When Single-Tooth Dentistry Fails: A Comprehensive Approach to Manage Risk and Restore Function
Bryan Nakagawa, DMD
Abstract: This case of a patient with a significant history of caries, single-tooth restorations, and multiple extractions demonstrates the potential problems that may be associated with intermittent, single-tooth care and the importance of restorative clinicians thoroughly assessing the patient's medical and dental history. Patients may present with a failing biological system that could lead to unforeseen circumstances during treatment. When such a case presents itself, systematic and comprehensive risk assessment can play an instrumental role in enabling the clinician to adapt to any unexpected changes to the treatment plan and achieve the best possible outcome. Completed over the course of three phases, the treatment provided in this case was aimed primarily at managing structural and caries biomechanical risk and restoring acceptable function for the patient.
Patients often present to the restorative clinician with a history of episodic, single-tooth dental care. While this may be adequate for a healthy patient with a stable and disease-resistant oral system, for patients with significant health issues and who are taking medications with oral manifestations, the dentition may be subject to failure. To predictably abate or reverse this failure, clinicians need a clear vision of the final outcome that will incorporate patient concerns and desires while taking into consideration the medical and dental landscape encompassing the patient. Even with a lucid vision and careful planning, unforeseen circumstances may alter the initial plan and necessitate treatment adaptations. Systematic and thorough risk assessment will allow the restorative clinician to adapt to changes while providing the optimal treatment outcome.
Clinical Case Overview
A 72-year-old man was referred by a local oral and maxillofacial surgeon (OMS) for a single implant restoration in the area of tooth No. 29. The patient had a long history of caries, single-tooth restorations, and multiple extractions despite being on a regular recare schedule. Implants had been placed in his mandibular arch by two different surgeons when teeth were lost. His medical history commanded significant consideration regarding the diagnosis, treatment planning, and execution of his dental care and future needs.
Medical and Dental History
The patient reported an extensive medical history, which would present challenges for dental treatment and long-term oral health success. On the medical history form (Kois Center, koiscenter.com) the following conditions were indicated: Guillain-Barré syndrome (GBS), limited scleroderma, rheumatoid arthritis, gastroesophageal reflux disease (GERD), Crohn's disease, pulmonary sarcoidosis, and a history of basal cell carcinoma. Oral manifestations of GBS may include lingering difficulty with chewing, swallowing, or speech,1 while scleroderma effects can comprise xerostomia, difficulty opening the mouth, swallowing, and speaking, and pseudoankylosis of the temporomandibular joint (TMJ).2 Rheumatoid arthritis has been associated with greater incidence of periodontal disease, decreased salivary rates, and poorer oral hygiene.3 GERD is associated with decreased oral pH, erosion of tooth structure, and increased caries risk.4 Crohn's disease complications can include aphthous ulcers, lip swelling, xerostomia, mucogingivitis, cheilitis, and salivary duct abscess or inflammation.5 Finally, sarcoidosis rarely may cause swelling of mucosa, gingivitis, and ulcers.6
Many of the patient's prescribed medications were associated with xerostomia and gastric issues. These included azathioprine, an immunosuppressive drug used for rheumatoid arthritis that can cause nausea and vomiting; diphenoxylate-atropine, which is used for irritable bowel syndrome and can cause nausea, vomiting, and dry mouth; and mesalamine DR, used for ulcerative colitis and which also may cause vomiting.
When completing the dental history form (Kois Center), the patient indicated recent caries, dry mouth, past difficulty with dental treatment, and changes to his teeth due to chipping or wear. He also mentioned that he had some difficulty speaking and limited mouth opening when receiving dental treatment, which was primarily attributed to scleroderma.2
Diagnosis, Risk Assessment, and Prognosis
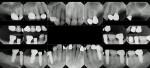
Periodontal: Periodontal examination revealed no areas of bleeding on probing. There was minor (less than 2 mm) horizontal bone loss on teeth Nos. 4, 5, 19, and 22 through 24. Less than 1 mm of recession was documented on teeth Nos. 11 and 19. All probing depths were less than 3 mm except for teeth Nos. 19 (buccal 4 mm) and 22 through 24 (mesial-distal 4 mm). The diagnosis was stage 1, grade A periodontitis, with localized areas of stage 2 (teeth Nos. 19 and 22 through 24) (Figure 1).
Risk: Low
Prognosis: Good
Biomechanical:The number and extent of caries lesions, the patient's medical conditions, and the medications he was taking were important considerations in determining the parameters of restorability of his remaining teeth.7 Tooth No. 3 was deemed hopeless because there was a failing crown and composite patch in the furcation as well as a periapical lesion. Tooth No. 4 was significantly compromised structurally and was given a guarded prognosis with the need for endodontic treatment likely. Tooth No. 12 had extensive undermining caries and a hopeless prognosis.
