Combining All-on-4 Treatment with CT-Guided Technology: Technique and Report of Three Cases
Abstract:
No longer merely a concept for the future, the use of digital technologies in dentistry has become common practice today. Computed tomography (CT)-guided dental implant surgery has greatly expanded over the past decade as concepts and techniques have become increasingly refined and more implant manufacturers have adapted their implant systems to these new technologies. The All-on-4® technique for dental implant placement and restoration, while developed some two decades ago, has recently generated increased interest as a highly functional, esthetic, cost-effective alternative for a large group of patients who could benefit from a full-arch, implant-supported fixed restoration. The authors ask, “Are these two technologies a marriage made in heaven?” This article describes the All-on-4 CT-guided surgery technique and reports on the treatment findings on three patients, each with different prosthodontic management.
Implant placement using “guided” technologies has been shown to have greater accuracy and precision when compared to freehand techniques.1-7 This can reduce the incidence of untoward involvement with vital anatomic structures and minimize patient morbidity.8-16 Using proprietary implant-planning software, implants can be “virtually” placed at known pre-planned depths and angulations in three dimensions. Surgical guides are then fabricated from the virtual treatment plan for highly accurate implant placement into the planned implant positions.
This use of virtual, guided technologies contrasts with the practice commonly employed for the placement of dental implants using the conventional All-on-4® (Nobel Biocare, www.nobelbiocare.com) protocol, a concept that has gained acceptance for complete arch restoration. Traditionally, after a clinical evaluation, the All-on-4 surgical workflow first involves a standard panoramic and/or a computed tomography (CT)/cone beam CT (CBCT) evaluation of the patient’s anatomy with routine pre-treatment planning. This leads to surgery involving a full-arch incision with full-arch flap elevation. If necessary, alveolar crest leveling is performed. A paralleling guide is used to verify implant angulation. Osteotomies and implant placement are done freehand. Implants are commonly placed at 30-degree angles (M-4 maxilla and V-4 mandible), and angled abutments are then placed as needed. The implants are usually immediately loaded by retrofitting an existing or new denture prosthesis or by placing a fixed provisional restoration based on an abutment-level impression taken at the time of surgery. The provisional restoration is screw retained.
The use of computer-aided design/computer-aided manufacturing (CAD/CAM) and digital technologies in oral and maxillofacial surgery and dentistry is no longer a futuristic concept. These technologies are being commonly used in dental practice today.17,18 Over the past decade the use of CT-guided dental implant surgery has increased significantly as concepts and techniques have become more refined and many implant manufacturers have adapted their implant systems to these new technologies. The All-on-4 concept for dental implant placement and restoration has been discussed for many years. Recently, the technique has generated increased interest as a highly functional, esthetic, more cost-effective alternative for a larger group of patients who could benefit from a full-arch, implant-supported fixed restoration.
The purpose of this article is to describe the All-on-4 CT-guided surgery technique and report on the findings of three patients treated. Each of the cases had different prosthodontic management.
Technique
CT-guided implant planning and surgery is a restoratively driven treatment plan. It first involves planning an ideal dental restoration for a patient; this may be a complete denture or, for a partially edentulous patient, a diagnostic wax-up of the planned restorations. In the typical guided surgery workflow, the patient then wears an acrylic resin appliance (“scan prosthesis”), which incorporates the ideal anatomy and position of the planned restoration(s), while having a CT/CBCT scan taken of his or her jaw. Various types of fiducial markers are embedded in the scan prosthesis.
The digital imaging and communication in medicine (DICOM) images generated from the scans are then imported into third-party proprietary softwares. The softwares use the fiducial marker points to align the data generated from the scan(s), creating computer images that accurately relate the planned restoration(s) to the patient’s underlying bony anatomy. Implant positions and angulations can then be precisely planned in a virtual environment.
This virtual treatment plan is then sent to a manufacturer or laboratory for fabrication of an appliance that is used at the time of surgery to accurately place the implants in their planned position(s). Most larger implant manufacturers offer guided surgery-specific instrumentation for flapless implant placement. When desired and indicated, techniques and armamentarium are available for extractions, bone reduction, immediate implant placement, and immediate loading, all of which are commonly used in the All-on-4 protocol.
