The Clinical Significance of Mechanical Properties in Retentive Posts
Abstract:
When a clinician is faced with the selection of dental materials for use in the permanent restoration of severely broken down teeth, esthetics are—and should be—secondary to the mechanical and physical properties necessary for that particular application. Most dentists over age 50 practicing in the United States today were trained using cast post and cores, amalgam, gold alloy, chromium cobalt, stainless-steel crowns, reversible hydrocolloid or polysulfide rubber impression materials, silicate cements and early developments of ceramics. The majority of practicing dentists must rely on postgraduate continuing education courses to stay abreast of the many new developments in dental materials. Many technologies being used in restorative dentistry today are borrowed from other industries and disciplines and are adapted to best suit a dental application—a sort of “technology transfer.” These include silicones, lasers, visible light-emitting diode (LED) curing lights, digital recordkeeping, fiber optics, and fiber-reinforced composites.
Fiber-reinforced composite (FRC) endodontic posts (ie, fiber posts) were developed and introduced in Europe in 1990.1 They were approved by the Food and Drug Administration (510k) and introduced to the US market in the mid-1990s (Composipost™, RTD [Recherches Techniques Dentaires]; imported as C-Post™, Bisco Inc.), and in Canada before that. The first generation of posts, made of carbon fibers, were black in color, radiolucent, and obviously very unesthetic. The inventors’ priorities were the critical aspects of clinical performance and optimal interaction of the product with the tooth structure. They were aiming for a material from which an “anatomic” retentive post could be fabricated that would not compromise the remaining root structure, as did metal posts that were commonly used at that time. Today, nearly all fiber posts are tooth colored and esthetic.
Selection of a dental material is based on the physical properties required and the unique functional demands placed upon it in a specific clinical application. For instance, in evaluating an industrial material for use in a fiber post, a clinician would not be that interested in characteristics such as abrasion resistance, solubility, or even compressive strength, but would be highly interested in these characteristics if evaluating a composite filling material. The primary function of an endodontic post is to retain the core, and by extension, the crown. The post selected should provide retention, conservation of tooth structure, durability under function, and root protection. The latter two factors are primarily post-related and will be the focus of this article.
The purpose of this article is to review how fiber posts differ from their metal predecessors, how they vary intrinsically from one design or brand and composition to another, and finally, how these posts actually function and interact with the tooth. The authors feel this review is timely, since the trend away from metal posts towards fiber posts is accelerating,2 and an increasing number of brands and designs have become available. In addition, increasingly more in-vitro studies are being published, some of which are good, some flawed, and some even misleading.
There have been very few clinical studies of fiber post products that extend beyond 5 years duration and that have been published in peer-reviewed journals.3-5 Products that have been studied include the carbon fiber and quartz fiber posts; these have been tested the most and have become the standard against which other products are often compared. Many fiber posts are introduced to the market with little or no evidence of clinical performance. However, a number of laboratory evaluations can be conducted that have clinical relevance, and some conclusions may be drawn by a careful analysis of in-vitro published data. The authors propose the following as critical mechanical properties for endodontic posts:
• elastic modulus (Young’s modulus of elasticity)
• flexural strength
• resistance to cyclic fatigue
• absence of galvanism and corrosion
Mechanical Properties
Elastic Modulus
Modulus of elasticity, a term used to describe a material’s stiffness, is an inherent physical property of a material regardless of size,6 and, like any other modulus, it is a ratio. In this case it is a calculation of stress over strain according to Hooke’s law (published in 1678). When combined with flexural strength it provides a description of how a material behaves in the elastic range when it is placed under a functional load.
