Tongue Restriction Questionnaire: A New Screening Tool to Identify Tongue-Tied Patients
Richard Baxter, DMD, MS; Ashley Lashley, BS; and Nicholas R. Rendell, PhD
Abstract
Purpose:This study was intended to determine the prevalence of tongue restrictions in a pediatric population and develop a screening tool for tongue-tie symptoms. Methods:Patients were screened for tongue elevation and common symptoms using a novel Tongue Restriction Questionnaire (TRQ) that assesses symptoms throughout the lifespan. Results:In total, 314 children (47.5% male) with a mean age of 5.8 years were screened; 25.5% of children were grade 1 (could elevate the tongue >80% to the incisive papilla), 51.3% were grade 2 (50%-80%), 20.4% were grade 3 (25%-50%), and 2.9% were grade 4 (<25% elevation) or most restricted. Inter-rater reliability between the dentist and the hygienist's independent grades was highly significant (ᴋ = .915, P < .001). With regard to consideration of the child's symptoms in addition to the functional grade (tongue elevation), 26.1% of parents were interested in a referral for possible treatment; 24.5% chose to wait and consider treatment in the future if symptoms worsened; 49.4% of children had excellent mobility and/or were unaffected. Childhood symptoms that correlated with more restricted tongue grades were spitting out food (P = .004) and slow eating (P = .021), and a history of prolonged feeding (P = .052) and milk dribbling out of the mouth (P = .027) as infants. A higher symptom score in infancy correlated with a higher score in childhood (r = .386, P < .001) and a greater likelihood of referral in childhood (P < .001). Conclusions:Tongue restrictions are common in pediatric patients presenting to dental practices, and symptom presentations vary between patients. Tongue elevation is an easy and reliable test of tongue mobility. Shared decision-making and proper assessments help prevent undertreatment and overtreatment.
Dentists are well-positioned to identify and treat patients of all ages with restricted tongue mobility from tongue-tie (ankyloglossia). In fact, a patient's dentist is likely to be the first to screen for and identify a restricted tongue. Tongue-tie impacts breastfeeding and bottle feeding and is commonly treated in infancy.1-3 The condition was once thought to be highly uncommon, and medical and dental programs advised trainees that children would stretch or rupture the frena before they caused problems related to speech or feeding.4 Estimates of the prevalence of tongue-ties in the 20th century were less than 1%, with some as low as 0.02%.5 Currently, it is estimated that the prevalence of anterior or near-the-tip tongue-ties is higher than previously reported, at 4% to 10%.1,6 The restricted tissue does not stretch out, so it persists into childhood, adolescence, and adulthood and should be evaluated by the dentist during an intraoral examination.7
Restrictions of the tongue also can be less apparent, especially when the restriction arises from restrictive fascia under the tongue and is deep or posterior to the mucosal surface (submucosal) (Figure 1).8-10 Patients with these less-visible variants of tongue restrictions often see impressive improvements when the restriction is properly released.10-14 A spectrum of restriction, therefore-from a classic to-the-tip appearance that is obvious upon inspection, to a webbing beneath the mucosa that is barely perceptible without palpation-can cause limitations in function (Figure 2).9,11 Symptoms arising from these restrictions can affect patients' quality of life significantly.14 When less-apparent submucosal (posterior) tongue restrictions are included, the true prevalence of restrictions is likely approximately 20% to 25%.10,15,16 A recent study from Brazil examining newborn babies for anterior and posterior tongue-ties reported a prevalence of 32.5%.16
Unfortunately, many tongue-ties in babies are not identified early in life.17 Limitations in speech, solid feeding, and sleep may originate in childhood and persist into adulthood. These can be treated by frenectomy with resulting functional improvement in most cases.14,17-20 Because of the multi-symptom and variable presentations of tongue-tied patients, ankylogossia often is overlooked as the source of many of these issues.11,14,19 Dentists and physicians are well-positioned to screen patients for this fairly common condition. However, currently there is no validated screening tool available.