Patient 1
A 50-year-old fully edentulous man presented desiring a full-arch, fixed maxillary restoration. He had been wearing a maxillary denture for 6 years after prematurely losing his teeth from decay and periodontal disease. The denture had never been relined. His past medical history was noncontributory. Finances were a problem for the patient.
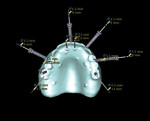
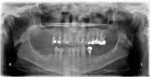
An initial clinical examination that included conventional dental and panoramic radiographs was performed (Figure 1). After an extensive discussion of the surgical and prosthodontic options, an All-on-4/6 option with a retrofit of his existing maxillary denture as an immediate hybrid provisional restoration was planned. First, a hard denture reline was performed on his existing maxillary denture for ideal denture adaptation to the mucosa. An occlusal registration between the denture and opposing arch was fabricated. Gutta percha points were added to the maxillary denture as fiducial markers (Figure 2). As per the double-scan protocol, two appropriate scans were then taken—one of the patient with the denture and occlusal registration in place and a second one of just the denture. The DICOM sets were then imported into the NobelClinician® (NobelBiocare) planning software. Because of the atrophy of the maxillary ridge in width, placement of six implants was planned virtually. One 30-degree, regular-diameter angled implant was treatment-planned posteriorly on each side; four narrow-platform, vertically positioned implants were planned in the anterior areas (Figure 3 and Figure 4). Once completed, the plan was digitally sent to the manufacturer for fabrication of a stereolithographic surgical guide (Figure 5).
At surgery, the surgical guide was properly positioned using an occlusal registration between the guide and the opposing arch. The appliance was stabilized using stabilization pins. Implant-specific instrumentation was used to place the six planned implants to full depth and accurate direction using guided-surgery techniques with implant mounts (Figure 6). Thirty-degree stock abutments were placed on the two posterior implants, and 0-degree stock abutments were placed on three of the four anterior implants. A healing abutment was placed on one implant because of suboptimal initial stability (Figure 7). Temporary titanium sleeves were then placed on the remaining five abutments, two at a time. The denture was modified by creating access openings for the titanium sleeves (Figure 8). Light-activated acrylic resin was used to attach the titanium sleeves to the modified denture. Once trimmed and adjusted, the denture was secured using prosthetic screws (Figure 9). It should be noted that one vertical implant—not the one with suboptimal initial stability—failed during the provisionalization period and was removed and not replaced. The implant that was not initially loaded went on to osseointegrate and was successfully used in the final restoration.
Patient 2
A 65-year-old woman presented with multiple missing and nonrestorable mandibular teeth. She refused to wear a full mandibular denture and wanted a fixed restoration. Her medical history was noncontributory. Finances were an issue for her.
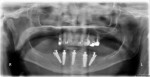
Standard dental records and radiographs (Figure 10) were taken as if the patient were to receive an immediate mandibular denture after extractions. A finished complete mandibular denture was fabricated by the dental laboratory for later modification as a provisional fixed restoration. A multiple-piece scanning prosthesis with gutta percha fiducial markers and an occlusal registration was fabricated by the dental laboratory according to the manufacturer’s guided-surgery protocol (Figure 11). CBCT scans (iCat®, Imaging Sciences International, LLC, www.i-cat.com) using the double-scan technique were taken with the patient wearing this appliance and occlusal registration. The CBCT data was converted into DICOM images and imported into the NobelClinician software for guided-surgery treatment planning. One 30-degree angled implant was treatment-planned posteriorly on each side. Three vertical implants were planned anteriorly, two in planned extraction sockets (Figure 12 and Figure 13). The completed plan was digitally sent to the manufacturer for surgical guide fabrication.