There are significant differences between metal posts, which are isotropic, and fiber-reinforced composite posts, which are anisotropic. Metal posts have the same elastic modulus regardless of the angle of load application from which it is calculated.7 Fiber posts, being anisotropic, have an elastic modulus that varies considerably from the 12 o’clock to the 3 o’clock position. The inventors of the fiber post (Duret and Reynaud) calculated the modulus at 30 degrees, which they based on the angle of incidence that most closely approximates function in the mouth during mastication and lateral excursions. Many in-vitro studies have followed this thinking. The elastic modulus of human dentin is reported in dental textbooks as 18.6 Gigapascals (GPa). Stainless-steel posts (regardless of diameter) have an elastic modulus of roughly 200 GPa, while titanium alloy posts are 110 GPa. The elastic modulus of fiber-reinforced posts, as reported by various manufacturers, varies from 6 GPa to 60 GPa. This large variation illustrates the dependence of this property on the type of fiber being used and its density within the matrix. For example, carbon fibers have a higher modulus than S-glass fibers or E-glass fibers8 (Table 1).
The easiest way to demonstrate and differentiate the interaction of the modulus of one material with another is through finite element analysis (FEA). FEA is a computer modeling technique that can determine the effect of an applied force on the stress resulting at any point within a multicomponent structure. A number of researchers have used FEA to examine the difference in the transmission of stress to different parts of the tooth as it relates to the one variable element—the endodontic post9—with all other factors remaining equal (tooth size, remaining dentin/ferrule, cement and cementation method, etc). It is clear from this research that a better match of modulus of elasticity between the post and root dentin is responsible for a considerable reduction in stress transfer in a severely compromised tooth.10-13 It can best be described as the post moving “with” the tooth rather than “against” it.
Flexural Strength
It is easy for the practitioner or student to confuse elastic modulus with flexural strength, since both imply a real or theoretical bending of a rod, or dowel. Flexural strength contrasts with elastic modulus in that it is significantly influenced by the diameter of the sample. It is an excellent screening test for fiber posts and clearly distinguishes some posts from others, even when the data is normalized to account for slight differences in diameter.
However, while it may seem straightforward enough to load a fiber post onto an Instron® machine and break it, the data generated is often unreliable and sometimes misleading.14-17 The reason is as follows: fiber posts vary in length from 15 mm to 22 mm. The jig used in the Instron machine has two resting points 10 mm to 13 mm apart, at a minimum (Figure 1). Mounting a post and applying downward pressure on a specimen only 13 mm long (the span) becomes a test of compression rather than of flexure. In fact, this type of flexural testing is actually a test of tensile strength of the fibers on the bottom side of the specimen, while the top surface undergoes compression. Therefore, incorporating fibers that have a high tensile strength contributes to a better result for fiber posts tested in this manner. The results are also influenced by the shape and design of the post (tapered vs. parallel, smooth vs. macro-retentive). Most published flexural strength tests of fiber posts utilize the post itself rather than standardized samples of the material from which it is made. This frequently leads to invalid comparisons—clearly, the strength of a tapered post will depend on where along its length the load is applied.
Well-defined testing methodologies such as those published by the International Standards Organization (ISO) are widely used in industry. ISO Standard No. 14125 for flexural strength testing of composites requires the application of a force to the midpoint of a specimen of consistent diameter that has a length 20 times its diameter (Figure 2). Tests conducted according to this standard generate reliable and reproducible results compared with the significant variations reported in the literature on the flexural strength of fiber composite posts. However, this test essentially requires the use of the raw material from which the post is made. These materials are not currently readily accessed by independent researchers, but a limited number of manufacturers have made their materials available. In a study conducted utilizing the ISO standard, Stewardson concluded: “The flexural strengths of FRC endodontic post materials in general exceed the yield strength of metals from which endodontic posts are made. The high Weibull modulus values suggest good clinical reliability of FRC posts. The flexural modulus values of the tested posts were from 2 to 6 times (FRC) to 4 to 10 times (metal) that of dentin. Valid measurement of flexural properties of endodontic post materials requires that test samples have appropriate length/diameter ratios.”
Clinicians should demand accurate data from manufacturers that will enable them to make an informed decision about which post to use. Increasingly, ISO-certified manufacturers are reporting the flexural strength of their fiber posts, determined with the standardized method described above, in their literature, website, or brochures.
