Zygomatic Implant Redesigned: Rationale and Biomechanical Principles
Edmond Bedrossian, DDS; and E. Armand Bedrossian, DDS, MSD
Abstract: The treatment of the moderate to advanced resorbed edentulous maxilla with a fixed prosthesis is complicated due to the presence of pneumatized maxillary sinuses posteriorly and the nasal aperture in the premaxilla. To treat patients with this condition using endosseous implants to support a functional prosthesis, grafting procedures have been advocated. The multiple surgical steps involved in the reconstruction of the resorbed maxilla, however, can be a significant barrier to patient acceptance of grafting treatment protocols. The success of graftless concepts using tilted and zygomatic implants has led to a higher case acceptance as the treatment can be accomplished in one appointment. Over the past two decades, the experience clinicians have gained using zygomatic implants has resulted in a redesign of the implant aimed at addressing the challenges associated with the treatment of patients with moderate to advanced resorbed maxillae to better serve these patients.
With a prolonged period of edentulism, the ability of patients to function with a full-arch removable prosthesis diminishes over time due to the loss of its retention as the maxillary alveolus resorbs. Tallgren and Cawood et al have described the changes to the maxillofacial alveolar bone resulting from edentulism.1,2 The contemporary literature has described the use of tilted implants to avoid extensive bone grafting procedures for patients who have residual alveolar bone in the premaxilla and the bicuspid region.3-5 In cases of advanced maxillary resorption, the zygomatic implant has been used as an alternative to extensive posterior maxillary grafting procedures. Multiple authors have reported the success rate for zygomatic implants to range from 94% to 100%.6-9 Also, Brånemark et al, Bedrossian, and Aparicio et al have reported cumulative survival rates of 94%, 97.2%, and 97.7%, respectively.10-12
When treatment planning patients with advanced maxillary resorption, communication among the implant team members is essential, and it is wise to adopt a systematic preoperative treatment planning protocol.13 The radiographic evaluation process is part of the comprehensive treatment planning protocol and is a critical step for the surgical team to screen and treatment plan for the use of a zygomatic implant. The zones of the maxilla and the zygomatic anatomy guided approach (ZAGA) as described by Bedrossian et al and Aparicio, respectively,13,14 may be used to guide surgeons in determining the potential use of zygomatic implants for this group of patients.
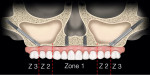
Zones of the Maxilla
On a panoramic radiograph, the maxillary alveolus is divided into three zones13: zone 1 - premaxilla (cuspid to cuspid); zone 2 - premolar area; zone 3 - molar area.
With moderate to advanced resorption patterns of the edentulous maxillary alveolus as well as the anterior positioning of large pneumatized maxillary sinuses, the placement of tilted implants in zone 2 is impossible. Therefore, for patients in whom there is the presence of bone in zone 1 only and the absence or limited volume of bone in zones 2 and 3, placement of a zygomatic implant for posterior support in conjunction with two to four premaxillary implants may be considered (Figure 1).
In cases of advanced maxillary hypoplasia/resorption, or in cases of tumor resection leading to partial or total maxillectomy, the absence of all three zones of the maxilla lends for the clinician's considering of the quad-zygoma implant concept (Figure 2).15
Zygomatic Anatomy Guided Approach (ZAGA)
In 2011, using the frontal view of a 3-dimentional radiographic study, Aparicio described the trajectory of the zygomatic implant as it relates to the patient's anatomy.14 The three areas that should be focused on during this evaluation process are the degree of concavity of the lateral wall of the maxillary sinus, the degree of maxillary alveolar resorption in the palatal direction, and the available zygoma bony volume (Figure 3).
In ZAGA 0-3 cases, the zygomatic implant is bicortically stabilized at the maxillary alveolus and zygoma bone; hence, a quad-cortically stabilized implant. In ZAGA 4 cases, the zygomatic implant is only bicortically stabilized at the zygoma bone.
Zygomatic Implant Redesign
The experience clinicians have gained using the zygomatic implant over the past two decades has led to greater understanding of the biomechanical principles that influence initial stability of the implant as well as long-term support of the final fixed prosthesis. Bedrossian et al in 2018 described how to prevent and manage potential complications that may occur with zygomatic implants.16 To address some of the issues learned from clinical outcomes over time, the cumulative experiences of the present authors and Drs. Carlos Aparicio and Sepehr Zarrine have led to a redesign of the zygomatic implant. Aimed at achieving more favorable outcomes, two different Straumann® Zygomatic implant designs have been created: the ZAGA Round implant and the ZAGA Flat implant.
Changes to the original design are focused on the following characteristics: implant diameter, surface enhancement, thread design, modifications to the middle portion of the implant, apical geometry, and angulation of the implant platform.
