardiovascular diseases do not show a statistically significant influence on the incidence of peri-implantitis. Modification of those risk factors, which may include improving homecare, treating periodontal issues, and addressing systemic health issues (eg, diabetes), can aid in decreasing peri-implantitis incidence and its severity when identified.5
Sterile but Contaminated Implants:
An Understated Risk Factor
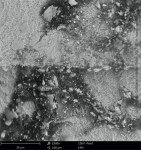
The actual manufacturing, sterilization, and packaging of a dental implant are largely underestimated factors that can affect the short- and long-term condition of the implant. How the implant is made and packaged can influence how surrounding bone interacts with the implant's surface during or after integration. The manufacturing process must be meticulous in all phases to ensure that the end-product is sterile and completely uncontaminated. Although the implant is sterile when removed from the package from the manufacturer, organic and/or non-organic particles on the implant's surface that are directly related to the manufacturing process may be present (Figure 1).11
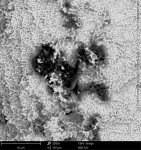
In particular, organic carbonaceous foreign materials (Figure 2) have been associated with peri-implant bone loss and peri-implantitis.12 Exposure of bone to foreign particles activates macrophages to secrete pro-inflammatory cytokines, such as tumor necrosis factor-α, interleukin (IL)-1b, IL-6, and prostaglandin E2, which, in turn, stimulates the differentiation of osteoclast precursors into mature osteoclasts. The increased osteoclast activity associated with a foreign-body reaction may result in peri-implant bone resorption (Figure 3).13 Foreign materials 0.2 µm to 7.2 µm in size are especially classified as pro-inflammatory.14-16 If such particles detach from the implant surface during the implant insertion process, macrophages take up the particles by phagocytosis and subsequently release pro-inflammatory cytokines, which also leads to the expression of matrix metalloproteinase (MMP-8). The result is an expanding zone of soft-tissue damage and inflammation.13
Quality assessment studies on dental implants conducted by the CleanImplant Foundation in collaboration with Charité University in Berlin and the Sahlgrenska Academy in Gothenburg, Sweden, used scanning electron microscopy (SEM) to identify impurities on sterile-packaged dental implants. Findings of particulate contamination were reported for both titanium and zirconia (ceramic) implants specific to the process used during the manufacture and packaging of those implants.11,17 Reported data demonstrated that one out of three implant systems analyzed contained significant amounts of impurities that are technically avoidable. Those contaminants included organic particles from the manufacturing process, metallic particles of nickel, tungsten, iron, copper, and chromium from the milling or surface treatment process, and plastic from handling and packaging.
SEM images of titanium implants showed not only isolated spots of impurity, but also larger areas of the implant surface that were either insufficiently cleaned in the production process chain or contaminated without being noticed during packaging of the implants. Under high magnification in the SEMs, organic carbonaceous particles appeared as black spots (Figure 4 through Figure 7). The SEM images in low (500x) and high magnification (2,500x) revealed thermoplastic materials, synthetic polymers, and polysiloxanes on sterile implant surfaces. Ceramic implants also demonstrated organic debris related to manufacturing, as some that were analyzed following removal from the manufacturer's packaging exhibited large amounts of predominately organic carbonaceous residue when viewed under SEM (Figure 8 through Figure 11).17
All of the implants with reported significant impurities carried the CE mark or had US Food and Drug Administration clearance. Ultimately, contaminated medical devices, even in sterile packaging, can be harmful to patients and lead to implant failure related to peri-implantitis stemming from inflammatory reactions to those impurities.
Conclusion
As the use of dental implants continues to proliferate worldwide, patients receiving these devices need to be carefully monitored during the lifetime of the restoration. Early identification of peri-implant mucositis and intervention is key to preserving the bone surrounding the implant, preventing progression to peri-implantitis, and improving long-term clinical results. Peri-implantitis is more prevalent than previously accepted as dental practitioners gain more understanding of the signs and symptoms of this inflammatory disease. Factors that contribute to peri-implant disease include smoking, certain systemic health issues such as uncontrolled diabetes, and lack of follow-up.
The quality of the implant surface may also play a role in peri-implant disease. Whether made of titanium or ceramic, the implant's surface must be free of foreign particles after removal from the sterile packaging. These particles are not visible to the naked eye or with magnifying glasses. While in most cases of peri-implantitis or implant loss clinicians assume the problem lies with the patient, the analysis results of sterile-packaged implants as cited earlier suggest that the medical device in use should also be considered as a possible cause for an inflammatory reaction and potential trigger of peri-implantitis upon insertion. Clinicians can be assured they are using a sterile and clean implant after a thorough SEM analysis has proven cleanliness across different batches of the implant product and sufficient clinical documentation stating so is made available.18,19
DISCLOSURE
Dr. Ganz is a member of the CleanImplant Foundation scientific advisory board. Dr. Duddeck is Managing Director of the CleanImplant Foundation. Dr. Kurtzman had no disclosures to report.