Major differences in mechanical behaviors exist among the various types of posts due to the materials used. Clinicians should be informed about the most favorable characteristics of certain compositions. With respect to flexural strength and fatigue resistance, differences in mechanical behaviors can be based on certain material factors or combination of factors, including:
• the type and quality of fiber used (glass, carbon, quartz, etc)
• the density of fibers used (the ratio of fiber to matrix)
• the interlaminate shear strength (the quality of the bond between the fibers and matrix, which often necessitates an additional step in manufacturing such as silane treatment of the fibers)
• the quality of the manufacturing process (absence of internal voids and spaces that create weak points)
• the inclusion of other filler particles (often as a low-cost means of increasing radiopacity)
• the choice of resin matrix
As a cost-cutting measure that can lead to a less expensive product for the end-user, some posts are made from fibers (eg, E-glass) that were developed for telecommunications and other industries. In such industries, S-glass or R-glass are considered expensive raw materials compared to standard E-glass and are typically priced about five times higher than E-glass. Quartz fibers are the most expensive, and are approximately 25 times the cost of E-glass. Additionally, less proven fibers (eg, zirconia-enriched glass fibers) might be used that will enhance radiopacity without the need for additional fillers.
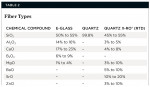
Some manufacturers have invested in the development of unique fibers to maximize and optimize strength, fatigue resistance, elastic modulus, radiopacity, light transmission, and the bonding of the fibers to the matrix resin. These fibers (Table 2) can include a very high percentage of silica, which drives up the price of the raw materials and end product, but also eliminates elements that can contribute to their susceptibility to the damaging effects of moisture. Still, these higher-end posts can be purchased on the North American market for less than $12 per post.
Cyclic Fatigue Resistance
Flexural strength testing is an excellent technique for determining the best type and combination of materials for fiber posts, and for evaluating the quality of manufacturing. However, fatigue loading is the most realistic in-vitro test that can be applied to materials, as it most closely simulates and predicts what may happen in vivo.18,19 Fatigue loading is the repetitive application of a force less than that required for fracture of the post, and is conducted over many cycles. It is more difficult and time-consuming to conduct than flexural strength testing, but more accurately reflects the conditions in the mouth. Grandini noted that more restorations fail clinically as a result of low energy abuse over a long period of time than from a single destructive event.19 Therefore, the previously mentioned inventors needed to know how fiber-reinforced posts would hold up under cyclic fatigue compared to metal posts, which were used at that time. The original test method called for the flexural strength to be determined before cyclic fatigue loading and again afterwards. The results were dramatic: the flexural strength of the metal post diminished by 40% following fatigue loading, while the fiber composite posts decreased by only 14%.20 Wiscott et al,21 used a different (“rotational”) fatigue test methodology in 2008 and concluded that the fiber posts were more fatigue-resistant than metal posts. Furthermore, the quartz fiber post was found to be more than twice as fatigue-resistant as the stainless and titanium alloy posts.
Additional data are available on the fatigue resistance of different brands of fiber posts by themselves without the additional variables introduced by the influence of extracted teeth that support this conclusion.22,23 The fatigue test used for this purpose is typically a three-point bending test, using a load that is 50% of the reported flexural strength of that post at a 90-degree angle of incidence.
With this test, typical survival rates can vary widely from post to post and manufacturer, with D.T. Light Post® (RTD) surviving 2 million cycles with no fractures, EasyPost™ (DENTSPLY) surviving 931,750 cycles to fracture, Luscent™ (Dentatus) 807,243 cycles to fracture, ParaPost® Fiber White (Coltène/Whaledent) 84,916 cycles to fracture, FibreKor® (Pentron) 29,688 cycles to fracture, and Snowpost® (Abrasive Technology) only 6,763 cycles to fracture.19 The test is usually ended after 2 million cycles, which represent 8 years of clinical service.19
To summarize, the mechanical properties and design of fiber composite posts should be optimized so that they will bend slightly under the repetitive functional forces encountered in the mouth, mimicking the same amount of bending occurring within the dentin (equivalent modulus). With fiber posts (particularly those containing quartz fibers), this is accomplished with a low risk of fatigue failure. On the other hand, with metal posts there is a mismatch of modulus with resulting stress concentration within the root and a lack of resistance to cyclic fatigue forces.