Implant Diameter
For patients who are missing their entire maxillary alveolar bone, placement of two zygomatic implants within the same zygoma bone is necessary (Figure 4). To address the possibility of placing two zygomatic implants within the same zygoma bone or to be able to replace a failed zygomatic implant immediately with a new zygomatic implant (the "rescue concept"17), a reduced-diameter zygomatic implant is preferred.
In the redesigned Straumann Zygomatic implant portfolio, the apical threads begin at 2.6 mm (D2) with gradual tapering toward the implant platform and terminating at 3.9 mm (D4) before the smooth midportion of the implant. The crestal threads are slightly larger than the midportion of the implant, at 4.3 mm (D1), allowing compression of the crestal bone for increased bone-to-implant contact (BIC) where possible. The implant platform is 4.3 mm in diameter with an external hex connection (Figure 5).
The reduced diameter at the apical portion of the Straumann Zygomatic Round and Flat implants will occupy a smaller volume of cancellous bone in the body of the zygoma bone. The reduction of "cutting" at the osteotomy limits the degree of apoptosis of the osteocytes lining the internal osteotomy walls18 thereby decreasing the remodeling effect within the osteotomy during the osseointegration period of the implants.
Surface Enhancement
Both machined and enhanced (rough) surfaces of endosseous implants have shown different benefits in specific applications. To achieve increased BIC, clinicians have for many years focused on surface enhancement of dental implants.19 The Straumann Zygomatic implants combine both machined and rough surface architecture to take advantage of each type of surface (Figure 5).
The sandblasted rough surface at the apical portion of the implant promotes BIC and contact osteogenesis and further stabilizes the implant during the osseointegration phase. The machined surface at the implant platform has shown a favorable soft-tissue response with Straumann® Tissue Level implants. In the redesign of the Straumann Zygomatic implants, the same machined surface has been used for the implant platform and the midportion of the implant. Stability of peri-implant soft tissue at the implant platform is essential. Oral-antral communications can be avoided by the close adaptation of the peri-abutment soft tissues to the implant platform and the abutment body.
Thread Design
The tapered design at the apical portion of the Straumann Zygomatic implant allows for the progressive compression of the zygoma bone and, therefore, increased initial stability at the time of placement. To enhance the stability of the zygomatic implant at the maxillary crest, threads and microthreads are also available at the implant platform (Figure 6).
Freedman et al in their 2013 and 2015 finite element analyses emphasized that the primary support of the zygomatic implant under function is at the implant platform, and the maintenance of bone circumferentially at the zygomatic implant platform is preferred.20,21
Modifications to the Middle Portion of the Implant
Because the midportion of the implant is either medial or lateral to the lateral wall of the maxillary sinus, and BIC is not anticipated, the middle portion of the implant is devoid of threads with a machined surface.
Apical Geometry
The design of the tip of the Straumann Zygomatic implant is round and smooth to help minimize the risk of soft-tissue irritation in cases where the implant may be slightly overextended or the patient's overlying tissue volume is thin (Figure 7).
55-Degree Platform, Screw-Retained Abutment, Prosthetic Versatility
The edentulous maxilla resorbs superiorly, palatally, and posteriorly. Because of the resorption pattern of the edentulous maxilla, the zygomatic implant platform is generally palatal to the dental arch. The one-piece 55-degree angulated platform of the Straumann Zygomatic implant allows the screw-access holes of the prosthesis to be closer to the prosthetic arch form (Figure 8).
Two Implant Designs and a Specific Abutment
The Straumann Zygomatic ZAGA Round implant is used in ZAGA 0-3 cases (Figure 6). The exiting threads and microthreads at the implant platform stabilize the implant within the residual crestal bone.
In cases of significant concavity of the lateral wall of the maxillary sinus wall, ie, ZAGA 4, or in cases of total or partial maxillectomy, the zygomatic implant will be located outside of the maxillary sinus, immediately below the soft tissue of the vestibule. There is potential for irritation of the overlying soft tissues because of muscle pull and the mobility of the vestibular soft tissues. To avoid excessive irritation of these tissues the midportion of the implant is flat, hence the Straumann Zygomatic ZAGA Flat implant (Figure 9, bottom implant). The partial palatal threads allow for potential BIC, because the implant platform will be overlying the lateral aspect of the maxilla.
A specific zygomatic screw-retained abutment, zSRA, has been developed with the abutment height ranging from 1.5 mm to 4.5 mm. The abutment engages the external hex of the Straumann Zygomatic implant and is torqued at 35 Ncm. The zSRA accepts the same titanium cylinders that are used with the existing Straumann® Bone Level implant portfolio and can be used for the fabrication of an immediate-load provisional prosthesis if immediate loading is planned (Figure 9).