To properly diagnose and treat ankyloglossia, a distinction must be made between a normal frenum and a pathologic one with a similar appearance.15,16,21 Some patients have what appears to be a tongue restriction but have no functional issues or symptoms. Others have virtually no string or apparent restriction but have many symptoms.14 With this diagnostic challenge, in order for providers to best determine which patients, whether children or adults, should receive treatment, a screening tool is needed to determine an individual's limitations, historical issues in infancy and childhood, and degree of functional restriction. Such an instrument could improve assessment and help in the identification of patients who would benefit from further evaluation.
The purpose of this study was to design a questionnaire that is easy to use in daily practice, can aid in detecting the patient's condition, and can facilitate shared decision-making with patients. The authors believe it is important to determine how many patients in a typical dental office are affected by ankyloglossia and which symptoms are most commonly related to a restricted tongue. The relationship between symptoms and appearance might help determine which patients will benefit from further assessment, which patients can be monitored, and which patients require no further evaluation.
Methods and Materials
Patients were recruited from dental hygiene visits at a pediatric dental practice in a continuous manner and were not chosen after examination. Children with previously released tongue-ties were excluded from participation. The patients' caregivers were asked to fill out the anonymous novel screening questionnaire, the Tongue Restriction Questionnaire (TRQ), which included 28 typical infant-through-adult issues that often accompany a tongue restriction and improve after treatment (Figure 3).10,14,15,19,22 The TRQ was designed to assess common symptoms of restricted tongue mobility in any patient population, infants through adults. The sample was taken of any patient presenting for a dental hygiene visit in the authors' pediatric practice. A condensed version of the TRQ with fewer questions was also created. The revised TRQ excluded questions about past infant symptoms as well as multifactorial symptoms that might or might not be associated with a tongue restriction, such as ear infections, enlarged tonsils and adenoids, sinus issues, crooked teeth, and thumb sucking (Figure 4). The authors also tested this version using the collected data to determine which questionnaire performed better.
After a calibration session with all providers (five hygienists and two dentists) using the images from Yoon et al (2017), hygienists were trained to recognize a tongue restriction and classify it before the dentist's examination.23 Restrictions were graded according to the published scale. The functional grade measures the amount a patient's tongue can elevate to the incisive papilla when the mouth is open comfortably without pain or excessive strain; this is called the tongue range of motion ratio.23 This ratio was estimated visually without the use of a mouth range of motion (ROM) ruler to simulate real-world clinical applications in which a ROM ruler may not be readily available. To best estimate tongue elevation in young children unable to follow commands, the provider assisted the child by lifting the tongue with a gloved finger to estimate the amount of elevation of the tongue to the incisive papilla (Figure 2). After the hygienist's examination, the dentist independently inspected the child and determined whether he or she child could lift the tongue less than 25% (grade 4), 25% to 50% (grade 3), 50% to 80% (grade 2), or more than 80% (grade 1) of the way to the papilla with the mouth open comfortably.23 A subjective clinical determination was then made based on the degree of restriction, symptoms reported on the questionnaire, and a brief discussion with the patient and parent about the impact of reported symptoms on the patient's quality of life. Three options were then presented: recommend a referral for a more in-depth assessment and possible treatment ("yes"), wait and see if any further symptoms arose or quality of life worsened ("maybe"), or conclude that the symptoms and appearance did not warrant further evaluation ("no").
In clinical practice, most providers divide tongue-tie into anterior (more apparent tongue restrictions, or grades 3 and 4) and posterior (less apparent, or grades 1 and 2); therefore, the research team combined these four grades into two groups for easy comparison and to determine if a more restricted tongue impacted symptom scores. Statistical analyses included descriptive statistics, analysis of variance (ANOVA), chi-square, t-test, and Cohen's kappa (ᴋ) for inter-rater reliability.
Institutional Review Board (IRB) approval and a waiver of informed consent were obtained from Solutions IRB as part of study #2018/12/8 because the data were collected without identifiable information. Data were analyzed using IBM SPSS Statistics for Windows, version 25 (IBM Corp.).
Results
Overall, 314 children (47.5% male) with a mean age of 5.8 years (range 1 year to 14.75 years) and their caregivers participated in the study. Using the dentist's evaluation of tongue grade, 25.5% of children had a grade 1 or least restricted tongue, 51.3% grade 2, 20.4% grade 3, and 2.9% grade 4 or most restricted. Inter-rater reliability between the dentist and the hygienist's independent functional grades was highly significant (ᴋ = .915, P < .001).
