How Should Care at an Early Age/Medical Management of Dental Caries Be Handled?
Joel H. Berg, DDS, MS; Joshua A. Bresler, DMD; Constance M. Killian, DMD
Dr. Berg
When considering dental care at an early age, the conceptual framework for medical management of dental caries comes into play. It must be remembered that caries is a progressive disease. It is the process of demineralization of tooth structure mediated through bacterial acid production. Without even discussing the nuances of the microbiological etiologies and other behavioral aspects of dental caries, one can consider its progression and various stages.
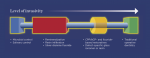
Figure 1 shows the "caries management continuum," in which the treatment of dental caries is seen as responsive to the phase of progression of the disease. "Traditional operative dentistry," at the bottom right portion of the graphic, represents the latest phase of treatment of dental caries. At this late stage, one is not actually treating the disease but, rather, the results of the disease. Indeed, most of dentistry, and, subsequently, most of the cost of dentistry is related to treating the results of dental caries and not the disease itself. Thus, needing to perform traditional operative dentistry, or any other form of restorative dentistry, including most prosthodontics, endodontics, etc, means that the disease has been allowed to progress to its full extent, resulting in cavitation of tooth structure.
Based on Figure 1, management of the disease would be less invasive at any point on the continuum to the left of traditional operative dentistry. The level of invasiveness can be characterized by the least invasive measure one could employ at the various stages of progression of the disease. Therefore, if a patient had a virulent pathogen in his or her mouth that when combined with other elements caused rapid progression of dental caries, the treatment approach should be microbial control (far left of the continuum). Microbial control entails reducing the load of microorganisms and includes behavioral aspects of disease prevention such as oral hygiene practices. In the future, this may also include treatment of the microbial biofilm within the individual with various forms of treatments, most yet to be identified. Management of saliva is also exceptionally important but often gets overlooked even though saliva is both the mediator and controller of disease in the instance of large loads of free biofilm existing in saliva. Saliva can be managed in terms of its volume and consistency, including the elements in it.
Progressing along the continuum, remineralization is used when more sensitive and specific detection methods are needed. The disease can be managed in a very specific way using demineralization tools to identify if treatments were indeed effective. Resin infiltration, a fairly recent though validated innovative concept, is a means of halting progression of interproximal and other smooth-surface caries lesions to avoid progression. Meanwhile, the use of silver diamine fluoride (SDF) has gained popularity recently. Although SDF, formerly known as silver nitrate, is actually a caries lesion therapy in that it treats the biofilm by killing it and, therefore, disallows progression of disease, it is most often deployed in the late stages of disease. Use of agents that halt the progression of disease prior to the occurrence of cavitation of tooth structure would be preferable. Such products include SDF and several others that are under development and not currently available on the market.
This continuum of medical management of caries allows one to visualize the ways in which clinicians may tackle the caries problem in various stages of disease progression. It may also prompt developers of pharmaceuticals and other products to strategically examine what might be done to enable better results in terms of preventing cavitation and destruction of tooth structure.
Dr. Bresler
Dentists who serve the pediatric community see a wide range of patients. They treat newborns who are hours old with natal teeth or atypical frenum attachments that inhibit feeding and adult patients with special needs who may be 50 years old but are developmentally age 3 or 4. Many patients pediatric dentists encounter also may have complex medical histories that can impact the way care is provided.
A clinician's interaction and partnership with medical counterparts is essential for the patient to receive comprehensive healthcare that includes oral healthcare. Pediatricians should be able to clearly explain the priority and importance of oral healthcare to their patients. Dental caries is the most common chronic disease among children, with more than 60% experiencing dental decay by age 5.1 All children should establish a dental home by their first birthday.
On average, pediatricians will see a healthy patient eight times by the time the child is 12 months old.2 With the first teeth erupting at around 5 to 6 months, the medical team will have ample opportunity to evaluate the early dentition. Early dental anticipatory guidance is often time-consuming and more effectively and efficiently handled at the dental office. Essential components of early dental visits include stressing the importance of proper oral hygiene, optimizing topical and systemic fluoride exposure, nutritional counseling to minimize prolonged or frequent sugar exposure, and early discussions about teething, non-nutritive oral habits, dental trauma/injury prevention, and occlusion. Patients who are seen early will receive a solid foundation of the tools needed to prevent oral disease.
For young patients with systemic disease, early interaction by the clinician with the patient's pediatrician or primary care medical provider is necessary to understand the exact medical diagnoses so the clinician can adjust the patient's treatment plan, as appropriate. Pediatric dentists see many young patients with cardiac disease, respiratory issues, cerebral palsy, seizure disorders, bleeding problems, allergies, behavioral issues, and other medical diagnoses that can significantly affect treatment modalities, the use of local anesthetics or sedation procedures, and the prescribing of medications. Parents, unfortunately, often are undependable or not in a position to evaluate and communicate cogent medical information to the pediatric dentist. The author, for example, once had parents report no medical issues, but upon examining the patient, a thoracotomy scar was noticed. Only upon further investigation was it discovered that the patient had hypoplastic left heart syndrome, one of a few cardiac diagnoses that usually requires subacute bacterial endocarditis (SBE) prophylaxis.