Under intravenous sedation and local anesthesia, the remaining mandibular teeth were extracted with minimal trauma (Figure 14). A bite registration was used to correctly position the surgical guide. Stabilization pins were then placed to secure the surgical guide. Implant-specific instrumentation was used to prepare the appropriate osteotomies and place five implants, fully guided, using implant mounts through the surgical guide to the planned depth and angulation (Figure 15). Thirty-degree stock abutments were placed on the two posterior implants, and 0-degree stock abutments were placed on the three anterior implants (Figure 16). At the time of surgery, open-tray impression copings were placed on the abutments, and an abutment-level impression was made of the postsurgical implant positions (Figure 17). Closed-tray impression copings were used to make an occlusal registration between the arches. The above impression and occlusal registration, along with the immediate mandibular denture and prior-fabricated mounted casts, were sent to the dental laboratory for overnight retrofitting of the mandibular denture. The following morning, the retrofitted acrylic provisional restoration was returned and secured on the implants in the patient’s mandibular arch by prosthetic screw retention (Figure 18 and Figure 19). A minimal occlusal adjustment was necessary. The patient was discharged with explicit dietary instructions regarding extractions and immediate loading of dental implants.
Patient 3
A 62-year-old woman presented with a nonrestorable maxillary dentition, which was indicated for full-mouth extraction. She wanted a full-mouth, implant-supported fixed restoration with an immediate provisional restoration. Her past medical history was negative. Finances were a concern for her.
The patient was evaluated and worked-up clinically and radiographically (Figure 20). Maxillary and mandibular diagnostic casts were made and mounted on an articulator. An ideal diagnostic wax-up of the planned maxillary dentition was created and converted into a multiple-piece hard acrylic scanning appliance. Gutta percha points were added as fiducial markers (Figure 21). CBCT scans were taken using the double-scan technique. The DICOM images were then imported into the NobelClinician software. Six implants were treatment-planned (Figure 22 and Figure 23). The plan was sent to the manufacturer via the Internet for fabrication of a stereolithographic surgical guide based on the virtual treatment plan (Figure 24). One 30-degree angled implant was treatment-planned posteriorly on each side; four vertical implants were planned anteriorly. Four of the six implants were placed through extraction sockets. Once received, the surgical guide was sent to the dental laboratory for fabrication of a full-arch provisional restoration prior to surgery. The provisional restoration was fabricated by creating a master cast using manufacturer componentry developed specifically for this application (Figure 25 and Figure 26). The master cast and an opposing arch diagnostic cast were mounted on an articulator. Using digital prosthodontic planning software and CAM milling technologies, the provisional fixed restoration was milled in one unit (Figure 27 and Figure 28).
Under intravenous sedation, the remaining maxillary teeth were removed. The surgical guide was accurately placed using a bite registration and secured with guided-surgery pins (Figure 29). Using implant-specific guided-surgery instrumentation, the six implants were placed to the planned depth and angulation. All implants were placed fully guided with implant mounts, as per guided-surgery protocols (Figure 30). Thirty-degree stock abutments were placed on the two posterior implants, and 0-degree stock abutments were placed on the four anterior implants. Titanium sleeves were placed on the abutments, and light-cured acrylic was used to accurately secure them to the presurgically fabricated provisional prosthesis. The provisional prosthesis was then secured into place using prosthetic screws (Figure 31 and Figure 32). A slight occlusal adjustment was necessary. The patient was discharged with explicit dietary and functional instructions.
Discussion
There is no CT-guided drill-guide technology with absolute precision. Stereolithographic guide deviations between virtual planning and obtained implant positions have been shown in all dimensions.19 The highest mean deviations are found in implants placed by bone-supported guides, while implants placed by mucosa-supported guides measure lower deviations.20 Tooth-supported drill guides measure the lowest deviations.21 Deviations are further minimized by using rigid-screw or pin fixation of a single guide, metal guide sleeves, drilling instrumentation specific to the implant to be placed, and instrumentation (implant-specific implant mounts) for the fully guided placement of implants through the surgical guide. Most systems use screws or pins to stabilize mucosal-supported guides; some systems recommend them to stabilize all guides.
Minimally invasive procedures maximize patient comfort by minimizing trauma to the tissues. Flapless dental implant insertion minimizes potential soft-tissue elevation complications such as infection, dehiscence, and soft- and hard-tissue necrosis and has been shown to have dental implant success rates equal to conventional techniques.15,22-24 A flapless technique using surgical guidance for optimal control of drill depth and angulation minimizes potential injury to underlying anatomical structures during implant osteotomies.