ABOUT THE AUTHORS
Scott D. Ganz, DMD
Adjunct Assistant Professor, Department of Restorative Dentistry, Rutgers School of Dental Medicine, Newark, New Jersey; Private Practice in Maxillofactial Prosthetics and Implant Dentistry, Fort Lee, New Jersey
Dirk U. Duddeck, DDS
Managing Director, CleanImplant Foundation, Berlin, Germany
Gregori M. Kurtzman, DDS, MAGD
Former Assistant Clinical Professor, University of Maryland School of Dentistry, Baltimore, Maryland; Diplomate, International Congress of Oral Implantologists; Private Practice, Silver Spring, Maryland
REFERENCES
1. Lo Bianco L, Montevecchi M, Ostanello M, Checchi V. Recognition and treatment of peri-implant mucositis: Do we have the right perception? A structured review. Dent Med Probl. 2021;58(4):545-554.
2. Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Periodontol. 2018;89 suppl 1:S267-S290.
3. Greenstein G, Eskow R. High prevalence rates of peri-implant mucositis and peri-implantitis post dental implantations dictate need for continuous peri-implant maintenance. Compend Contin Educ Dent. 2022;43(4):206-213.
4. Hu C, Lang NP, Ong MM, et al. Influence of periodontal maintenance and periodontitis susceptibility on implant success: a 5-year retrospective cohort on moderately rough surfaced implants. Clin Oral Implants Res. 2020;31(8):727-736.
5. Lee CT, Huang YW, Zhu L, Weltman R. Prevalences of peri-implantitis and peri-implant mucositis: systematic review and meta-analysis. J Dent. 2017;62:1-12.
6. Astolfi V, Rios-Carrasco B, Gil-Mur FJ, et al. Incidence of peri-implantitis and relationship with different conditions: a retrospective study. Int J Environ Res Public Health. 2022;19(7):4147.
7. Amerio E, Blasi G, Valles C, et al. Impact of smoking on peri-implant bleeding on probing. Clin Implant Dent Relat Res. 2022;24(2):151-165.
8. Costa FO, Lages EJP, Cortelli SC, et al. Association between cumulative smoking exposure, span since smoking cessation, and peri-implantitis: a cross-sectional study. Clin Oral Investig. 2022;26(7):4835-4846.
9. Renvert S, Polyzois I. Risk indicators for peri-implant mucositis: a systematic literature review. J Clin Periodontol. 2015;42 suppl 16:S172-S186.
10. Lee DW. Periodontitis and dental implant loss. Evid Based Dent. 2014;
15(2):59-60.
11. Duddeck DU, Albrektsson T, Wennerberg A, et al. On the cleanliness of different oral implant systems: a pilot study. J Clin Med. 2019;8(9):1280.
12. Mouhyi J, Dohan Ehrenfest DM, Albrektsson T. The peri-implantitis: implant surfaces, microstructure, and physicochemical aspects. Clin Implant Dent Relat Res. 2012;14(2):170-183.
13. Hallab NJ, Jacobs JJ. Biologic effects of implant debris. Bull NYU Hosp Jt Dis. 2009;67(2):182-188.
14. Matthews JB, Besong AA, Green TR, et al. Evaluation of the response of primary human peripheral blood mononuclear phagocytes to challenge with in vitro generated clinically relevant UHMWPE particles of known size and dose. J Biomed Mater Res. 2000;52(2):296-307.
15. Rader CP, Sterner T, Jakob F, et al. Cytokine response of human macrophage-like cells after contact with polyethylene and pure titanium particles. J Arthroplasty. 1999;14(7):840-848.
16. Shanbhag AS, Bailey HO, Hwang DS, et al. Quantitative analysis of ultrahigh molecular weight polyethylene (UHMWPE) wear debris associated with total knee replacements. J Biomed Mater Res. 2000;53(1):100-110.
17. Duddeck DU, Albrektsson T, Wennerberg A, et al. Quality assessment of five randomly chosen ceramic oral implant systems: cleanliness, surface topography, and clinical documentation. Int J Oral Maxillofac Implants. 2021;36(5):863-874.
18. Duddeck D, Albrektsson T, Wennerberg A, et al. CleanImplant Trusted Quality Mark 2017-2018 - Process Description Quality Mark Criteria. CleanImplant Foundation; 2017. https://www.cleanimplant.org. Accessed November 16, 2022.
19. Norton MR. Will any dental implant do? Br Dent J. 2020;228(4):243-244.