The mandibular dentition presented several teeth that might have been restored in a low caries risk environment. For example, teeth Nos. 19, 21, 22, 25, and 26 could have been treated with full-coverage crowns and endodontic therapy, while teeth Nos. 27 and 28 could have been addressed with full-coverage restorations. Teeth Nos. 23 and 24, however, were hopeless due to recurrent caries. Considering the patient's substantial autoimmune issues, dry mouth condition, and medications, it was determined that the likelihood of future recurrent decay was high even if current caries were removed and a strong caries management program was implemented.4 The patient elected to have the remaining teeth on the mandibular arch removed and an additional implant placed in the area of tooth No. 27, and to utilize the existing implants (Figure 1) for a screw-retained fixed prosthesis.
Risk: High
Prognosis: Poor
Functional:The patient had limited range of motion, which was most likely due to the limited scleroderma.2 He had no pain, joint sounds, or difficulty chewing, and the joints accepted load without discomfort. While the patient reported no functional issues, some fremitus was noted on maxillary anterior teeth. Wear was found on facial surfaces of the mandibular incisors, and a diastema had manifested between teeth Nos. 8 and 9 over time; the patient did not know the duration of time over which the diastema occurred.
With a diagnosis of a constricted chewing pattern, the clinician surmised that the anterior teeth might have become constricted over the course of the patient's history of tooth loss and replacement. Because the mandibular dentition was to be completely replaced, the occlusal vertical dimension (OVD) could be opened to remove the chewing pattern constriction (Figure 2 through Figure 4).
Risk: Moderate
Prognosis: Good
Dentofacial:The patient had a low lip line and did not reveal any gingival display during full smile (Figure 5).
Risk: Low
Prognosis: Good
Treatment Plan
The primary goals for treatment were to manage the structural and caries biomechanical risk and restore acceptable function to the patient. Hopeless teeth would be extracted and the existing implants on the mandibular arch would be used for an implant-supported fixed restoration. Implants would be placed at sites Nos. 3, 4, 12, and 14 to restore function to the maxillary dentition and at site No. 27 to provide additional support for the mandibular fixed restoration. The patient would be placed on a caries management protocol that would include recare visits every 4 months with fluoride varnish application, treatment rinse (CariFree CTx4™ Treatment Rinse, Oral Biotech, carifree.com), and tooth gel (CariFree CTx4™ Gel 5000, Oral Biotech).8,9
Treatment Phases
Phase 1
Teeth Nos. 3, 4, 12, 19, and 21 through 28 were removed. Crowns on implant Nos. 18, 20, and 30 were removed and healing abutments were placed to help support a mandibular immediate complete denture (ICD), which had been fabricated to use during healing of the extraction sites (Figure 6). A Locator-type abutment was placed on implant No. 29 for added retention to the mandibular ICD (Figure 7). In the maxilla, an immediate removable partial denture (IRPD) was used during the maxillary healing phase. Soft relines were implemented to aid in patient comfort. Tooth No. 6 required endodontic treatment during this phase due to a periapical lesion and pulpal necrosis.
Phase 2
Because of structural compromises and recurrent decay, lithium-disilicate crowns (e.max®, Ivoclar Vivadent, ivoclarvivadent.com) were placed on teeth Nos. 5, 6, 11, and 13. Margins on these crowns were intentionally placed 0.5 mm to 1 mm subgingivally on the premise of reducing caries susceptibility on these teeth, although the value of subgingival margins has been questioned in the literature.10
During this phase of treatment, while the mandibular ICD was in function and because it had increased the patient's OVD, the constricted chewing pattern was relieved. Additionally, the clinician noted that the diastema between teeth Nos. 8 and 9 had gradually closed.
Phase 3
Four months after his teeth had been removed, the patient was seen by an otolaryngologist for bleeding while coughing. He was referred to Oregon Health & Science University Hospital and subsequently diagnosed with oral-pharyngeal cancer-stage 2 squamous cell carcinoma p16 positive, of the left posterior base of the tongue.11 The referring OMS advised against the use of implants that had been planned for sites Nos. 3, 4, 12, 14, and 27 due to radiation therapy and the risk of osteoradionecrosis.
After the extraction sites healed, the decision was made to proceed with a mandibular fixed restoration without the addition of the implant in the area of No. 27. Although not considered to be an ideal solution, the clinician determined that the four existing implants would provide adequate support without the additional implant at No. 27 (Figure 6). Obtaining impressions of the mandibular implants proved highly challenging because of the patient's very limited opening and the non-parallel angulations of the implants. Use of an open-tray impression with pick-up copings has been shown to render the greatest accuracy,12 however this was not possible to do in this case due to the limited opening and tissue fragility (Figure 8).