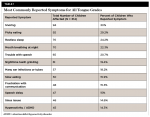
The most commonly reported symptoms for the entire sample of children were snoring (30%), picky eating (29.3%), restless sleep (24.2%), mouth breathing at night (22.3%), trouble with speech sounds (20.7%), grinding teeth at night (19.4%), ear tubes or many ear infections (18.2%), slow eating (15.9%), frustration with communication (15.3%), speech delay (15%), sinus issues (14.6%), and hyperactivity or attention deficit hyperactivity disorder (ADHD) (14.3%) (Table 1).
There was a trend toward significance with increasing symptoms correlated to more restricted grades (3 and 4) versus less restricted grades (1 and 2) (P = .083) and for the number of current symptoms related to tighter grades (3 and 4) (P = .067). The authors also analyzed the data a priori with the revised TRQ questionnaire, a variant of the TRQ that removed issues that are less related to but present in many children with tongue restrictions. In this analysis using the revised TRQ questionnaire, the tongue grade and number of symptoms (more restricted had higher symptom counts) were correlated (P = .047). Also, several individual symptoms were significantly correlated with higher and more restricted tongue grades (3 and 4). These included current feeding issues of spitting out food (P = .004) and slow eating (P = .021), and infant issues of prolonged feeding (P = .052) and milk dribbling out of the mouth (P = .027). Individual speech or sleep issues and other infant issues were not related to higher versus lower tongue grades, indicating variability in symptoms of restricted individuals.
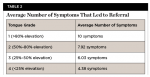
Combining the symptoms and functional grade using the TRQ revealed that 26.1% of children's parents were interested in a referral for further evaluation and possible treatment of a significant tongue restriction and many current symptoms affecting the child's quality of life ("yes" on the TRQ); 24.5% of children had symptoms or appearances that were questionable, and through shared decision-making the parents were advised to monitor their child and inform the provider if any symptoms worsened ("maybe" on the TRQ); 49.4% of children had few symptoms and/or little restriction of the tongue, and no further evaluation was warranted ("no" on the TRQ). There was a significant inverse relationship between total symptom scores and tongue grades for those who received a "yes" referral recommendation (r = -.317, P = .004). The less restrictive the tongue, the more symptoms were needed to warrant referral. The mean total symptoms to qualify for a referral for grade 4 (tightest) was 4.38 symptoms, for grade 3 was 6.03, for grade 2 was 7.92, and for grade 1 was 10 symptoms (Table 2). There was also a significant relationship between infant symptoms and later symptoms, as a higher symptom score in infancy correlated with a higher score in childhood (r = .386, P < .001). A higher symptom score in infancy also correlated with a greater likelihood of receiving a referral in childhood (P < .001). There was no difference between gender and referral for further evaluation and treatment (P = .107).
Discussion
The authors utilized a novel screening tool, the Tongue Restriction Questionnaire (TRQ), to determine the prevalence of tongue restrictions in a pediatric population. The questionnaire included eight symptoms babies commonly experience from restricted tongues and 20 symptoms that children, adolescents, and adults often experience from tongue restrictions. The questionnaire represents a condensed version of a 51-item full-symptom evaluation form that combines five domains (infant issues, speech, feeding, sleep, and other) into a synopsis of that individual's struggles and limitations (Figure 5). Many parents and providers do not realize all of the functions that might be impacted by a restricted tongue, or how symptoms can improve after a proper tongue-tie release.14 The TRQ also has a section for recording the functional grade of each patient and is intended to prompt discussion between parent and provider to decide if a referral for further evaluation and potential release of the tongue restriction is warranted.
The dentists' and hygienists' functional grades were in agreement 95% of the time, indicating it is possible to assess tongue elevation in children easily and precisely as a screen for tongue function. The functional grades were assessed separately, first by the hygienist and second by the dentist without knowing the hygienist's score. Without using a ROM ruler, the grade was assessed visually, and if the patient could lift around 25% (the line of demarcation separating a grade 3 versus 4) or 50% (the line between a grade 2 and 3) the clinician's judgment would be needed to determine the score. In all instances, the grade difference between providers was never off by more than one grade (ie, a 1 versus 2, or a 3 versus 4) and would not affect treatment recommendations, since recommending a referral is based on a discussion of the combination of the grade, symptoms present, and symptom severity. Yet, with calibration, this functional grading scale based on tongue elevation is easily taught to other providers and has high inter-rater reliability (ᴋ = .915, P < .001).