There is a growing body of research using the universal testing machine (Instron) to test the interactions, survival rates, and failure modes with different types of prefabricated and custom-made posts in extracted teeth. This has resulted in an evolution over the past 20 years of material and post design and placement and cementation techniques. To summarize the general conclusion of these tests, metal posts tend to demonstrate a higher fracture strength, but the results of the fracture are catastrophic (root fracture), whereas the failure modes with fiber post restorations are generally repairable.24-27 This, in the view of the authors, is the most compelling reason for the supplanting of metal posts by fiber posts.
Corrosive and Galvanic Interaction
For decades, if not centuries, gold was the material of choice for inlays, onlays, and crown and bridge work. One of the reasons gold has worked so well is because the elastic modulus of dental gold alloy better approximates that of enamel and dentin than do other dental materials. Another reason is that gold is basically inert—it does not readily react with the environment to form oxides. In contrast, stainless steel, amalgam, and base-metal (non-noble) casting alloys can corrode when placed in the oral environment due to galvanic action.28 Metallurgists and engineers have been aware of these problems for centuries, but dentists lacked (or overlooked) alternatives.
In a study of teeth with metallic posts, 468 vertical root fractures were observed, of which 72% involved corrosive sequelae.29 Whether corrosion causes a root to fracture or whether non-precious posts corrode after the root has fractured remains an unanswered question. A further concern is the well-known allergic potential related to the nickel present in certain dental alloys. Women are particularly susceptible to this in that they may have been sensitized to the material through contact with jewelry. Given today’s price of gold it is unlikely that gold posts will be affordable for most patients. Fiber composite remains a highly biocompatible, cost-effective choice.
Additional Characteristics
There are additional characteristics that distinguish fiber posts from metal posts as well as one type of fiber post from another. These characteristics, which include radiopacity, light transmission or conductivity, and removability, facilitate diagnosis, contribute to optical benefits, and enhance clinical expediency.
Radiopacity
Radiopacity is important to both clinicians and insurance companies. Distinct contrast of the post with the surrounding tooth structure facilitates diagnosis and clearly reveals the use of a post in the buildup procedure. Yet, hundreds of thousands (if not millions) of fiber-reinforced post-retained restorations are in good clinical service 20 years after placement and with a less than optimal level of radiopacity.3 As with flexural strength and fatigue resistance, more radiopacity is better, providing it does not compromise the mechanical priorities previously discussed. It is difficult for clinicians to measure differences in flexural strength or fatigue resistance, but they can certainly see a difference in the radiopacity of a post, the cement, the core, and the dentin. The differences in radiopacity among various brands of fiber posts have been compared on several occasions.30-32
The radiopacity of various posts is clearly demonstrated in Figure 3 and should be self-explanatory to the practitioner. Non-radiopaque or marginally radiopaque fibers can be enhanced by replacing some of the fibers with radiopaque fillers (Figure 4) such as barium or ytterbium. Unfortunately, this has a negative impact on flexural strength, light transmission, and often the cyclic fatigue resistance of the post.19
Light Transmission
Thus, the challenge is to provide the clinician with a post that has high fatigue resistance, high flexural strength, low elastic modulus, and high radiopacity, while at the same time conducting as much light (polymerization energy) to the most apical sections of the post. The latter property offers the clinical advantage of expediency. Clearly, some fiber posts are more light-conductive than others,33-36 as seen in Figure 5 and Figure 6.
To the best of the authors’ knowledge, no fiber post manufacturer guarantees that its fiber post will allow sufficient light transmission to result in complete curing of bonding agents and resin cements at the most apical portion of the post. The published in-vitro documentation on this topic is still inconclusive, since there is no standard test methodology. It is, therefore, recommended to always use cements that are dual-cured. However, a translucent fiber post with greater light transmission will allow the clinician to seat the post in the resin cement, even if adding accessory posts, and “shoot” enough photons into the interior to immediately stabilize the post so that the core can be applied immediately.