Maló popularized the All-on-4 concept initially reported by Mathews.25 The concept involves the placement of four dental implants in each arch. Two implants are typically placed in the maxillary or mandibular anterior lateral incisor/canine region in a conventional vertical fashion. Two additional anterior-posterior angled implants are placed in the posterior regions, usually in the premolar regions, at a 30-degree angulation. The posterior angled implants are placed in order to avoid the maxillary sinuses and the mental foramina, while enlarging the anterior-posterior spread of the implant platforms in order to maximize the number of teeth fabricated in the final restoration. These techniques minimized the need for preparatory bone-grafting procedures and lessened the number of implants needed for a complete-arch restoration. Manufacturers began creating stock 30-degree angled abutments specifically for this technique. The final restoration is commonly a complete-arch, which is usually limited to the second premolar or first molar teeth. As the All-on-4 concept has gained acceptance, new modifications to the technique have been developed and presented in order to alleviate the problems of severe atrophy with limited bone stock or limited interocclusal space for restorations.26-31
Intentional angled implant placement is not a new surgical technique, as for many years implant manufacturers have created stock angled abutments for intentional or unintentional angled implant placement. Dental laboratories have been fabricating customized abutments using traditional lab techniques almost as long as titanium root form implants have been in existence. CAD/CAM technologies are now commonly used to fabricate customized abutments in a digital environment to solve implant placement and esthetic problems.
Successful immediate and early loading of implants using the latest generation of implants has been described in the literature.32-34 Rigid cross-arch stabilization successfully permits the immediate loading of titanium implants in an edentulous ridge, allowing rapid rehabilitation of the arch, with 6- to 24-month implant survival rates of 91% to 96.9%,35-37 but it is dependent on proper patient selection. New implant designs and surface technologies allow immediate placement of an implant-supported restoration following surgery as a predictable treatment option for single-tooth implants and multiple-unit fixed prostheses.38-41 Immediate loading of dental implants has a positive effect on the tissue differentiation and bone formation around titanium implants.42
Implant placement followed by immediate loading is also not new. Ledermann, Schnitman, and Tarnow were among the first to introduce this technique.38,43-45 Wolfinger presented a change in concept by placing fewer implants but loading all the implants at the same time.46 Prior to this, immediate-loading concepts involved loading a select few implants among a larger number of dental implants in edentulous mandibles. Long-term survival rates of 96.6% to 99.4% for screw-type dental implants in edentulous mandibles using both concepts have been reported.38,46-50 While Tarnow et al stated that immediate loading must include at least five dental implants in edentulous mandibles,38 other authors have shown that fewer implants can be used for immediate loading.25,41,46,51-52 This is comparable to other reports of immediate loading on dental implants, such as the 98.2% cumulative survival rate after 6 months reported by Maló,25 the cumulative survival rate of 96% (mean follow-up, 36 months) presented by Valente,53 and a systematic review of the Cochrane database regarding different times for loading of implants presented in 2009, in which there were no statistically significant differences in the meta-analyses for the loading of osseointegrated implants in any treatment timeframe, ie, immediate (within 1 week), early (between 1 week and 2 months), and conventional (after 2 months).54
Although the success rates of immediately loaded implants in the edentulous jaw is comparable to a staged healing protocol, screw loosening, prosthesis breakage, overloading, and/or parafunction can all lead to implant micromovement, resulting in potential failure.55 Hence, proper case selection and patient awareness, education, and compliance are all critical factors for success.
Conclusion
The use of CT-guided surgery to perform the All-on-4 procedure is a combination of technologies that is in the early stages of common practice. However, early experience suggests a successful “marriage” of these two techniques, with the possibility of improved patient outcomes. Future research is required to fully examine the limitations of both technologies in the myriad situations found in the terminal dentition or atrophic jaw.
