Immediate Loading of Full-Arch Prostheses Utilizing Self-Drilling Implants
Mahmoud Serag, BDS, MDS; Alex Gillone, DDS, MS; and Acela A. Martinez Luna, DMD, MS
Abstract: The use of a dental implant system that allows for primary stability and immediate loading in the treatment of terminal dentitions requiring full-mouth extractions and implants can be advantageous for both the clinician and the patient. This case report describes the treatment of a patient with a failing dentition with placement and immediate loading of self-drilling dental implants for full-arch maxillary and mandibular implant-supported prostheses.
Treatment of terminal dentitions with full-arch implant-supported prostheses has become a common treatment modality for patients seeking improved esthetics and function with a fixed approach. Furthermore, advances in biomaterials, implant design, and prosthetic components offer clinicians the opportunity to provide comprehensive implant treatment in a shorter period of time while helping to ensure long-term success and preservation of crestal bone.
When dental implants are placed, primary stability plays a crucial role in osseointegration, especially in immediate implant placement scenarios (with or without immediate loading). Adequate primary stability is fundamental to withstand implant micromovement before osseointegration is obtained. Also, primary stability is positively correlated with secondary stability with ensuing new osseous tissue formation.1,2 Primary stability may be influenced by various patient-related factors, such as socket or peri-implant osseous defect morphology, bone density, cortical thickness, and osseous height.3,4 These factors cannot be controlled by the clinician; however, implant selection could affect the initial stability depending on implant design, geometry, treatment surface, and drilling protocols.1
Immediate loading with a one-piece fixed interim prosthesis has demonstrated high implant and prosthesis survival rates and can be recommended for both the maxilla and mandible.5 Nevertheless, it is important to note that there may be a higher risk for implant failure of immediate-loaded implants in the maxilla as compared to the mandible,6,7 which may possibly be due to the difference in bone density. While this treatment modality has been widely utilized and documented, recent advances in implant design have allowed clinicians to increase the possibility of immediate loading with improved predictability. Before immediate loading edentulous arches, the primary stability of each implant must be confirmed5; therefore, the use of an implant system that could aid in obtaining primary stability is intuitively advantageous.
The purpose of this case report is to demonstrate the use and advantages of a self-drilling dental implant system for full-arch immediate implant placement and loading, and subsequent rehabilitation with implant-supported prostheses. This treatment option offers several advantages as compared to conventional loading protocols, such as increased patient satisfaction through the delivery of an immediate fixed temporary prosthesis, reduction of postoperative discomfort caused by a removable interim prosthesis, fewer appointments, and shorter overall treatment length.5
Case Presentation
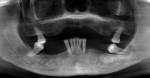
A 62-year-old African American female patient with well-controlled hypertension presented to the East Carolina University School of Dental Medicine Faculty Practice Clinic for comprehensive treatment. Her chief complaint pertained to her existing maxillary prosthesis; she was seeking to improve her esthetics and speech with a fixed approach. Clinical and radiographic examination revealed partial edentulism, generalized stage IV grade C periodontitis, and an ill-fitting acrylic maxillary partial denture retained from two molars opposing a partially edentulous mandible (Figure 1 and Figure 2).
The patient was presented with several treatment options, including implant-retained overdentures and implant-supported prostheses. Because the patient wanted to replace her teeth with a fixed approach, the selected treatment plan included maxillary and mandibular full-arch implant-supported prostheses.
Preliminary impressions were made using large plastic stock trays and alginate (Jeltrate®, Dentsply Sirona, dentsplysirona.com). Vertical dimension of occlusion, centric relation, and incisal edge position were assessed. Jaw relation records were made using occlusal rims and polyvinyl siloxane (Regisil®, Dentsply Sirona). The patient's smile was assessed to determine the future location of the prosthesis tissue junction (PTJ).8 Casts were mounted on a semi-adjustable articulator (Hanau™ Wide-Vue, Whip Mix, whipmix.com). A cone-beam computed tomography (CBCT) scan was obtained, and the case was planned virtually using coDiagnostiX® (Dental Wings, dentalwings.com) software to determine the size and location of the implants. Cast surgery was completed on maxillary and mandibular casts according to the location of the planned PTJ and to obtain adequate restorative space for the planned screw-retained prostheses.
Under local anesthesia and nitrous oxide inhalation sedation, full-thickness maxillary and mandibular flaps were elevated, and the remaining teeth were extracted. Using a slow-speed handpiece with surgical bur, alveoloplasty was completed to obtain the previously planned restorative space. Five maxillary and four mandibular Straumann® BLX implants (Straumann, straumann.com) were placed to 35 Ncm-45 Ncm, followed by placement of Straumann® screw-retained abutments (SRA) (Straumann) torqued to 35 Ncm (Figure 3 and Figure 4).
