Cone-Beam Computed Tomography–Guided Management of C-Shaped Type III Dens Invaginatus With Peri-invagination Periodontitis in a Maxillary Canine: A Case Report
Priya Mittal, MDS; Ganesh Ranganath Jadhav, MDS; Shibli Syed, MDS; and Nikita D. Bhujbal, BDS
Abstract
Dens invaginatus (DI) is a developmental anomaly seen infrequently in maxillary canines. This article describes cone-beam computed tomography-guided nonsurgical management of type III (subtype B) DI in a permanent maxillary canine associated with a sinus tract and peri-invagination periodontitis in a 17-year-old female. After gaining access to the root canal, thorough chemo-mechanical preparation was performed and usage of intracanal medicament of calcium hydroxide was prescribed for 3 weeks, during which the sinus tract healed completely. Obturation was completed by a technique of down-packing master-cone gutta-percha, followed by backfilling with thermoplasticized gutta-percha. At 12-months follow-up, the patient was asymptomatic with complete resolution of the sinus tract and radiographic evidence of healing of periapical pathology.
Dens invaginatus (DI) is a developmental anomaly resulting from the invagination of an enamel organ into the dental papilla before tooth mineralization.1 It is presented as a small pit, fissure, or deep invagination into the root with prevalence of 0.3% to 10%.2 The permanent maxillary lateral incisor is most commonly affected followed by the permanent maxillary central incisor; however, maxillary canines are also invaginated on rare occasions.1 Enamel and dentin present in the invagination is hypomineralized, which increases the tooth’s susceptibility for caries and periodontal involvement.
Oehler3 classified DI according to its severity as: type I, confined within the crown; type II, invades the root but remains confined as a blind sac; and type III, penetrates through the root and communicates with the periodontal ligament space either laterally (subtype A) or apically (subtype B). Oehler’s type III lesions are prone to evoke an inflammatory response within the periodontal tissue, giving rise to a “peri-invagination periodontitis.”4 In such cases thorough chemo-mechanical preparation is difficult. If the nonsurgical endodontic treatment fails as in the most severe forms of type III invaginatus, surgical intervention is needed.5 To date, no case of C-shaped Oehler’s type III DI in maxillary canines has been reported in the literature.
This case reports cone-beam computed tomography (CBCT)-guided nonsurgical management of type III (B) DI in a permanent maxillary canine associated with a sinus tract and peri-invagination periodontitis.
Case Report
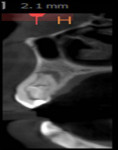
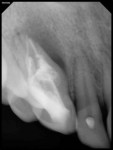
A 17-year-old healthy female was referred for the management of a persistent vestibular sinus tract in the periapical area labially in relation to the permanent maxillary right canine (tooth No. 6). The patient’s general dentist had started root-canal treatment of teeth Nos. 6 and 7 but did not complete the treatment. Tracer radiographic examination revealed the origin of the sinus tract to be in the apical end of an invagination with respect to tooth No. 6 (Figure 1 and Figure 2). This invagination extended into the root surface apically and was associated with large peri-invagination radiolucency.
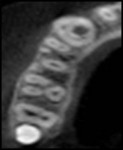
The relationship between the invagination–pulp canal space and the exact origin of the radiolucency was not entirely clear from the conventional radiographs. Therefore, a limited-area CBCT scan of the maxilla was advised to better understand the internal anatomy of the tooth. The benefits and risks of the CBCT scan were explained to the patient, and written informed consent for the CBCT scan was obtained. The scan revealed two canals: the main canal located palatally (Figure 3), and an invaginated, C-shaped, enamel-lined canal that interconnected with the periodontal ligament space labially in the apical area. Invagination was also interconnecting with the main canal through a thin channel (Figure 4). The invagination was associated with a periradicular lesion and a perforated labial cortical plate. Although the incisal portion of the crown was within normal limits regarding its form and size, the crown and root below the site of the invagination appeared markedly dilated. The abnormality present in the tooth and the possible need for surgical intervention was explained to the patient.
The tooth was re-accessed under rubber dam isolation (Figure 5), and a working length radiograph was taken (Figure 6). The C-shaped invagination was prepared by circumferential filing using an International Organization for Standardization (ISO) #30 K-file. The round canal was prepared using a crown-down technique, to a ProTaper® F3 hand file (DENTSPLY Maillefer, www.dentsplymaillefer.com). Throughout the procedure, copious irrigation was performed using 2.5% sodium hypochlorite solution (Cmident, India) and 15% ethylenediaminetetraacetic acid (EDTA) (Largal Ultra, Septodont, www.septodont.com). Inter-appointment medicament of calcium hydroxide (Prime Dental Products Pvt. Ltd., www.prime-dental.com) was given for 3 weeks, during which time the sinus tract healed completely. Obturation was completed by a technique of down-packing master-cone gutta-percha followed by backfilling with thermoplasticized gutta-percha (Calamus Obturation System, DENTSPLY Maillefer) (Figure 7).