To check tongue function, simply asking a patient to lift the tongue instead of protrude the tongue (ie, "stick out your tongue and say ‘ahh'") could revolutionize the way providers assess for tongue restrictions. It is difficult to determine the degree of tongue restriction in any patient based on how far the patient can stick out his or her tongue. Evaluating protrusion alone will lead to significant underdiagnosis and not resolve the problem. Tongue elevation, not protrusion, is the essential movement for proper nursing, feeding, speech, and breathing.11,15,19,20,24,25
With improved evaluation, more children and adults with tongue restrictions can be properly identified and helped.14 Tongue-ties are thought to affect no more than 10% of the population.1,5,6 In this study, 2.9% of the children had very significantly impaired tongue movement with less than 25% elevation, and another 20.4% lifted the tongue less than 50%, which is also significantly limited. Combining grades 3 and 4, 23.3% of patients in this study were considerably restricted, which is much higher than 10%. The exact percentage is likely even higher in other offices because tongue-tied patients who were previously treated were excluded from this sample. However, not all patients with grades 3 and 4 tongue restrictions warrant releases or referrals. There must be functional limitations of speech, feeding, sleep, or other behaviors that affect quality of life before a tongue-tie release is warranted.9,21 Symptoms are the deciding factor in whether to release or not.
Total TRQ symptom count varies when comparing functional grades, with a trend toward significance with tighter restrictions yielding more issues. This finding indicates that the diagnosis is more challenging than other straightforward conditions. Children can have concerns such as tonsillar enlargement, recurrent ear infections, sinus issues, crooked teeth, or thumb sucking that may or may not be related to a tongue restriction. When the TRQ was revised and these issues were removed (Figure 4), its usage enabled the significant relationship between symptom count and tongue restriction to be detected (P = .047). A few of the feeding issues were directly related to a tighter restriction, indicating that many children experiencing feeding struggles are not just being picky. A child with a restricted tongue is more likely to spit out food (P = .004) or eat slowly (P = .021), because the physical limitation prevents proper oral function. Babies with symptoms that are left untreated are more likely to have higher symptom counts as children (P < .001) and more likely to be referred as children for further assessment and treatment (P < .001). Babies should be appropriately screened for common symptoms of tongue-ties and treated if they are present.1,2 After a full release of the restricted tissue in infancy, there seems to be a protective effect against future symptoms. To attain this effect requires a frenectomy, not a simple "clip" or "snip" frenotomy.26 Treatment is not recommended solely for potential future benefits in the absence of symptoms.15,21
Combining symptom count and tongue elevation gives the provider and the parent increased information from which to make an informed decision about the need for treatment. A grade 4 patient only needed to have a few symptoms (4.38 on average) to warrant a referral. However, a child with average elevation (grade 2) but a mean of 7.98 symptoms might also be referred for further evaluation. Even a child with seemingly above-average mobility (grade 1) but who has 10 symptoms and significant quality-of-life issues might benefit from a release. The more problems and domains involved, the higher the likelihood that a restricted tongue is playing a role in a child's limitations. Some children and adults augment tongue elevation by engaging the neck muscles and elevating the floor of the mouth, masking the true elevation of the tongue. The examiner can control the floor-of-mouth elevation by holding a gloved finger behind the mandibular incisors and asking the patient to lift; this isolates the lingual frenum and allows a more accurate visualization of restriction (this maneuver was not used in this study).19
The questionnaire did not ask how significantly these issues affected the child, but this fact was considered before a referral was recommended. The revised TRQ (Figure 4) included a section to assess how significantly the issues affected a child's quality of life. Some parents checked as many as nine issues but reported they did not affect the child significantly, while some parents checked only three or four but reported that the family struggled and attended therapy twice a week for these issues. The addition of this quality-of-life factor may help encourage discussions between parents and providers and prevent overtreatment for issues that do not impact the family significantly. It is also possible that families may be affected more than they realize and that reviewing the scores may help them recognize issues to which they had adapted unconsciously. The same effect may be seen in teens and adults in clinical practice who complete the TRQ and did not realize these related issues and a tongue restriction could be impacting their own quality of life.