Particulate bovine xenograft (Bio-Oss®, Geistlich Biomaterials, geistlich-na.com) was placed in the socket space around implants Nos. 27 and 29 and covered with a resorbable collagen membrane (Bio-Gide®, Geistlich Biomaterials). Tissues were adapted and sutured with 4-0 polytetrafluoroethylene suture (CytoSurg®, Salvin Dental, salvin.com), and primary closure was obtained. The temporary cylinders were screwed and picked up with acrylic utilizing the prostheses. The interim prostheses were finalized in the laboratory and delivered (Figure 5).
After a healing period of 3 months following implant placement, an open-tray impression was obtained. A polymethyl methacrylate (PMMA) prototype was delivered to evaluate the esthetics and function (Figure 6). The PMMA prototype was scanned (CEREC® Omnicam, Dentsply Sirona), and a full-arch maxillary and mandibular zirconia prosthesis was delivered (Sculpture Studios, sculpturestudios.net) (Figure 7 and Figure 8). The patient was very satisfied with the treatment outcomes, including the improved esthetics and function.
Discussion
Overall, this documented case report demonstrates that extraction of failing teeth, simultaneous implant placement, and immediate loading of full-arch interim prostheses are feasible treatment options for patients with a terminal dentition. This case report also demonstrates the importance of diagnostic treatment planning for successfully treating complex cases requiring both surgical and prosthetic management.
In immediate and early implant loading protocols, implant stability and the ability to promote predictable and rapid osseointegration after placement are major considerations for treatment success. The advantages of immediate loading in terms of reduced treatment time and improved patient satisfaction are important factors; however, the clinician needs to ensure that the implants placed are both clinically and functionally successful long-term. Implant success depends not only on initial osseointegration but also on preservation of the crestal bone.9 The implant system used in this case has several features that helped in obtaining improved primary stability for potential immediate loading along with potential long-term bone preservation.
The Straumann BLX implant has a "self-drilling" design with double threads that are designed to provide initial stability via uniform and controlled osseous compaction and densification around the implant while obtaining dissipation of stress from the peri-implant bone.10 This design has a protruding thread geometry in combination with a reduced diameter implant neck, which determine its mechanism of bone engagement and force distribution in loading situations.11 This implant system is aimed at maximizing primary stability in situations with limited bone quantity, lack of cortical bone, and poor bone density/quality (eg, posterior maxilla).4,10
Emmert et al demonstrated in an in vitro study that the mean primary stability of BLX implants placed in type IV bone (regardless of the presence of cortical bone) is significantly higher as compared to other implant designs.4 This finding could be due to the double-thread design and the presence of sharp and highly engaging apical threads, which allow bone-to-implant contact and mechanical anchorage with minimal negative effect in the absence of cortical bone. The implant thread design likely contributes to primary stability by increasing the initial contact with the underlying bone12; therefore, this implant system may be beneficial for post-extraction sockets or osseous defects, as illustrated in this case report. Stabilization of the implant within the socket or osseous defect without additional apical drilling can be obtained with the use of this system featuring protruding self-drilling threads. In addition, the tapered implant design may provide additional primary stability. Compared to parallel implants, conical/tapered implants have increased implant stability quotient (ISQ) values and excellent primary stability and mechanical anchorage due to an improved compressive force distribution.1,13
The Straumann BLX system is composed of a Roxolid® (Straumann) alloy in combination with SLActive® (Straumann) surface. This titanium-zirconium (TiZr) alloy is a biocompatible biomaterial with higher tensile strength as compared to pure titanium.14,15 Due to its excellent mechanical properties, the TiZr alloy may be utilized with diameters of 3.75 mm or greater with this system.10 Additionally, the hydrophilic SLActive surface allows for faster osseointegration and shorter healing periods16 and long-term implant survival and crestal bone maintenance in immediate and early loading protocols.9
Maintenance of the crestal bone is crucial for long-term implant success, peri-implant health, and soft-tissue stability.17 Several implant-related and prosthetic factors may influence the maintenance of crestal bone. The implant system utilized in this case report has a reduced neck diameter that minimizes the stress concentrated in the cortical bone following insertion. Furthermore, the system has a single TorcFit® (Straumann) connection that allows the use of prosthetic components with reduced diameters and thus may allow for platform switching and the associated benefits, such as crestal bone preservation and maintenance of soft tissue around the implant neck.10
Besides the benefit of crestal bone maintenance, having one single connection significantly reduces the number of prosthetic and surgical instruments needed in the overall treatment armamentarium. Francisco et al in an in vivo animal model assessed the influence of transgingival healing and submerged healing on peri-implant bone maintenance on Straumann BLX implants and found that both approaches have similar bone levels with gain in crestal bone height at 12 weeks.11 Interestingly, the transgingival healing group in this study showed increased bone formation on the buccal aspect of the implant. This in vivo study further supports the use of this implant system for transgingival healing for complex cases with immediate loading.