ABOUT THE AUTHORS
Gary Orentlicher, DMD
Chief, Division of Oral and Maxillofacial Surgery, White Plains Hospital Medical Center, White Plains, New York; Private Practice, New York Oral, Maxillofacial, and Implant Surgery, Scarsdale, New York
Ole Jensen DDS, MS
Director, Colorado Tissue Engineering Institute, Denver, Colorado; Private Practice, Greenwood Village, Colorado
Andrew Horowitz, DMD, MD
Private Practice, New York Oral, Maxillofacial, and Implant Surgery,
Scarsdale, New York
Mark Adams, DDS, MS
Private Practice, Prosthodontics, Greenwood Village, Colorado
Marcus Abboud, DMD
Chairman, Department of Prosthodontics and Digital Technologies,
Stony Brook University School of Dental Medicine, Stony Brook, New York
ACKNOWLEDGMENTS
The authors would like to acknowledge the contributions of: Mark Briskin, DDS, Ardsley, New York, on Patient 1; Raymond Weiss, DMD, Scarsdale, New York, and Marotta Dental Laboratory, Farmingdale, New York, on Patient 2; and Matthew Teich, DDS, White Plains, New York, and Laboratory-Björn Zappa, Oldenburg, Germany, on Patient 3.
REFERENCES
1. van Steenberghe D, Glauser R, Blombäck U, et al. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: a prospective multicenter study. Clin Implant Dent Relat Res. 2005;7(suppl 1):S111-S120.
2. Tardieu P, Vrielinck L. Implantologie assistèe par ordinateur: le propramme SimPlant/SurgiCase™ et le SAFE System™ mis en charge immediate d’unbridge mandibulaire avec des impalt transmuqueux. Implant. 2003;9:15-28.
3. Rosenfeld AL, Mandelaris GA, Tardieu PB. Prosthetically directed implant placement using computer software to ensure precise placement and predictable prosthetic outcomes. Part 3: stereolithographic drilling guides that do not require bone exposure and the immediate delivery of teeth. Int J Periodontics Restorative Dent. 2006;26(5):493-499.
4. Vrielinck L, Politis C, Schepers S, et al. Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe bone atrophy using customized drill guides. Preliminary results from a prospective clinical follow-up study. Int. J Oral Maxillofac Surg. 2003;32(1):7-14.
5. Sarment DP, Sukovic P, Clinthorne N. Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants. 2003;18(4):571-577.
6. Soares MM, Harari ND, Cardoso ES, et al. An in vitro model to evaluate the accuracy of guided surgery systems. Int J Oral Maxillofac Implants. 2012;27(4):824-831.
7. Van Assche N, van Steenberghe D, Guerrero ME, et al. Accuracy of implant placement based on pre-surgical planning of three-dimensional cone-beam images: a pilot study. J Clin Periodontol. 2007;34(9):816-821.
8. Ramez J, Donazzan M, Chanavaz M, et al. [The contribution of scanner imagery in implant surgery and sinus overflow using frontal oblique orthogonal reconstruction.] Rev Stomatol Chir Maxillofac. 1992;93(3):212-214.
9. Pattijn V, van Cleynenbreugel T, vander Sloten J, et al. Structural and radiological parameters for the nondestructive characterization of trabecular bone. Ann Biomed Eng. 2001;29(12):1064-1073.
10. Sonick M, Abrahams J, Faiella R. A comparison of the accuracy of periapical, panoramic, and computerized tomographic radiographs in locating the mandibular canal. Int J Oral Maxillofac Implants. 1994;9(4);455-460.
11. Todd A, Gher M, Quintero G, Richardson AC. Interpretation of linear and computed tomograms in the assessment of implant recipient sites. J Periodontol. 1993;64(12):1243-1249.
12. Gher ME, Richardson AC. The accuracy of dental radiographic techniques used for evaluation of implant fixture placement. Int J Periodontics Restorative Dent. 1995;15(3):268-283.
13. Hahn J. Single-stage, immediate loading, and flapless surgery. J Oral Implantol. 2000;26(3):193-198.
14. Campelo LD, Camara JR. Flapless implant surgery: a 10-year clinical retrospective analysis. J Oral Maxillofac Implants. 2002;17(2):271-276.
15. Becker W, Goldstein M, Becker BE, Sennerby L. Minimally invasive flapless implant surgery: a prospective multicenter study. Clin Implant Dent Relat Res. 2005;7(suppl 1):S21-S27.