The tooth was restored using light-cured composite resin (Z100™ Restorative, 3M ESPE, www.3MESPE.com). At the 12-month follow-up, the patient was asymptomatic with complete resolution of the sinus tract. A periapical radiograph revealed healing of periapical pathology (Figure 8).
Discussion
This article presents CBCT-guided diagnosis and nonsurgical endodontic management of an unusual case of C-shaped Oehlers type III (B) DI with peri-invagination periodontitis in a maxillary canine. The main canal and enamel-lined C-shaped invagination associated with large periradicular radiolucency and a thin channel were diagnosed in sagittal (Figure 3) and transverse (Figure 4) CBCT sections. DI poses a treatment challenge for effective chemo-mechanical preparation and obturation because isthmi and recesses present in such cases are difficult to clean. In the presented case, the invaginated C-shaped canal was cleaned using circumferential filing with copious irrigation so as to clean interconnecting thin channels, and obturation was done using thermoplasticized gutta-percha.
DI presents an unusual radiographic appearance that may lead to diagnostic difficulties and uncertainties regarding the root canal system, which ultimately affects selecting the appropriate treatment plan.6 CBCT uses an effective yet low radiation dose and generates undistorted 3-dimensional reconstruction of the teeth and their surrounding tissues that helps in early detection of the origin and size of periapical pathology.7 Therefore, in the presented case a CBCT scan was taken, which provided an accurate extent of an invagination and its relationship to the peri-invagination radiolucency and main canal.
Various theories proposed for the formation of DI include infection, trauma, external forces (such as adjacent tooth germ), generic factors, growth pressure of the dental arch, growth failure of inner enamel epithelium, rapid and aggressive proliferation of a part of the inner enamel epithelium, distortion of the enamel organ, fusion of two tooth germs, etc.1 In most cases, DI remains asymptomatic in early stages; however, it may be associated with acute pain or a draining sinus. Generally, it is diagnosed incidentally during routine clinical (morphologic alteration of the crown or a deep lingual pit) or radiographic (a tooth within a tooth appearance) examination. DI affects symmetrical teeth and, hence, the contralateral tooth should be examined. It is also susceptible to the development of dental caries and may provide a portal of entry for irritants.
In the documented case, the periapical pathology was developed primarily because of the presence of a large-sized, C-shaped DI present labially as evident from the CBCT scan. This was the reason for labial bone loss and the presence of a sinus tract labially. Moreover, the thin channel within the enamel of the DI interconnected directly with the main canal and, hence, pulpitis and necrotic pulp was reported.
About the Authors
Priya Mittal, MDS
Senior Resident
Department of Conservative Dentistry and Endodontics
Centre for Dental Education and Research
All India Institute of Medical Sciences
New Delhi, India
Ganesh Ranganath Jadhav, MDS
Lecturer
Department of Conservative Dentistry and Endodontics
Sinhgad Dental College and Hospital
Pune, India
Shibli Syed, MDS
Private Practitioner
Pune Orthodontics
Nikita D. Bhujbal, BDS
Private Practitioner
Pune Orthodontics
References
1. Hülsmann M. Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30(2):79-90.
2. Alani A, Bishop K. Dens invaginatus. Part 1: classification, prevalence and aetiology. Int Endod J. 2008;41(12):1123-1136.
3. Oehlers FA. Dens invaginatus (dilated composite odontome). I. Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med Oral Pathol. 1957;10(11):1204-1218.
4. Thakur S, Thakur NS, Bramta M, Gupta M. Dens invagination: A review of literature and report of two cases. J Nat Sci Biol Med. 2014;5(1):218-221.
5. Nallapati S. Clinical management of a maxillary lateral incisor with vital pulp and type 3 dens invaginatus: a case report. J Endod. 2004;30(10):726-731.
6. Štamfelj I, Kansky AA, Gašperšic D. Unusual variant of type 3 dens invaginatus in a maxillary canine: a rare case report. J Endod. 2007;33(1):64-68.
7. Al-Rawi B, Hassan B, Vandenberge B, Jacobs R. Accuracy assessment of three-dimensional surface reconstructions of teeth from cone beam computed tomography scans. J Oral Rehabil. 2010;37(5):352-358.