Research37 indicates that the ultimate cross-linking of a cement is higher when utilizing a combination of the light-curing and chemical-curing modalities. The same is true for the placement of the core. While self-etching and self-adhesive systems are proving to be adequate in-vitro,38 higher bond strengths are attained with etch-and-rinse systems.39 In a systematic review of the literature, Dietsche concluded: “to establish the best possible adhesion within the root, only specific combinations of dentin adhesives and luting cements proved efficient; presently etch-and-rinse adhesives with a dual curing resin cement appear to be the best choice.”40
Removability
Clinicians place restorations with the expectation of long-term success. However, a certain percentage of endodontic treatment fails and retreatment is indicated. As many as 25% of these cases may involve the presence of a post. Certainly, the removal of a metal post can be stressful to the patient and clinician, and has risks. In contrast, fiber posts can be removed with a minimal amount of destruction to the remaining tooth structure. Most removal drill systems do not provide a specific removal technique, which leaves clinicians to use their best judgment. It is worth noting that fiber posts must be removed by hollowing them out from the inside, rather than vibrating or pulling them out, as with metal posts. Ample evidence exists that supports this clinical benefit of fiber posts during retreatment.41-44 A novel patented post composition with thermo-dynamic color change capability is available (DT Light-Post® Illusion® X-RO and Macro-Lock™ Post Illusion X-RO, RTD) that helps identify post location and post size, thereby facilitating the removal process.
Post Selection
As has been stated, clearly there are well-defined criteria for mechanical and physical properties as well as manufacturing quality that can aid clinicians in choosing a fiber post. Additional selection criteria include the shape of the post (parallel, tapered, double-tapered) and surface characteristics (smooth, macro-retentive). Each of these additional factors has its proponents, and clinician preference plays an important role in selection.
While post selection is a critical factor in the reconstruction of an endodontically treated tooth, there are others of equal or even greater importance. Clinical studies have provided strong evidence that the amount of remaining tooth structure (ferrule) is the most important prognostic factor for tooth survival.5,45 Another key factor is the proficiency and comfort level of the clinician in using etch-and-rinse procedures and priming systems within the root canal. Interior radicular dentin is different morphologically from “exterior” dentin. It is more difficult to see and access and to clean interior surfaces and prevent moisture contamination. There are now a number of brands of self-adhesive and/or self-etching cements that present data in bonding to dentin, but it should be emphasized that this data is generally to exterior dentin (as in crown and bridge preparations), and not to radicular dentin. Regardless of the location in the mouth, in-vitro studies still show that the etch-and-rinse bonding technique, while perhaps more technique-sensitive and requiring extra steps, provides superior bonding compared to newer systems.
In summary, when choosing materials for their practice, clinicians should rely on long-term documentation that supports the product(s), particularly with respect to mechanical properties and performance. Selecting the best material should be based on knowledge and an understanding of what properties are critical rather than on a recommendation without strong clinical and basic research support. This is especially critical when restoring a compromised tooth that has already been subjected to endodontic treatment and now requires a post, core, and definitive restoration. A solid foundation improves long-term predictability and longevity of the restoration.
ACKNOWLEDGMENT
The authors gratefully acknowledge the contributions of Norman Hicks of Norman Hicks Consulting, Louisville, Kentucky.
DISCLOSURE
Dr. Boksman is a paid part-time consultant to Clinician’s Choice Dental Products, Inc.
ABOUT THE AUTHORS
Leendert Boksman, DDS, BSc
Former Tenured Associate Professor, Restorative Dentistry, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada
Cornelis H. Pameijer, DMD, DSc, PhD
Professor Emeritus, University of Connecticut School of Dental Medicine, Farmington, Connecticut
James C. Broome, DDS, MS
Professor, Department of Restorative Sciences, University of Alabama at Birmingham, School of Dentistry, Birmingham, Alabama
REFERENCES
1. Duret B, Reynaud M, Duret F. Un nouveau concept de reconstitution corono-radiculaire. Le Chir Dent de France. 1990;542:69-77.