16. Becker W, Wikesjö UM, Sennerby L, et al. Histologic evaluation of implants following flapless and flapped surgery: a study in canines. J Periodontol. 2006;77(10):1717-1722.
17. Orentlicher G, Goldsmith D, Horowitz A. Applications of 3-dimensional virtual computerized tomography technology in oral and maxillofacial surgery: current therapy. J Oral Maxillofac Surg. 2010;68(8):1933-1959.
18. Orentlicher G. Digital Technologies in Oral and Maxillofacial Surgery, An Issue of Atlas of Oral and Maxillofacial Surgery Clinics. Vol 20. No. 1. Philadelphia, PA: Elsevier; 2012.
19. D’haese J, Van De Velde T, Komiyama A, et al. Accuracy and complications using computer-designed streolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clin Implant Dent Relat Res. 2012;14(3):321-335.
20. Arisan V, Karabuda ZC, Ozdemir T. Accuracy of two stereolithographic guide systems for computer-aided implant placement: a computed tomography-based clinical comparative study. J Periodontol. 2010;81(1):43-51.
21. Ozan O, Turkyilmaz I, Ersoy AE, et al. Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg. 2009;67(2):394-401.
22. Arisan V, Karabuda CZ, Ozdemir T. Implant surgery using bone- and mucosa-supported stereolithographic guides in totally edentulous jaws: surgical and post-operative outcomes of computer-aided vs. standard techniques. Clin Oral Implants Res. 2010;21(9):980-988.
23. Cannizzaro G, Torchio C, Leone M, Esposito M. Immediate versus early loading of flapless-placed implants supporting maxillary full-arch prostheses: a randomised controlled clinical trial. Eur J Oral Implantol. 2008;1(2):127-139.
24. Abboud M, Wahl G, Guirado JL, Orentlicher G. Application and success of two stereolithographic surgical guide systems for implant placement with immediate loading. Int J Oral Maxillofac Implants. 2012;27(3):634-643.
25. Maló P, Rangert B, Nobre M. All-on-Four immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(suppl 1):2-9.
26. Jensen OT, Adams MW. All-on-4 treatment of highly atrophic mandible with mandibular V-4: report of 2 cases. J Oral Maxillofac Surg. 2009;67(7):1503-1509.
27. Jensen OT, Adams MW. The maxillary M-4: A technical and biomechanical note for all-on-4 management of severe maxillary atrophy—report of 3 cases. J Oral Maxillofac Surg. 2009;67(8):1739-1744.
28. Jensen OT, Adams MW, Cottam JR, et al. The All-on-4 shelf: maxilla. J Oral Maxillofac Surg. 2010;68(10):2520-2527.
29. Jensen OT, Adams MW, Cottam JR, et al. The All-on-4 shelf: mandible. J Oral Maxillofac Surg. 2011;69(1):175-181.
30. Jensen O, Cottam J, Adams M, Adams S. Buccal to lingual transalveolar implant placement for all-on-four immediate function in posterior mandible: report of 10 cases. J Oral Maxillofac Surg. 2011;69(7):1919-1922.
31. Jensen OT, Cottam J, Ringeman J, Adams M. Trans-sinus dental implants, bone morphogenetic protein 2, and immediate function for all-on-4 treatment of severe maxillary atrophy. J Oral Maxillofac Surg. 2012;70(1):141-148.
32. Gapski R, Wang HL, Mascarenhas P, Lang NP. Critical review of immediate implant loading. Clin Oral Implants Res. 2003;14(5):515-527.
33. Ogawa T, Nishimura I. Different bone integration profiles of turned and acid-etched implants associated with modulated expression of extracellular matrix genes. Int J Oral Maxillofac Implants. 2003;18(2):200-210.
34. Zechner W, Tangl S, Fürst G, et al. Osseous healing characteristics of three different implant types. Clin Oral Implants Res. 2003;14(2):150-157.
35. Lorenzoni M, Pertl C, Zhang K, Wegscheider WA. In-patient comparison of immediately loaded and non-loaded implants within 6 months. Clin Oral Implants Res. 2003;14(3):273-279.
36. Jaffin RA, Kumar A, Berman CL. Immediate loading of dental implants in the completely edentulous maxilla: a clinical report. Int J Oral Maxillofac Implants. 2004;19(5):721-730.