Conclusion
The two redesigned Straumann Zygomatic implants should aid in the treatment of patients with moderate to severe maxillary resorption with predictable results. The use of these implants has shown encouraging and favorable outcomes to date (Figure 10 and Figure 11). Further studies are in progress to evaluate the features of the implants.
Disclosure
This article was commercially supported by Straumann.
About the Authors
Edmond Bedrossian, DDS
Diplomate, American Board of Oral & Maxillofacial Surgery
E. Armand Bedrossian, DDS, MSD
Diplomate, American Board of Prosthodontists
References
1. Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. 1972. J Prosthet Dent. 2003;89(5):427-435.
2. Cawood JI, Howell RA. Reconstructive preprosthetic surgery. I. Anatomical considerations. Int J Oral Maxillofac Surg. 1991;20(2):75-82.
3. Fortin Y, Sullivan RM, Rangert BR: The Marius implant bridge: surgical and prosthetic rehabilitation for the completely edentulous upper jaw with moderate to severe resorption: a 5-year retrospective clinical study. Clin Implant Dent Relat Res. 2002;4(2):69-77.
4. Krekmanov L, Kahn M, Rangert B, Lindstrom H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000;15(3):405-414.
5. Aparicio C, Perales P, Rangert B. Tilted implants as an alternative to maxillary sinus grafting: a clinical, radiologic, and periotest study. Clin Implant Dent Relat Res. 2001;3(1):39-49.
6. Stevenson AR, Austin BW. Zygomatic fixtures—the Sydney experience. Ann R Australas Coll Dent Surg. 2000;15:337-339.
7. Higuchi KW. The zygomaticus fixture: an alternative approach for implant anchorage in the posterior maxilla. Ann R Australas Coll Dent Surg. 2000;15:28-33.
8. Bedrossian E, Stumpel L, Beckely ML, Indresano T. The zygomatic implant: preliminary data on treatment of severely resorbed maxillae. A clinical report. Int J Oral Maxillofac Implants. 2002;17(6):861-865.
9. Malevez C, Abarca M, Durdu F, Daelemans P. Clinical outcome of 103 consecutive zygomatic implants: a 6-48 month follow-up study. Clin Oral Implant Res. 2004;15(1):18-22.
10. Brånemark PI, Gröndahl K, Ohrnell LO, et al. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):70-85.
11. Bedrossian E. Rehabilitation of the edentulous maxilla with the zygoma concept: a 7-year prospective study. Int J Oral Maxillofac Implants. 2010;25(6):1213-1221.
12. Aparicio C, Manresa C, Francisco K, et al. The long-term use of zygomatic implants: a 10-year clinical and radiographic report. Clin Implant Dent Relat Res. 2014;16(3):447-459.
13. Bedrossian E, Sullivan RM, Fortin Y, et al. Fixed-prosthetic implant restoration of the edentulous maxilla: a systematic pretreatment evaluation method. J Oral Maxillofac Surg. 2008;66(1):112-122.
14. Aparicio C. A proposed classification for zygomatic implant patient based on the zygoma anatomy guided approach (ZAGA): a cross-sectional survey. Eur J OralImplantol. 2011;4(3):269-275.
15. Davo R, Pons O, Rojas J, Carpio E. Immediate function of four zygomatic implants: a 1-year report of a prospective study. Eur J Oral Implantol. 2010;3(4):323-334.
16. Bedrossian E, Bedrossian EA. Prevention and the management of complications using the zygoma implant: a review and clinical experiences. Int J Oral Maxillofac Implants. 2018;33(5):e135-e145.
17. Bedrossian E. Rescue implant concept: the expanded use of the zygoma implant in the graftless solutions. Oral Maxillofac Surg Clin North Am. 2011;23(2):257-276.
18. Wang L, Aghvami M, Brunski J, Helms J. Biophysical regulation of osteotomy healing: an animal study. Clin Implant Dent Relat Res. 2017;19(4):590-599.
19. Schwarz F, Messias A, Sanz-Sánchez I, et al. Influence of implant neck and abutment characteristics on peri-implant tissue health and stability. Oral reconstruction foundation consensus report. Clin Oral Implants Res. 2019;30(6):588-593.
20. Freedman M, Ring M, Stassen LFA. Effect of alveolar bone support on zygomatic implants: a finite element analysis study. Int J Oral Maxillofac Surg. 2013;42(5):671-676.
21. Freedman M, Ring M, Stassen LFA. Effect of alveolar bone support on zygomatic implants in an extra-sinus position—a finite element analysis study. Int J Oral Maxillofac Surg. 2015;44(6):785-790.