2. Christensen GJ. Post concepts are changing. J Am Dent Assoc. 2004;135(9):1308-1310.
3. Ferrari M, Cagidiaco MC, Goracci C, et al. Long-term retrospective study of the clinical performance of fiber posts. Am J Dent. 2007;20(5):287-291.
4. Goracci C, Cagidiaco M, Cagidiaco E, et al. Effects of oral environment and occlusal wear on FRC-posts integrity [abstract]. J Dent Res. 2007;86(spec iss A). Abstract 0131.
5. Ferrari M, Vichi A, Fadda GM, et al. A randomized controlled trial of endodontically treated and restored premolars. J Dent Res. 2012;91(7 suppl):S72-S78.
6. Wagnild G, Mueller K. Restoration of endodontically treated teeth. In: Cohen S, Hargreaves KM, Keiser K, eds. Pathways of the Pulp. 9th ed. Philadelphia, PA: Elsevier Health Sciences; 2006:796.
7. Ferrari M, Scotti R. Fiber Posts: Characteristics and Clinical Applications. Paris, France: Masson Publishing; 2002:40.
8. Freilich MA, Meiers JC, Duncan JP, Goldberg AJ. Fiber-Reinforced Composites in Clinical Dentistry. Hanover Park, IL: Quintessence Publishing; 2000:11.
9. Pegoretti A, Fambri L, Zappini G, Bianchetti M. Finite element analysis of a glass fibre reinforced composite endodontic post. Biomaterials. 2002;23(13):2667-2682.
10. Lanza A, Aversa R, Rengo S, et al. 3D FEA of cemented steel, glass and carbon posts in a maxillary incisor. Dent Mater. 2005;21(8):709-715.
11. Garbin CA, Spazzin AO, Meira-Júnior AD, et al. Biomechanical behaviour of a fractured maxillary incisor restored with direct composite resin only or with different post systems. Int Endod J. 2010;43(12):1098-1107.
12. Coelho CS, Biffi JC, Silva GR, et al. Finite element analysis of weakened roots restored with composite resin and posts. Dent Mater J. 2009;28(6):671-678.
13. Ferrari M, Sorrentino R, Zarone F, et al. Non-linear viscoelastic finite element analysis of the effect of the length of glass fiber posts on the biomechanical behaviour of directly restored incisors and surrounding alveolar bone. Dent Mater J. 2008;27(4):485-498.
14. Tomazinho FSF, Zaitter S, Silva SRC, et al. Flexural properties of fiber reinforced root canal posts [abstract]. J Dent Res. 2010;89(spec iss B). Abstract 3115.
15. Beck P, Ghuman T, Cakir D, et al. Evaluation of flexural strength and elastic modulus of endodontic posts [abstract]. J Dent Res. 2009;88(spec iss A). Abstract 3065.
16. Seefeld F, Wenz HJ, Ludwig K, Kern M. Resistance to fracture and structural characteristics of different fiber reinforced post systems. Dent Mater. 2007;23(3):265-271.
17. Galhano GA, Valandro LF, de Melo RM, et al. Evaluation of the flexural strength of carbon fiber-, quartz fiber-, and glass fiber-based posts. J Endod. 2005;31(3):209-211.
18. Dietschi D, Romelli M, Goretti A. Evaluation of post and cores in the laboratory: rationale for developing a fatigue test and preliminary results. Compend Contin Educ Dent Suppl. 1996;(20):S65-S73.
19. Grandini S, Goracci C, Monticelli F, et al. An evaluation, using a “three-point bending” test, of the fatigue resistance of certain fiber posts. Il Dentista Moderno. March 2004;70-74.
20. Duret B, Duret F, Reynaud M. Long-life physical property preservation and postendodontic rehabilitation with the Composipost. Compend Contin Educ Dent Suppl. 1996;(20):S50-S56.
21. Wiskott HW, Meyer M, Perriard J, Scherrer SS. Rotational fatigue-resistance of seven post types anchored on natural teeth. Dent Mater. 2007;23(11):1412-1419.
22. Grandini S, Goracci C, Monticelli F, et al. Fatigue resistance and structural characteristics of fiber posts: three-point bending test and SEM evaluation. Dent Mater. 2005;21(2):75-82.
