Simplified Fabrication of an Esthetic Implant-Supported Crown With a Novel CAD/CAM Glass Ceramic
Julián Conejo, DDS, MSc; and Markus B. Blatz, DMD, PhD
Abstract: Implant therapy and CAD/CAM technologies are advancing quickly, providing predictable esthetic and functional treatment options. A recent development involves the use of zirconia-reinforced lithium-silicate ceramic for fabrication of implant-supported restorations. Suitable for monolithic crowns, the material provides the optical advantages of a silicate ceramic with improved physical strength. Several prerequisites, however, are necessary to fabricate screw-retained monolithic restorations in the anterior maxilla. This case report demonstrates the clinical steps to fabricate a monolithic ceramic CAD/CAM crown on an immediately placed dental implant in the esthetic zone.
Proper planning is the first and arguably most important step when treating a patient with dental implants in the esthetic zone. This includes selecting the most appropriate restorative materials.
When immediate implant placement is considered, evaluation of the extraction socket and buccal plate, as well as soft-tissue thickness and height, provides valuable determinants for long-term success and tissue stabilty.1 From a restorative perspective, prosthetic reconstruction dentistry should always aim to replicate natural morphology, texture, and color to match the adjacent dentition.2 Lithium-disilicate ceramic has become an extremely popular choice for single-unit restorations. It is preferred for monolithic crowns, providing excellent long-term success and overcoming some of the shortcomings reported for veneered bilayer all-ceramic restorations.3
A recent development is a zirconia-reinforced lithium-silicate (ZLS) ceramic that potentially offers excellent esthetics, good physical properties, high edge stability, and simple CAD/CAM fabrication. While independent scientific proof is still sparse, the novel glass ceramic seems to present a viable material option for use in monolithic implant restorations. ZLS can be milled in chairside and laboratory milling units, which significantly simplifies the fabrication and customization and eliminates numerous laboratory steps, making it a more predictable procedure.4 Starting with treatment planning and implant positioning, the dental team needs several prerequisites to fabricate screw-retained monolithic restorations in the anterior maxilla.
This case report demonstrates the clinical steps to fabricate a monolithic CAD/CAM ceramic crown on an immediately placed dental implant in the esthetic zone.
Case Presentation
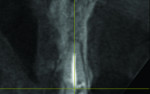
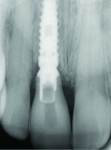
A 55-year-old female presented with a failing maxillary right central incisor, which had been previously endodontically treated and restored with a metal post and a porcelain-fused-to-metal crown (Figure 1 and Figure 2). After clinical and radiographic examination, a root fracture was observed. The root fracture was confirmed with cone-beam computed tomography (CBCT) scan (Orthophos XG 3D, Sirona Dental, www.sirona.com), which also revealed an intact buccal plate with a thickness of approximately 1 mm (Figure 3).
After a detailed diagnosis, the site was classified as a type 1 socket with the soft tissues and buccal plate intact.1 A minimally traumatic tooth extraction was performed, and the extraction socket condition was clinically evaluated. Measurement with a periodontal probe indicated a vertical distance of 3 mm from the buccal plate to the gingival margin. Because of the favorable condition of the socket walls and soft tissues, an immediate implant was placed.
Pilot drilling and implant-bed preparation should follow a palatal approach to avoid inadvertently damaging the buccal plate, which is critical in supporting a long-term stable soft-tissue architecture.5 The approach is to place the implant slightly palatally to the long axis, ie, the incisal edge of the prospective tooth. This position prevents not only damage to the buccal bone but also allows for fabrication of a screw-retained restoration without compromising the esthetic outcome. The screw-access hole can be placed in the area of the cingulum, not in the area of the incisal edge or labial aspect of the prospective restoration.