A closed-tray impression ultimately was successful, and a milled titanium bar was fitted and utilized with nanohybrid composite for a fixed, screw-retained mandibular restoration (Figure 9 and Figure 10). With consideration given to the advice from the referring OMS, a maxillary RPD was fabricated rather than risk potential osteoradionecrosis (Figure 11). With the e.max crowns having already been seated on teeth Nos. 5 and 13, rest preparations and guide planes were created intraorally with a handpiece to accommodate the maxillary RPD.
Discussion
This patient presented a challenging medical and dental history that directly impacted his dentition. Xerostomia, limited range of motion in the TMJ, and a significant medication regimen contributed to his high caries rate and tooth loss. Dental implants had been placed by two different surgeons at different times using two different implant systems. Adding to the confounding nature of this case, the implants had been placed at dissimilar depths and varying angles, making the restorative phase rather difficult.
Because of the patient's xerostomia the option of using a removable complete mandibular denture was a poor choice for patient comfort and function. In fact, during the healing phase the existing mandibular ICD rested on the healing abutments and Locator-style abutment on No. 29, which helped minimize tissue irritation and discomfort. The screw-retained, fixed mandibular arch restoration was successfully delivered, and the patient was very pleased with the comfort and function. He remains pleased with it as of this writing.
Due to the concerns of the OMS with regard to implant placement, the maxillary RPD was a compromise. The patient, however, has remained relatively comfortable because the remaining dentition provides reasonable stability (Figure 11 through Figure 13). As a result of the oral-pharyngeal cancer radiation therapy, salivary gland function has decreased further and the patient will be closely monitored for any new caries activity. The final outcome, including the closure of the diastema between teeth Nos. 8 and 9, is shown in Figure 14 and Figure 15.
Conclusion
Although single-tooth dentistry may often be appropriate, when the patient's biological system is failing, a broader, more comprehensive perspective is needed. An accurate history and diagnosis and thorough risk assessment are crucial to achieving a predictable outcome. Today, patients have access to an array of clinical providers and varied treatment systems. Restorative clinicians must take the time to "decode" the patient's history in order to utilize the correct armamentarium to manage treatment.
Acknowledgment
The author thanks Claudio Bucceri, CDT, of Swiss Dental and Technical Art, Seattle, Washington, for his laboratory expertise, and Matt Falkenstein, DDS, for his guidance.
About the Author
Bryan Nakagawa, DMD
Clinical Instructor, Kois Center, Seattle, Washington; Private Practice, Salem, Oregon
References
1. Wijdicks EF, Klein CJ. Guillain-Barré Syndrome. Mayo Clin Proc. 2017;92
(3):467-479.
2. Crincoli V, Fatone L, Fanelli M, et al. Orofacial manifestations and temporomandibular disorders of systemic scleroderma: an observational study. Int J Mol Sci. 2016;17(7):E1189.
3. Silvestre-Rangil J, Bagán L, Silvestre FJ, Bagán JV. Oral manifestations of rheumatoid arthritis. A cross-sectional study of 73 patients. Clin Oral Investig. 2016;20(9):2575-2580.
4. Marsh PD. Dental plaque as a biofilm: the significance of pH in health and caries. Compend Contin Educ Dent. 2009;30(2):76-87.
5. Lankarani KB, Sivandzadeh GR, Hassanpour S. Oral manifestation in inflammatory bowel disease: a review. World J Gastroenterol. 2013;19(46):8571-8579.
6. Nunes H, Bouvry D, Soler P, Valeyre D. Sarcoidosis. Orphanet J Rare Dis. 2007;2:46.
7. Hayes M, Da Mata C, Cole M, et al. Risk indicators associated with root caries in independently living older adults. J Dent. 2016;51:8-14.
8. Lynge Pedersen AM, Belstrøm D. The role of natural salivary defenses in maintaining a healthy oral microbiota. J Dent. 2019;80(suppl 1):S3-S12.
9. Zero DT, Brennan MT, Daniels TE, et al. Clinical practice guidelines for oral management of Sjögren disease: dental caries prevention. J Am Dent Assoc. 2016;147(4):295-305.
10. Papageorgiou SN, Papadelli AP, Koidis PT, Petridis HP. The effect of prosthetic margin location on caries susceptibility: a systematic review and meta-analysis. Br Dent J. 2013;214(12):617-624.
11. Tota JE, Best AF, Zumsteg ZS, et al. Evolution of the oropharynx cancer epidemic in the United States: moderation of increasing incidence in younger individuals and shift in burden to older individuals. J Clin Oncol. 2019;37(18):1538-1546.
12. Phillips KM, Nicholls JI, Ma T, Rubenstein J. The accuracy of three implant impression techniques: a three-dimensional analysis. Int J Oral Maxillofac Implants. 1994;9:533-540.