37. Gatti C, Haefliger W, Chiapasco M. Implant-retained mandibular overdentures with immediate loading: a prospective study of ITI implants. Int J Oral Maxillofac Implants. 2000;15(3):383-388.
38. Tarnow DP, Emtiaz S, Classi A. Immediate loading of threaded implants at stage 1 surgery in edentulous arches: ten consecutive case reports with 1- to 5-year data. Int J Oral Maxillofac Implants. 1997;12(3):319-324.
39. Chatzistavrou M, Felton DA, Cooper LF. Immediate loading of dental implants in partially edentulous patients: a clinical report. J Prosthodont. 2003;12(1):26-29.
40. Glauser R, Lundgren AK, Gottlow J, et al. Immediate occlusal loading of Brånemark TiUnite implants placed predominantly in soft bone: 1-year results of a prospective clinical study. Clin Implant Dent Relat Res. 2003;5 suppl 1:47-56.
41. Abboud M, Koeck B, Stark H, et al. Immediate loading of single-tooth implants in the posterior region. Int J Oral Maxillofac Implants. 2005;20(1):61-68.
42. Vandamme K, Naert I, Geris L, et al. Histodynamics of bone tissue formation around immediately loaded cylindrical implants in the rabbit. Clin Oral Implants Res. 2007;18(4):471-480.
43. Ledermann D. [6-year clinical trial with titanium plasma-coated ITI (Internationales Team fur Implantologie) screw implants in the mandibular interforaminal region]. SSO Schweiz Monatsschr Zahnheilkd. 1983;93(11):1070-1089.
44. Ledermann P. [Bar-prosthetic management of the edentulous mandible by means of plasma-coated implantation with titanium screws]. Dtsch Zahnarztl Z. 1979;34(12):907-911.
45. Schnitman PA, Wöhrle PS, Rubenstein JE, et al. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants. 1997;12(4):495-503.
46. Wolfinger GJ, Balshi TJ, Rangert B. Immediate functional loading of Brånemark system implants in edentulous mandibles: clinical report of the results of developmental and simplified protocols. Int J Oral Maxillofac Implants. 2003;18(2):250-257.
47. Horiuchi K, Uchida H, Yamamoto K, Sugimura M. Immediate loading of Brånemark system implants following placement in edentulous patients: a clinical report. Int J Oral Maxillofac Implants. 2000;15(6):824-830.
48. Ganeles J, Rosenberg MM, Holt RL, Reichman LH. Immediate loading of implants with fixed restorations in the completely edentulous mandible: report of 27 patients from a private practice. Int J Oral Maxillofac Implants. 2001;16(3):418-426.
49. Aalam AA, Nowzari H, Krivitsky A. Functional restoration of implants on the day of surgical placement in the fully edentulous mandible: a case series. Clin Implant Dent Relat Res. 2005;7(1):10-16.
50. Degidi M, Piattelli A, Felice P, Carinci F. Immediate functional loading of edentulous maxilla: a 5-year retrospective study of 388 titanium implants. J Periodontol. 2005;76(6):1016-1024.
51. Brånemark PI, Engstrand P, Ohrnell LO, et al. Brånemark Novum: a new treatment concept for rehabilitation of the edentulous mandible. Preliminary results from a prospective clinical follow-up study. Clin Implant Dent Relat Res. 1999;1(1):2-16.
52. De Bruyn H, Kisch J, Collaert B, et al. Fixed mandibular restorations on three early-loaded regular platform Brånemark implants. Clin Implant Dent Relat Res. 2001;3(4):176-184.
53. Valente F, Schiroli G, Sbrenna A. Accuracy of computer-aided oral implant surgery: a clinical and radiographic study. Int J Oral Maxillofac Implants. 2009;24(2):234-242.
54. Esposito M, Grusovin MG, Achille H, et al. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2009;1:CD003878.
55. Misch CM. Immediate loading of definitive implants in the edentulous mandible using a fixed provisional prosthesis: The denture conversion technique. J Oral Maxillofac Surg. 2004;62(9 suppl 2):106-115.