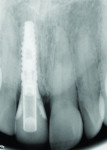
The implant shoulder should be 3 mm to 4 mm apical from the gingival margin.5 A wide-diameter implant should be avoided to maintain the interproximal bone and provide a greater distance between the labial implant surface and the buccal bone, thereby preserving and stabilizing the surrounding soft tissues.5 A tapered implant (3.8 mm x 12 mm) with buttress threads (Tapered Internal Plus, BioHorizons, www.biohorizons.com) that featured Laser-Lok® microchannel technology (BioHorizons) was placed, and a high primary stability of more than 45 N/cm2 was achieved (Figure 4).6 The space between the implant and bone walls was filled with a xenograft (MinerOss® X Particulate, BioHorizons) to compensate for the buccal plate remodeling after the tooth extraction (Figure 5).
A screw-retained immediate provisional crown was delivered (Figure 6), ensuring the absence of any occlusal contacts during maximum intercuspation and functional movements.7 The fixation screw was torqued as recommended by the manufacturer at 30 N/cm2 to avoid micromovements during osseointegration. The screw-access opening was covered with Teflon™ tape and a light-cure temporary material (Clip, VOCO, www.voco.com).
After 5 months, the implant site and provisional crown were reevaluated. Healthy and stable soft tissues were observed. The dimensions of the provisional crown and gingival margin were compared with the contralateral tooth (Figure 7).
The shade for the definitive crown was determined with a spectrophotometer (VITA Easyshade®, VITA Zahnfabrik, www.vita-zahnfabrik.com) and traditional shade tabs (3D-MASTER®, VITA Zahnfabrik). Subsequently, the provisional crown was removed to make an impression for fabrication of the final restoration. The emergence profile was transferred with a customized impression coping, which was made with a flowable composite (Grandio® Flow, VOCO) to support the soft-tissue architecture during the impression making (Figure 8 and Figure 9).
CAD/CAM Procedures
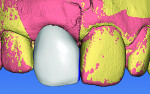
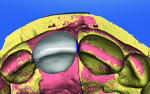
A titanium insert (Titanium Base Abutments, BioHorizons) was placed on the implant analog, and the stone model was scanned. Then, a scan of the soft-tissue replica material was performed to capture the gingival contours. The BioReference tool in the design software (InLab 4.2, Sirona Dental) provided an adequate initial crown proposal (Figure 10 and Figure 11).
The final restoration was milled in a laboratory milling system (MC XL, Sirona Dental) from a ZLS ceramic (SUPRINITY® LT, VITA Zahnfabrik). This material represents a new generation of glass ceramics enriched with zirconia (approximately 10% by weight). It offers a flexural strength of 495 MPa,8 making it similar to lithium-disilicate ceramics but with improved edge stability during milling and simplified processing. The esthetic properties are characterized by its inherent translucency and opalescence.
After esthetic try-in and stain-and-glaze procedures, the monolithic crown was bonded to the titanium insert with a resin cement (Bifix, VOCO) (Figure 12). Air-particle abrasion of the titanium surface, combined with hydrofluoric acid etching (20 seconds) and salinization (60 seconds) of the ceramic surface, provided improved mechanical interlocking and a stronger bond.9
The final restoration was torqued into the implant at 30 N/cm2, and the screw-access hole was covered with Teflon tape and composite resin (Grandio) (Figure 13 and Figure 14).
Discussion
Traditional prefabricated titanium abutments and cast-gold personalized abutments show good mechanical properties but result in deficient esthetic outcomes when thin periodontal biotypes are present. Zirconia hybrid abutments composed of a zirconia mesostructure bonded to a titanium insert show good esthetic results and biocompatibility with soft tissues. If an angulated implant needs to be restored, a CAD/CAM hybrid abutment with a shoulder that follows the soft-tissue contours and a cement-retained crown should be considered. The margin position is crucial for excess cement removal. The zirconia abutment–titanium implant interface may be susceptible to wear of the abutment coupled with deformation of the implant neck greater than that associated with a conventional titanium abutment–titanium implant interface under dynamic loading.10 Full zirconia abutments with internal hex and Morse conical connections show higher fracture rates than hybrid abutments.11
The new monolithic screw-retained implant crown described combines the esthetic and functional advantages of the zirconia hybrid abutments with a faster and more economical elaboration process. Screw-retained restorations are more easily retrieved and biologically safer than cement-retained restorations because the possibility of leaving excess cement around the implant is eliminated.12 Proper 3D implant placement is crucial to avoid the screw-access hole from being visible at the labial surface.
