The Teamwork Approach to Esthetic Tooth Replacement with Immediate Implant Placement and Immediate Temporization
Barry P. Levin, DMD; and Brian L. Wilk, DMD
Abstract: Enduring a period of edentulism between extraction and final restoration is difficult for patients— especially when it concerns the esthetic zone. The approach described demonstrates key points of consideration when replacing a maxillary anterior tooth with a dental implant using immediate implant placement, hard- and soft-tissue augmentation, and provisionalization. The authors stress adherence to patient selection and prosthetic design guidelines, and recommend the use of a digital impression technique, rather than traditional, rubber-based impressions.
The challenge of replacing a tooth in esthetically sensitive areas is exacerbated during the period between extraction and delivery of the definitive restoration. When implants can be placed into the extraction socket immediately after extraction, the treatment period is shortened compared to delayed protocols. Regardless of the advantages of immediate placement, some period of edentulism is frequently endured by the patient. Provisionalization of immediate implants can circumvent this problem. In a case series, Norton1 showed the predictability of immediate temporization in the esthetic zone in terms of stable peri-implant bone levels up to 9 years after therapy. The current authors2 demonstrated the success of immediate placement and temporization in terms of bone maintenance at 12 months loading with the final restoration.
One of the other advantages of this technique is the conditioning of soft tissues from the outset of treatment. Becker et al3 demonstrated how provisionalization of immediate implants can develop favorable emergence profiles prior to fabrication of the final restoration. Relative to conventionally loaded implants, Shibly et al4 demonstrated comparable success with immediately loaded implants in a clinical study.
In a 1-year study, Cosyn et al5 demonstrated the success of immediate implant placement and screw-retained temporization. Of note, they treated patients with thick periodontal biotypes and treated sites with postoperative recession with subepithelial connective tissue grafts. Other clinicians have found that routine placement of these autogenous tissue grafts results in more favorable esthetics compared to treatment without these grafts.6 Others have used autogenous bone grafts from distant sites to support facial soft tissues in compromised sites.7
In a case series, Valentini et al8 showed how immediate implant placement and simultaneous bone regeneration (bone xenograft and collagen membrane) can be successfully implemented with temporization at the time of implant placement.
At present, there is no consensus as to the most favorable method of preserving or augmenting peri-implant hard and soft tissues in these types of procedures. Regardless of how these sites are managed, some attempt at tissue preservation is recommended by the authors to avoid long-term esthetic complications.
The purpose of this case report is to demonstrate key points of consideration when replacing a maxillary anterior tooth with a dental implant. Implant timing, selection, method of placement, and management of hard and soft tissues are paramount to achieving success. Additionally, the method and timing of temporization, incorporation of technologies, and restoration are equally crucial to achieving a long-term, esthetic outcome.
Case Report
A 60-year-old man presented to his restorative dentist on an emergency basis with a fractured maxillary right canine (Figure 1). He had a history of periodontal, endodontic, and implant therapy, and had a heavily restored dentition with multiple fixed, tooth-supported, and implant-supported restorations. A portion of the prepared clinical crown, along with the prosthetic post, was attached to the porcelain-fused-to-metal crown (Figure 2). As a temporary measure, the post was recemented for esthetic purposes until surgical therapy could be initiated.
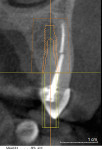
He presented to his periodontist’s office for extraction and implant therapy several days after his crown was recemented. Evaluation of his cone beam computed tomography (CBCT) scan revealed adequate apical and palatal bone to anticipate primary stability of an immediate implant (Figure 3).
Tooth No. 6 was extracted with care to preserve the thin, intact facial bone and integrity of the surrounding hard and soft tissues. After thorough debridement of the alveolus with ultrasonic and manual instrumentation, the socket was conditioned with a mixture of doxycycline and sterile saline. Once the alveolus was visually clear of soft-tissue remnants, a 13-mm-long implant with a longitudinal diameter of 3.6 mm and a conical portion coronally of 4.2 mm (4.2C x 13 mm [ASTRA TECH Implant System EV™; DENTSPLY Implants, www.dentsplyimplants.com]) was palatally positioned (Figure 4).