The decision to refer a patient for assessment and likely treatment was based on clinical experience and the provider-parent discussion. The relatively high percentage of patients whose parents thought that a referral would be helpful (26.1%) demonstrates that the incidence of children with poor tongue function, as well as significant quality-of-life symptoms (more than 10 in many cases), is common. These symptoms and a proper evaluation of tongue function should be assessed routinely at well-child or hygiene visits by medical professionals and dentists, as the true number of children who are affected was shown to be much higher than currently thought. Teens and adults can be assessed with the same TRQ and tongue elevation measures to screen for tongue restrictions as well.
Most dentists may refer or perform a frenectomy procedure on one or two patients a year, which would be around 0.05% for a practice of 4,000 active patients. Most parents of children with clearly visible, grade 4 tongue restrictions (<25% mobility) remarked that no medical or dental provider had ever mentioned any restriction or asked about related symptoms. This finding has been reported in other studies.11,17
Providers must educate themselves and discuss this important oral examination finding with patients and their families. It is essential that dentists evaluate a patient's tongue mobility and screen for common symptoms of a tongue restriction, as there are critical yet often overlooked oral-systemic health connections that can impact a patient's quality of life throughout the lifespan.
Limitations of This Study
This sample was taken from one pediatric dental office with the main provider experienced in treating tongue restrictions. Percentages of tongue-tied patients may vary between offices, and might be higher in this one office due to referrals, or perhaps lower in the same office since it had already identified, treated, and excluded previously tongue-tied patients from this sample. This is a cross-sectional observational study, so causation cannot be assumed and generalizability is limited. While based on symptoms and appearance, diagnosis is subjective and variability among practitioners could yield different results. More research is needed to help practitioners assess and diagnose patients with tongue restrictions.
Conclusions
Tongue restrictions are more common than previously thought in patients presenting to pediatric dental practices, and systematic screening for the condition should be performed during intraoral examinations. Symptom presentations and tongue elevation vary between patients, so shared decision-making and proper assessments will help prevent undertreatment and overtreatment. Tongue elevation grading is an easy and reliable test of tongue mobility after calibration of providers and should replace protrusion as the standard test of tongue function. More research, including research in other settings, is needed to validate a screening and assessment tool for tongue restrictions so children and adults with this condition do not go undiagnosed.
About the Authors
Richard Baxter, DMD, MS
Founder and Owner, Alabama Tongue-Tie Center, Pelham, Alabama
Ashley Lashley, BS
Clinic Coordinator, Alabama Tongue-Tie Center, Pelham, Alabama
Nicholas R. Rendell, MSc, PhD
Affiliate Researcher, Birkbeck College, University of London, London, United Kingdom
References
1. Hogan M, Westcott C, Griffiths M. Randomized, controlled trial of division of tongue-tie in infants with feeding problems. J Paediatr Child Health. 2005;41(5-6):246-250.
2. Buryk M, Bloom D, Shope T. Efficacy of neonatal release of ankyloglossia: a randomized trial. Pediatrics. 2011;128(2):280-288.
3. Berry J, Griffiths M, Westcott C. A double-blind, randomized, controlled trial of tongue-tie division and its immediate effect on breastfeeding. Breastfeed Med. 2012;7(3):189-193.
4. Wallace AF. Tongue tie. Lancet. 1963;2(7304):377-378.
5. Williams WN, Waldron CM. Assessment of lingual function when ankyloglossia (tongue-tie) is suspected. J Am Dent Assoc. 1985;110(3):353-356.
6. Ricke LA, Baker NJ, Madlon-Kay DJ, DeFor TA. Newborn tongue-tie: prevalence and effect on breast-feeding. J Am Board Fam Pract. 2005;18(1):1-7.