By following established guidelines for implant therapy in the esthetic zone, the clinician can achieve functional restorations with high esthetics. Understanding the biology of the mouth and the peri-implant structures can help clinicians perform less invasive treatments with high success rates. When an intact socket, buccal plate, and soft tissues are present, an immediate implant is a possible treatment option. If any of these structures is flawed, a regenerative procedure with a delayed approach is indicated.13
New CAD/CAM software and ceramic materials support clinicians and dental technicians in delivering natural-looking restorations more rapidly. ZLS ceramics are another option for implant-supported monolithic restorations because of their high flexural strength. Occlusal adjustments and contour modifications must be performed before the crystallization process. Glazing can compensate for the effect of minor surface damages.8 Traditional laboratory concepts of color replication, morphology, and texture remain crucial for achieving high esthetics.
Conclusion
With the advances in dental ceramic materials for CAD/CAM technology along with the established protocols for implant therapy in the esthetic zone, clinicians are able to obtain natural-appearing and functional restorations in a more timely fashion with high success rates.
Acknowledgements
Dental technicians Angelica Niño and Angie Benambur provided the laboratory work in this case report.
Disclosure
Julián Conejo, DDS, MSc, has received grant/research support from VITA Zahnfabrik.
About the Authors
Julián Conejo, DDS, MSc
Visiting Scholar
Department of Preventive and Restorative Sciences
University of Pennsylvania School of Dental Medicine
Philadelphia, Pennsylvania
Markus B. Blatz, DMD, PhD
Professor of Restorative Dentistry
Chairman
Department of Preventive and Restorative Sciences
University of Pennsylvania School of Dental Medicine
Philadelphia, Pennsylvania
References
1. Elian N, Cho SC, Froum S, et al. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104.
2. Gracis S, Fradeani M, Celletti R, Bracchetti G. Biological integration of aesthetic restorations: factors influencing appearance and long-term success. Periodontol 2000. 2001;27:29-44.
3. Pieger S, Salman A, Bidra AS. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review. J Prosthet Dent. 2014;112(1):22-30.
4. Sartori N, Tostado G, Phark J, et al. CAD/CAM high-strength glass-ceramics. Quintessence of Dental Technology. 2015;38:39-54.
5. Gamborena I, Blatz MB. Evolution: Contemporary Protocols for Anterior Single-Tooth Implants. Hanover Park, IL: Quintessence Publishing Co Inc; 2015
6. Romanos GE. Advanced immediate functional loading: requirements for long-term success in modern implant dentistry. Compend Contin Educ Dent. 2014;35(7):474-483.
7. Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524-534.
8. Gödiker M, Coldea A, Just B, et al. Damage tolerance of glass ceramics associated with thermal treatment [abstract]. J Dent Res. 2014;93(spec iss B). Abstract 299.
9. Spitznagel FA, Horvath SD, Guess P, Blatz MB. Resin bond to indirect composite and new ceramic/polymer materials: a review of the literature. J Esthet Restor Dent. 2014;26(6):382-393.
10. Cavusoglu Y, Akça K, Gürbüz R, Cehreli MC. A pilot study of joint stability at the zirconium or titanium abutment/titanium implant interface. Int J Oral Maxillofac Implants. 2014;29(2):338-343.
11. Delben JA, Barao VA, Ferreira MB, et al. Influence of abutment-to-fixture design on reliability and failure mode of all-ceramic crown systems. Dent Mater. 2014;30(4):408-416.
12. Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol. 2009;80(9):1388-1392.
13. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19 suppl:43-61.