The implant was intentionally positioned palatally, avoiding contact with the thin facial bone, which consists almost entirely of bundle bone. The void between the facial implant surface and facial plate was obturated with a composite graft of mineralized bone allograft (SYMBIOS® Mineralized Cortical Powder, DENTSPLY Implants) and deproteinized bovine bone mineral (Bio-Oss®; Geistlich Pharma North America, www.geistlich-na.com) in a ratio of approximately 4:1 (Figure 5).
The xenograft was for an osteoconductive, though non-resorbing and space-maintaining, purpose. The graft material was placed level or slightly coronal to the fixture head.
A pick-up impression coping was fastened to the implant (Figure 6), and an open-tray impression (Position™ Penta™ Quick, 3M ESPE, www.3mespe.com) was taken; then an implant replica was attached (Figure 7), and the model was poured immediately. Digital scanning at the time of surgery was not indicated, as immediate temporization would not be possible. A core file would require fabrication, and laboratory steps would delay placement of a temporary restoration for several days.
After the impression was obtained, the site was confirmed to be free of any impression material. After removal of the impression coping and tray, the site was inspected, and additional bone graft particulate was added at the desired level of the top of the implant fixture to compensate for any material lost secondary to taking the impression. A subepithelial connective tissue graft was harvested from the palatal mucosa in the maxillary right quadrant. The graft was obtained with a single-incision technique, facilitating primary closure of the donor site and without an epithelial collar. Using a thin, periosteal elevator, the marginal portion of the facial soft tissue was gently reflected several millimeters in an envelope manner. The subepithelial connective-tissue graft was placed within this “pouch,” lying passively around a narrow, loosely fastened healing abutment (UniAbutment, DENTSPLY Implants). The graft was attached to the facial overlying soft tissue with a monofilament resorbable suture (Ethicon MONOCRYL suture, Ethicon, www.ethicon.com) (Figure 8). The application of the subepithelial connective-tissue graft was to augment the thickness of the peri-implant mucosa, not necessarily to widen the zone of keratinized tissue. Horizontal resorption, which could lead to esthetic compromise, even in thick-biotype patients, has been reported without soft-tissue augmentation.
Using the same suture material, the facial soft tissue was sutured over the connective-tissue graft, compressing the facial and soft tissues and covering a majority of the free soft-tissue graft (Figure 9). The first suture was used to secure the connective-tissue graft between the overlying soft tissue and crestal bone, and the second suture was used to compress the graft and reduce clot dimensions, as well as to achieve hemostasis.
After taking a “baseline” periapical radiograph (Figure 10), the patient was prepared to report to his restorative dentist, taking the poured cast containing the implant replica, which would facilitate provisionalization in vitro, rather than intraorally.
Postoperative instructions included ice pack application for the first 24 hours, systemic antibiotics (amoxicillin, 500 mg, 3 times a day for 10 days), systemic corticosteroids (methylprednisolone for 6 days), nonsteroidal anti-inflammatories for 3 days (etodolac, 400 mg), and 0.12% chlorhexidine rinses twice daily in place of manual toothbrushing for the first 10 days after surgery.
Prior to the initiation of surgical therapy, a vacuum-formed template had been fabricated on a maxillary cast used to facilitate previous restorative therapy (Figure 11). This template was then used to form a screw-retained provisional crown on the model containing the implant replica from the surgical impression. Bisacryl provisional material (Luxatemp® Ultra, DMG, www.dmg-dental.com) was flowed into the perforated vacuum-formed template after fixation of a temporary abutment to the implant replica (Figure 12).
Contact areas and the emergence profile of the temporary crown were developed on the cast, eliminating the need for repeated placement and removal intraorally, enhancing patient comfort. Great care was taken to confirm no occlusal contacts existed in maximum intercuspation and excursive movements.
At the patient’s first postoperative visit, 10 days after surgery, the sutures were removed, the area was gently polished with a rubber cup, and the patient was instructed on the “roll” brushing technique with an extra-soft toothbrush (GUM®, Sunstar, www.gumbrand.com). Over-the-counter essential-oil mouthwash (LISTERINE®, Johnson & Johnson, www.listerine.com) was recommended. The patient was also instructed not to perform any mastication for the next 4 weeks, when he would be returning for clinical and radiographic follow-up. Excellent incorporation of the soft-tissue graft and surrounding soft tissues around the provisional crown was noted (Figure 13).
