Guided Bone Regeneration of a Seibert Class III Bone Defect With Bioactive Calcium Phosphosilicate Bone Graft: Human Histology and Clinical Report
Filipe F. Lopes, DMD, DDS; and Maurice Salama, DDS
Abstract: This clinical case aimed to achieve two main objectives. The first was to determine if the use of only calcium phosphosilicate bone graft as a regeneration material (with no autologous bone added) on a severe vertical and horizontal mandibular defect would allow enough bone to be obtained to enable the placement of dental implants. The second objective was to determine histologic characteristics of the regenerated site after a healing period of 10 months.
Vertical ridge augmentation is one of the greatest challenges for bone regeneration in implant dentistry. Intraoperative and postoperative complications are common.1-3 Achieving bone regeneration without osseous wall containment is biologically demanding.4,5 Covering the grafted area is also a challenge as the increased dimensions necessary for vertical ridge augmentation can make it difficult to achieve tensionfree wound closure.6
Three therapeutic modalities have been proposed for vertical ridge augmentation: distraction osteogenesis,7 bone blocks (either as onlays or inlays/interpositional grafts),8,9 and guided bone regeneration (GBR).10,11
Despite numerous studies having been done on all of these methods, the most suitable approach remains unclear.12 Block grafts are often described as the "gold standard" for severe atrophies13; however, advances in the field of biomaterials have favored the use of GBR, a procedure that is significantly less invasive than the first two.12
In the case presented here, GBR for implant placement in a severe clinical situation was accomplished using only calcium phosphosilicate as a regeneration material.
Case Presentation
A 42-year-old female patient with a severe vertical and horizontal defect in the left posterior mandible, a Seibert class III defect,14 with two failing dental implants that were never loaded, presented for treatment. The patient had spent more than 2 years waiting for the implants to be restored. She reported having great difficulty in trying to properly chew food and also being psychologically affected by the absence of a large span of teeth.
The patient reported having no systemic conditions or medications. After a thorough dental examination, several treatment needs were identified. In the previous 2 years, the patient had been subjected to extensive dental treatment, including endodontic treatments, restorations, dental implants, veneers, and crown-and-bridges. All treatments were failing, with obvious implications to the treatment plan.
To enable a more comprehensive evaluation of the existing conditions and establish a treatment plan, several clinical photographs were taken (Figure 1) and a cone-beam computed tomography (CBCT) examination was done (Figure 2). The alveolar nerve was particularly superficially located, both at its emergence on the mental nerve and also on all portions of the ridge where implants needed to be placed. A sequential approach was suggested, not only because of financial reasons, but also to address and provide adequate timing for all the patient's needs, as many of them had long waiting periods. (The patient had a similar clinical situation on the right mandible, with a failing bridge on two failing implants less than 1 year in function. She also presented with a failing implant and bridge on her right maxilla and a large cyst on tooth No. 5. Together, all of these conditions resulted in severely impaired function. She also presented with esthetic complaints about six maxillary veneers from canine to canine.)
After discussing all of the treatment needs with the patient, it was decided that treatment would begin on the third quadrant. This is the part of the treatment that is the subject of this clinical case report.
Existing implants were removed and a custom titanium mesh was fabricated (according to the patient's preoperative CBCT). The mesh was loaded with calcium phosphosilicate (NovaBone® Morsels, NovaBone, novabonedental
.com), and then remaining voids were filled with putty (NovaBone Putty®, NovaBone) through the holes in the titanium mesh (Figure 3). An acellular dermal matrix was used to cover the entire titanium mesh. Tension-free primary closure of the wound was achieved.
Ten months later, a CBCT of the area was done. Biopsies of the regenerated area were conducted, taken from the implant bed preparations (Figure 4). Trephine burs were used to collect the biopsies, which comprised four cylinders of 3.5 mm diameter by 5 mm to 6 mm length. Four implants were then placed into the regenerated area (Figure 5 and Figure 6).
Rationale for Treatment Approach
There were four possible treatment options to consider for this severe clinical situation, all of which were discussed with the patient.
The first option was distraction osteogenesis. The patient rejected this option because of the procedure's complexity, and moreover, the clinician had no experience with this technique. The next option discussed with the patient was the use of short implants; however, because vertical and horizontal bone volume were inadequate, especially in the region from where the failing implants were to be extracted, this option was ruled out.
The use of bone blocks was also discussed. Although the clinician considered this to be one of the best possible treatment options, the need for a second surgical site (ie, donor site) was a major factor in the patient deciding against it as she desired a much less invasive procedure. Finally, GBR was deemed the best option for two main reasons: first, it has a lower complication rate when compared to the other viable treatment modalities, and second, it is much less invasive than the first and third options.12,15,16
Rationale for the Use of the Primary Products in the Case
The titanium mesh was loaded with calcium phosphosilicate (morsels) before being positioned and immobilized with screws against the recipient site (Figure 3). Then, all of the small voids were filled with calcium phosphosilicate (putty) dispensed via an easy-to-use unidose cartridge.
In this case, the clinician relied on the general properties of calcium phosphosilicate (morsels); namely, it is osteostimulative, osteoconductive, macroporous, fully resorbable, and radiodense.17 It was used as the sole bone grafting material; no autologous bone was added. The putty was used only to fill small voids under the titanium mesh. The putty material is not macroporous; it is non-porous.
This biomaterial is osteoconductive: bone formation occurs along the surfaces of the biomaterial's particles. Osteoconductive grafts usually are not bioactive and are just scaffolds without active chemical interaction. This is not the case, however, with calcium phosphosilicate. Besides being osteoconductive, it promotes osteostimulation, an active mechanism (bioactive regenerative)stimulating osteoblast proliferation and differentiation due to chemical ion release. The biomaterial acts as a matrix and encourages the differentiation of new bone cells at the site, resulting in faster bone regeneration than exhibited by osteoconduction alone. New bone formation occurs throughout the defect, not just at the defect margins.