A pediatric dental practice should require current history and physicals for all patients who will be treated with sedation or general anesthesia. Information obtained from the patient's primary care provider will help to ensure that the dental office has current and accurate medical data, which will enable the highest level of safe care to be provided. Additionally, for patients with significant systemic disease, consultation with their medical specialist is often required to formulate surgical plans specific to the patient and dental treatment rendered.
The partnership between dentist and physician is crucial to ensure that patients establish a dental home by their first birthday. This enables the dentist to focus on preventative care to help the patient avoid dental disease.
Dr. Killian
Dentists who treat children have long recognized that the tradition of the first dental visit at age 3 is woefully inadequate. By that age the oral flora responsible for caries is well established, and behaviors that promote oral disease may result in significant oral health problems. Thus, in 1986 the American Academy of Pediatric Dentistry made a bold and critical recommendation that the first dental visit occur within 6 months of the eruption of the child's first tooth. The primary goal of this visit is to establish a dental home where routine and emergency services and specialty referrals are provided and where parents can receive timely preventative information for their child.
The age 1 visit is an opportunity for the dentist to build a relationship with the family of the child and promote behaviors that are conducive to oral health. Components of this visit include information gathering, which encompasses medical history and risk assessment questions; oral examination of the child; and development of a risk profile for the child with recommendations and anticipatory guidance.
During the information gathering, the dentist or a team member reviews the medical history, which should include questions about the prenatal and perinatal period of the child's development. Risk assessment questions should comprise the following topics: family history of caries (especially maternal/primary caregiver history), child's dietary habits (with attention given to between-meal, sugar-containing snacks or beverages), child's oral hygiene habits, whether or not the child is put to bed with a bottle containing sweetened liquid or breast feeds on-demand throughout the night, special healthcare needs, fluoride exposure, regular dental care, non-nutritive oral habits, and history of orofacial injury.
If the child is sitting on the parent's lap at this time and becomes impatient, having a small book or toy on hand to entertain the child may help the parent focus on the discussion. As the parent observes the dentist's interactions with the child, parental trust and confidence may be earned as the dentist demonstrates not only knowledge about oral health, but also an understanding of child behavior. It is important that the dentist and parent work together as a team to care for the child.
While the risk assessment form outlines risk factors, the oral examination provides evidence of the child's specific clinical condition. The clinician should examine hard and soft tissues, noting soft-tissue attachments and any alterations related to non-nutritive oral habits. Teeth that are erupted should be noted, dental anatomy and any anomalies or alterations in tooth structure (such as hypoplasia or decalcification) evaluated, and the presence of plaque assessed. These findings will be used in development of the risk profile.
The final step of the age 1 visit is to create and review the risk profile specific to the child and provide anticipatory guidance. AAPD provides an example of a caries risk assessment form,3 which can be easily completed during the appointment and reviewed with the parent. The parent learns the particular needs, recommendations, and behaviors that must be met to prevent oral disease for the child. Simple but practical advice can be provided regarding each specific risk factor, such as giving tips on positioning the child for toothbrushing. If oral disease is noted during the examination, the parent must be informed and given options for therapeutic management. Based on the risk profile, an interval for the next oral health visit is determined: 3 months for a child with high risk and up to 6 to 12 months for a child with low risk.3 Of course, the parent should be told to contact the office should any questions, concerns, or injuries arise.
The age 1 visit initiates the journey toward a lifetime of optimal oral health for the child, and once the dental home is established, the dentist can provide the knowledge and care to assist the family on this journey.
About the Authors
Joel H. Berg, DDS, MS
Professor, Department of Pediatric Dentistry, School of Dentistry, University of Washington, Seattle, Washington; Past-President, American Academy of Pediatric Dentistry; Diplomate, American Board of Pediatric Dentistry
Joshua A. Bresler, DMD
Assistant Professor of Pediatric Dentistry, Temple University Kornberg School of Dentistry, Philadelphia, Pennsylvania; Assistant Professor of Pediatric Dentistry, University of Pennsylvania School of Dental Medicine; Philadelphia, Pennsylvania; Diplomate, American Board of Pediatric Dentistry; Fellow, American Academy of Pediatric Dentistry; Private Practice, Philadelphia, Pennsylvania
Constance M. Killian, DMD
Adjunct Associate Professor, Division of Pediatric Dentistry, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania; Diplomate and Past-President, American Board of Pediatric Dentistry; Fellow, American Academy of Pediatric Dentistry; Private Practice, Doylestown, Pennsylvania