7. de Castro Martinelli RL, Marchesan IQ, Gusmão RJ, et al. Histological characteristics of altered human lingual frenulum. Int J Pediatrics and Child Health. 2014;2(1):5-9.
8. Corrylos E, Genna C W, Salloum AC. Congenital tongue-tie and its impact on breastfeeding. American Academy of Pediatrics Section on Breastfeeding. 2004;Summer:1-6.
9. Mills N, Keough N, Geddes DT, et al. Defining the anatomy of the neonatal lingual frenulum. Clin Anat. 2019;32(6):824-835.
10. Ghaheri BA, Cole M, Fausel SC, et al. Breastfeeding improvement following tongue-tie and lip-tie release: a prospective cohort study. Laryngoscope. 2017;127(5):1217-1223.
11. Baxter R, Hughes L. Speech and feeding improvements in children after posterior tongue-tie release: a case series. Int J Clinical Pediatrics. 2018;7(3):29-35.
12. O'Callahan C, Macary S, Clemente S. The effects of office-based frenotomy for anterior and posterior ankyloglossia on breastfeeding. Int J Pediatr Otorhinolaryngol. 2013;77(5):827-832.
13. Pransky SM, Lago D, Hong P. Breastfeeding difficulties and oral cavity anomalies: the influence of posterior ankyloglossia and upper-lip ties. Int J Pediatr Otorhinolaryngol. 2015;79(10):1714-1717.
14. Baxter R, Merkel-Walsh R, Baxter BS, et al. Functional improvements of speech, feeding, and sleep after lingual frenectomy tongue-tie release: a prospective cohort study. Clin Pediatr (Phila). 2020;59(9-10):885-892.
15. Baxter R, Agarwal R, Musso M, et al. Tongue-Tied: How a Tiny String Under the Tongue Impacts Nursing, Speech, Feeding, and More. Pelham, AL: Alabama Tongue-Tie Center; 2018.
16. de Castro Martinelli RL, Marchesan IQ, Berretin-Felix G. Posterior lingual frenulum in infants: occurrence and maneuver for visual inspection. Revista CEFAC. 2018;20(4):478-483.
17. Guilleminault C, Huseni S, Lo L. A frequent phenotype for paediatric sleep apnoea: short lingual frenulum. ERJ Open Res. 2016;2(3):00043-2016.
18. Huang YS, Quo S, Berkowski JA, Guilleminault C. Short lingual frenulum and obstructive sleep apnea in children. Int J Pediatr Res. 2015;1(003). https://orofacialintegrity.com/wp-content/uploads/2015/05/short-ling-frenum-and-sleep-apnea.pdf. Accessed February 11, 2021.
19. Zaghi S, Valcu-Pinkerton S, Jabara M, et al. Lingual frenuloplasty with myofunctional therapy: exploring safety and efficacy in 348 cases. Laryngoscope Investig Otolaryngol. 2019;4(5):489-496.
20. Brooks L, Landry A, Deshpande A, et al. Posterior tongue tie, base of tongue movement, and pharyngeal dysphagia: What is the connection? Dysphagia. 2020;35(1):129-132.
21. Merkel-Walsh R, Overland L. Tongue-Tied: Functional Assessment and Remediation of TOTs (Tethered Oral Tissues). TalkTools; 2018.
22. Kotlow LA. Oral diagnosis of abnormal frenum attachments in neonates and infants: evaluation and treatment of the maxillary and lingual frenum using the Erbium: YAG laser. J Pediatric Dent Care. 2004;10(3):11-14.
23. Yoon A, Zaghi S, Weitzman R, et al. Toward a functional definition of ankyloglossia: validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017;21(3):767-775.
24. Messner AH, Lalakea ML. The effect of ankyloglossia on speech in children. Otolaryngol Head Neck Surg. 2002;127(6):539-545.
25. Geddes DT, Langton DB, Gollow I, et al. Frenulotomy for breastfeeding infants with ankyloglossia: effect on milk removal and sucking mechanism as imaged by ultrasound. Pediatrics. 2008;122(1):e188-e194.
26. Walls A, Pierce M, Wang H, et al. Parental perception of speech and tongue mobility in three-year olds after neonatal frenotomy. Int J Pediatr Otorhinolaryngol. 2014;78(1):128-131.