In the present case, the bone volume obtained and the histological characteristics of the regenerated areas appeared adequate to receive dental implants, even though no autologous bone was used (Figure 5 and Figure 6). The resulting bone volume was a substantial improvement compared to the initial clinical situation, allowing the placement of four dental implants.
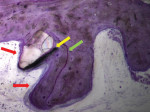
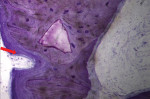
Biopsies of all of the involved areas (Figure 7 and Figure 8) showed several interesting results: a large portion of the regenerated area was bone, there were areas of intense remodeling and osteogenic activity, and there were well-osseointegrated biomaterial particles. Figure 9 demonstrates the outcome of the case at 3 months post-implant placement. (The author notes that this was a complex case in which bone and soft tissues had to be grafted. After bone grafting, implant placement was possible. At the time of this writing, the implants were not yet restored because soft tissues were not suitable to proceed with the final restoration and still have to be grafted.)
Conclusion
This case report showed that it seems reasonable to consider the use of calcium phosphosilicate alone as an adequate biomaterial to perform GBR of extraosseous defects. Histological analysis and findings are extremely clinically relevant, revealing in this case that it appears possible to accomplish the effective bone regeneration of severe 3-dimensional defects without the need to use autologous bone. This approach would equate to less morbidity for the patient, precluding the need for a second surgical site (ie, donor site). It would also enable less complex surgical procedures, making it easier for clinicians to focus only on the defect to be regenerated and allowing them to perform just one surgery.
Acknowledgment
The histologies in this case (Figure 7 and Figure 8) were provided by Laboratório de Investigação de Tecidos Duros - Coimbra Medical University, Coimbra, Portugal.
Disclosure
This article was commercially supported by NovaBone.
About the Authors
Filipe F. Lopes, DMD, DDS
Private Practice, Porto, Portugal
Maurice Salama, DDS
Private Practice, Atlanta, Georgia
References
1. Fontana F, Maschera E, Rocchietta I, Simion M. Clinical classification of complications in guided bone regeneration procedures by means of a nonresorbable membrane. Int J Periodontics Restorative Dent. 2011;31(3):265-273.
2. Rocchietta I, Fontana F, Simion M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: a systematic review. J Clin Periodontol. 2008;35(8 suppl):203-215.
3. Tinti C, Parma-Benfenati S, Polizzi G. Vertical ridge augmentation: what is the limit? Int J Periodontics Restorative Dent. 1996;
16(3):220-229.
4. Wang HL, Boyapati L. "PASS" principles for predictable bone regeneration. Implant Dent. 2006;15(1):8-17.
5. Esposito M, Grusovin MG, Worthington HV, Coulthard P. Interventions for replacing missing teeth: bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev. 2006;(1):CD003607.
6. Urban IA, Monje A, Lozada JL, Wang HL. Long-term evaluation of peri-implant bone level after reconstruction of severely atrophic edentulous maxilla via vertical and horizontal guided bone regeneration in combination with sinus augmentation: a case series with 1 to 15 years of loading. Clin Implant Dent Relat Res. 2017;19(1):46-55.
7. Froum SJ, Rosenberg ES, Elian N, et al. Distraction osteogenesis for ridge augmentation: prevention and treatment of complications. Thirty case reports. Int J Periodontics Restorative Dent. 2008;28(4):337-345.
8. Chiapasco M, Brusati R, Ronchi P. Le Fort I osteotomy with interpositional bone grafts and delayed oral implants for the rehabilitation of extremely atrophied maxillae: a 1-9-year clinical follow-up study on humans. Clin Oral Implants Res. 2007;18(1):74-85.
9. Chiapasco M, Zaniboni M, Rimondini L. Autogenous onlay bone grafts vs. alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: a 2-4-year prospective study on humans. Clin Oral Implants Res. 2007;18(4):432-440.
10. Hämmerle CHF, Jung RE. Bone augmentation by means of barrier membranes. Periodontol 2000.2003;33:36-53.
11. Buser D, Brägger U, Lang NP, Nyman S. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin Oral Implants Res. 1990;1(1):22-32.
12. Urban IA, Montero E, Monte A, Sanz-Sánchez I. Effectiveness of vertical ridge augmentation interventions: a systematic review and meta-analysis. J Clin Periodontol.2019;46(suppl 21):319-339.
13. Tessier P, Kawamoto H, Matthews D, et al. Autogenous bone grafts and bone substitutes-tools and techniques: I. A 20,000-case experience in maxillofacial and craniofacial surgery. Plast Reconstr Surg.2005;116(4 suppl):6S-24S.
14. Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part I. Technique and wound healing. Compend Contin Educ Dent. 1983;4(5):437-453.
15. Ilharreborde B, Morel E, Fitoussi F, et al. Bioactive glass as a bone substitute for spinal fusion in adolescent idiopathic scoliosis: a comparative study with iliac crest autograft. J Pediatr Orthop. 2008;28(3):347-351.
16. Wheeler DL, Eschbach EJ, Hoellrich RG, et al. Assessment of resorbable bioactive material for grafting of critical-size cancellous defects. J Orthop Res. 2000;18(1):140-148.
17. Gonshor A, Saroff SA, Anderegg CR, et al. Histologic and clinical evaluation of a bioactive calcium phosphosilicate bone graft material in postextraction alveolar sockets. Int J Oral Implantol Clin Res. 2011;2(2):79-84.