Lastly, the use of prosthetic components with designs compatible with peri-implant soft-tissue health (eg, the novel, edge-free, rounded Straumann SRA abutments with the BLX system) that can be maintained by the patient is a crucial factor in obtaining long-term peri-implant health and crestal bone maintenance.
Conclusion
Proper case selection and utilization of self-drilling implants and appropriate prosthetic components can aid the clinician in performing full-arch immediate placement and loading of dental implants with the end goal of long-term success and maintenance of crestal bone. In addition, the patient benefits from fewer interventions and less treatment time while esthetics and function are improved as early as the implant placement appointment.
Acknowledgment
The authors thank Hanan Elgendy, BDS, for her contribution of clinical photography to this article.
Disclosure
This article was commercially supported by Straumann.
About the Authors
Mahmoud Serag, BDS, MDS
Clinical Director, Local Start Dental, Durham, North Carolina; Fellow, American College of Prosthodontics
Alex Gillone, DDS, MS
Clinical Assistant Professor and Division Director of Periodontology, East Carolina University School of Dental Medicine, Greenville, North Carolina; Diplomate, American Board of Periodontology; Fellow, International Team for Implantology
Acela A. Martinez Luna, DMD, MS
Clinical Assistant Professor and Division Director of Clinical Implantology, East Carolina University School of Dental Medicine, Greenville, North Carolina; Diplomate, American Board of Periodontology; Fellow, International Team for Implantology
References
1. Ibrahim A, Heitzer M, Bock A, et al. Relationship between implant geometry and primary stability in different bony defects and variant bone densities: an in vitro study. Materials (Basel). 2020;13(19):4349.
2. Davies JE. Mechanisms of endosseous integration. Int J Prosthodont. 1998;11(5):391-401.
3. Arosio P, Arosio F, Di Stefano DA. Implant diameter, length, and the insertion torque/depth integral: a study using polyurethane foam blocks. Dent J (Basel). 2020;8(2):56.
4. Emmert M, Gülses A, Behrens E, et al. An experimental study on the effects of the cortical thickness and bone density on initial mechanical anchorage of different Straumann® implant designs. Int J Implant Dent. 2021;7(1):83.
5. Gallucci GO, Benic GI, Eckert SE, et al. Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants. 2014;29 suppl:287-290.
6. Andersson P, Degasperi W, Verrocchi D, Sennerby L. A retrospective study on immediate placement of Neoss implants with early loading of full-arch bridges. Clin Implant Dent Relat Res. 2015;17(4):646-657.
7. Ji TJ, Kan JY, Rungcharassaeng K, et al. Immediate loading of maxillary and mandibular implant-supported fixed complete dentures: a 1- to 10-year retrospective study. J Oral Implantol. 2012;38 spec no:469-476.
8. Bidra AS, Agar JR. A classification system of patients for esthetic fixed implant-supported prostheses in the edentulous maxilla. Compend Contin Educ Dent. 2010;31(5):366-374.
9. Nicolau P, Guerra F, Reis R, et al. 10-year outcomes with immediate and early loaded implants with a chemically modified SLA surface. Quintessence Int. 2019;50(2):114-124.
10. Fromovich O, Dada K, Pariente L, Daas M. BLX: a new generation of self-drilling implants. Quintessence. Special Issue. 2019:7-38.
11. Francisco H, Finelle G, Bornert F, et al. Peri-implant bone preservation of a novel, self-cutting, and fully tapered implant in the healed crestal ridge of minipigs: submerged vs. transgingival healing. Clin Oral Investig. 2021;25(12):6821-6832.
12. Udomsawat C, Rungsiyakull P, Rungsiyakull C, Khongkhunthian P. Comparative study of stress characteristics in surrounding bone during insertion of dental implants of three different thread designs: A three-dimensional dynamic finite element study. Clin Exp Dent Res. 2018;5(1):26-37.
13. Romanos GE, Ciornei G, Jucan A, Malmstrom H, Gupta B. In vitro assessment of primary stability of Straumann® implant designs. Clin Implant Dent Relat Res. 2014;16(1):89-95.
14. Altuna P, Lucas-Taulé E, Gargallo-Albiol J, et al. Clinical evidence on titanium-zirconium dental implants: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2016;45(7):842-850.
15. Kobayashi E, Matsumoto S, Doi H, et al. Mechanical properties of the binary titanium-zirconium alloys and their potential for biomedical materials. J Biomed Mater Res. 1995;29(8):943-950.
16. Lang NP, Salvi GE, Huynh-Ba G, et al. Early osseointegration to hydrophilic and hydrophobic implant surfaces in humans. Clin Oral Implants Res. 2011;22(4):349-356.
17. Romanos GE. Tissue preservation strategies for fostering long-term soft and hard tissue stability. Int J Periodontics Restorative Dent. 2015;35(3):363-371.