23. Grandini S, Chieffi N, Cagidiaco MC, et al. Fatigue resistance and structural integrity of different types of fiber posts. Dent Mater J. 2008;27(5):687-694.
24. Bonfante G, Kaizer OB, Pegoraro LF, do Valle AL. Fracture strength of teeth with flared root canals restored with glass fibre posts. Int Dent J. 2007;57(3):153-160.
25. Clavijo VG, Reis JM, Kabbach W, et al. Fracture strength of flared bovine roots restored with different intraradicular posts. J Appl Oral Sci. 2009;17(6):574-578.
26. Al-Wahadni AM, Hamdan S, Al-Omiri M, et al. Fracture resistance of teeth restored with different post systems: in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(2):e77-e83.
27. Akkayan B, Gülmez T. Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent. 2002;87(4):431-437.
28. Pameijer CH, Glantz PO, Mobasherat MA. On clinical corrosion of pins. Swed Dent J. 1983;7(4):161-167.
29. Rosenstiel SF, Land MF, Fujimoto J. Contemporary Fixed Prosthodontics. 3rd ed. Philadelphia PA: Mosby; 2001.
30. Schmage P, Wicht HS, Nergiz I, Pfeiffer P. Grey level differences between different root post materials and dentin [abstract]. J Dent Res. 2010;89(spec iss B). Abstract 0820.
31. McClendon K, Ripps A, Fan Y. Comparative study on radiopacity of fiber posts and resin cements [abstract]. J Dent Res. 2010;89(spec iss A). Abstract 0253.
32. Furtos G, Baldea B, Bratu D, et al. Radiopacity of fiber posts [abstract]. J Dent Res. 2010;89(spec iss A). Abstract 0142.
33. Goracci C, Corciolani G, Vichi A, Ferrari M. Light-transmitting ability of marketed fiber posts. J Dent Res. 2008;87(12):1122-1126.
34. Kim YK, Kim SK, Kim KH, Kwon TY. Degree of conversion of dual-cured resin cement light-cured through three fibre posts within human root canals: an ex vivo study. Int Endod J. 2009;42(8):667-674.
35. dos Santos Alves Morgan LF, Peixoto RT, de Castro Albuquerque R, et al. Light transmission through a translucent fiber post. J Endod. 2008;34(3):299-302.
36. Faria e Silva AL, Arias VG, Soares LE, et al. Influence of fiber-post translucency on the degree of conversion of a dual-cured resin cement. J Endod. 2007;33(3):303-305.
37. Cury AH, Pegoraro TA, Pereira JC, et al. Effects of polymerization-mode on the push-out retention of self-adhesive resin-cements [abstract]. J Dent Res. 2008:87(spec iss A). Abstract 0379.
38. Melo RM, Ozcan M, Barbosa SH, et al. Bond strength of two resin cements on dentin using different cementation strategies. J Esthet Restor Dent. 2010;22(4):262-268.
39. Mazzoni A, Marchesi G, Cadenaro M, et al. Push-out stress for fibre posts luted using different adhesive strategies. Eur J Oral Sci. 2009;117(4):447-453.
40. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int. 2008;39(2):117-129.
41. Sakkal S. Carbon-fiber post removal technique. Compend Contin Educ Dent Suppl. 1996;(20):S86.
42. Frazer RQ, Kovarik R, Chance KB, Mitchell RJ. Removal time of fiber posts versus titanium posts. Am J Dent. 2008;21(3):175-178.
43. Gesi A, Magnolfi S, Goracci C, Ferrari M. Comparison of two techniques for removing fiber posts. J Endod. 2003;29(9):580-582.
44. Anderson GC, Perdigão J, Hodges JS, Bowles WR. Efficiency and effectiveness of fiber post removal using 3 techniques. Quintessence Int. 2007;38(8):663-670.
45 . Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H. 10-year survival evaluation for glass-fiber-supported postendodontic restoration: a prospective observational clinical study. J Endod. 2012;38(4):432-435.