After 4 months of hard- and soft-tissue maturation, a digital impression was taken. As an alternative to a conventional, rubber-based technique, a scanbody (ATLANTIS™ IO FLO, DENTSPLY Implants) was attached to the implant after removal of the provisional crown (Figure 14 and Figure 15).
With a digital scanner (iTero®, Align Technology, www.itero.com) capturing the position of the scanbody, a digital file was created, facilitating CAD/CAM fabrication of a custom zirconia abutment (ATLANTIS™, DENTSPLY Implants) (Figure 16).
The final crown, porcelain pressed to an all-zirconia core (zerion®, Straumann, www.straumann.com), was seated on the final abutment (Figure 17). Then the final crown was cemented onto the custom abutment (Figure 18).
Conclusion
The present case report demonstrates the efficacy of immediate implant placement, hard- and soft-tissue augmentation, and provisionalization. It is noteworthy that the patient had a thick periodontal biotype, a favorable occlusion scheme, and an intact extraction socket at the time of implant placement. The literature has shown severe esthetic complications even when bone augmentation is performed in these types of situations.10 The same group demonstrated stability of facial gingival levels in these types of cases when a subepithelial connective-tissue graft was used in conjunction with particulate bone grafts and immediate provisional crowns.11 Recently, Butler12 demonstrated the efficacy of autogenous connective-tissue grafts’ ability to compensate for the buccal plate diminution following extraction and implant placement.
Another aspect that is featured in this case report is prosthetic design. Abutment contour plays a crucial role, as does the submucosal portion of the crown, in soft-tissue health and esthetics. It is critical that the pressure exerted on the proximal and facial soft tissues is not excessive, leading to apical migration of the marginal mucosa. Recently, Steigmann et al13 presented an algorithm based on implant position and submucosal contours. Depending on the axial inclination and position of the implant platform in relation to the adjacent teeth, modifications to the submucosal contours should be customized. Labial or centered implants require varying degrees of concavity, and over-palatally positioned fixtures require a convex contour to support the soft tissues. These authors also emphasized the importance of provisional crowns to “sculpt” peri-implant soft tissues before delivery of the final restoration.
An additional aspect to this treatment, which is relatively current, is the digital impression technique, rather than traditional, rubber-based impressions. The accuracy of digital scanners when measuring soft-tissue parameters was recently demonstrated by Schneider et al.14 Ramsey and Ritter15 demonstrated the digital fabrication of a 3-dimensional model, facilitating fabrication of a virtual abutment with the production of a CAD/CAM-designed custom abutment and all-ceramic crown, delivered to the clinician, seated on a stereolithographic model. Recently, in an in vitro study, Gimenez et al16 demonstrated the accuracy of a parallel, confocal laser-based impression system, identical to the one used in this case report. They showed the accuracy of recapturing parallel and angled implants with the digital impression technique, noting, however, that accuracy decreased with “shallower” implant placement, as compared to those 2 mm to 4 mm subgingivally. Also, increasing the length of the scan led to slightly less accurate reproduction.
The obvious advantages to the digital impression technique include patient and operator comfort. The unpleasantness of rubber-based impressions is eliminated with this technology. The impression procedure is also of shorter duration, resulting in a more pleasant patient experience.
The distortion of conventional impression materials is not a factor with digital impressions, contributing to their accuracy. Also, distortion related to contraction of gypsum-based stone models is obviated. The virtual reproduction of a working cast, which facilitates virtual abutment design, negates the need to pour traditional models, shortening laboratory working time, and avoids the possible dimensional changes associated with these materials.
As with any procedure, case selection is critical to achieving optimal results. The patient featured in this case report was one with a thick periodontal biotype, lowering the risks of significant postoperative recession.17 The extraction socket was intact after tooth removal, and his occlusal scheme permitted the placement of a provisional restoration out of contact with the mandibular antagonist teeth. Had any of these criteria not been met, a deviation from the current procedure may have been necessary. This may have included flap reflection and concurrent guided bone regeneration, delayed placement with socket augmentation, or the need for a transitional removable partial denture.
About the Authors
Barry P. Levin, DMD
Diplomate
American Board of Periodontology
Clinical Associate Professor
Department of Periodontics
School of Dental Medicine
University of Pennsylvania
Philadelphia, Pennsylvania
Private Practice
Elkins Park, Pennsylvania
Brian L. Wilk, DMD
Private Practice
Chalfont, Pennsylvania
References
1. Norton MR. The influence of insertion torque on the survival of immediately placed and restored single-tooth implants. Int J Oral Maxillofac Implants 2011;26(6):1333-1343.
2. Levin BP, Wilk BL. Immediate provisionalization of immediate implants in the esthetic zone: A prospective case series evaluating implant survival, esthetics, and bone maintenance. Compend Contin Educ Dent. 2013;34(5): 352-361.
3. Becker W, Doerr J, Becker BE. A novel method for creating an optimal emergence profile adjacent to dental implants. J Esthet Restor Dent. 2012;24(6):395-400.
4. Shibly O, Kutkut A, Patel N, Albandar JM. Immediate implants with immediate loading vs. conventional loading: 1-year randomized clinical trial. Clin Implant Dent Relat Res. 2012;14(5):663-671.
5. Cosyn J, De Bruyn H, Cleymaet R. Soft tissue preservation and pink aesthetics around single immediate implant restorations: a 1-year prospective study. Clin Implant Dent Relat Res. 2013;15(6):847-857.
6. Grunder U. Crestal ridge width changes when placing implants at the time of tooth extraction with and without soft tissue augmentation after a healing period of 6 months: report of 24 consecutive cases. Int J Periodontics Restor Dent. 2011;31(1):9-17.
7. Da Rosa JCM, De Oliveira Rosa ACP, Francishone CE, Sotto-Maior BS. Esthetic outcomes and tissue stability of implant placement in compromised sockets following immediate dentoalveolar restoration: results of a prospective case series at 58 months follow-up. Int J Periodontics Restor Dent. 2014;34(2):199-208.
8. Valentini P, Abensur D, Albertini JF, Rocchesani M. Immediate provisionalization of single extraction-site implants in the esthetic zone: a clinical evaluation. Int J Periodontics Restor Dent. 2010;30(1):41-51.
9. Kan JY, Roe P, Rungcharassaeng K, et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011;26(4):873-876.
10. Roe P, Kan JY, Rungcharassaeng K, et al. Horizontal and vertical dimensional changes of peri-implant facial bone following immediate placement and provisionalization of maxillary anterior single implants: a 1-year cone beam computed tomography study. Int J Oral Maxillofac Implants. 2012;27(2):393-400.
11. Yoshino S, Kan JY, Rungcharassaeng K, et al. Effects of connective tissue grafting on the facial gingival level following single immediate implant placement and provisionalization in the esthetic zone: a 1-year randomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29(2):432-440.
12. Butler B. Masking buccal plate remodeling in the esthetic zone with connective tissue grafts: Immediate implant concepts, techniques. Compend Contin Educ Dent. 2014;35(7):486-493.
13. Steigmann M, Monje A, Chan HL, Wang HL. Emergence profile design based on implant position in the esthetic zone. Int J Periodontics Restor Dent. 2014;34(4):559-563.
14. Schneider D, Ender A, Truninger T, et al. Comparison between clinical and digital soft tissue measurements. J Esthet Restor Dent. 2014;26(3):191-199.
15. Ramsey CD, Ritter RG. Utilization of digital technologies for fabrication of definitive implant-supported restorations. J Esthet Restor Dent. 2012;24(5):299-308.
16. Gimenez B, Ozcan M, Martinez-Rus F, Pradies G. Accuracy of a digital impression system based on parallel confocal laser technology for implants with consideration of operator experience and implant angulation and depth. Int J Oral Maxillofac Implants. 2014;29(4):853-862.
17. Kan JY, Rungcharassaeng K, Lozada JL, Zimmerman G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: a 2- to 8-year follow-up. Int J Oral Maxillofac Implants. 2011;26(1):179-187.