Clinical Case Report: An Interdisciplinary Approach for Congenitally Missing Maxillary Lateral Incisors
Norman W. Ickert, DMD; Perry H. Beeson Jr, DDS; and Kimberly L. Gragg, DDS, MS
Background
Age at Initial Presentation: 14
Initial Presentation: February 2004
Treatment Completed: January 2009
The patient’s main concerns were that her teeth were not properly aligned, two upper lateral incisors were missing, and the canines in the lateral incisor position did not present the proper appearance. She said it was important to have “normal” lateral incisors (Figure 1).
Medical History
The patient was a healthy 14-year-old with no current significant medical concerns. She had partial paralysis of the left maxillary lip as a result of minor facial surgery as a young child.
Diagnostic Findings
Temporomandibular Joints: Within normal limits (WNL)
Extraoral: Lip dynamics are affected on the upper left side.
Intraoral: The patient presented with retained maxillary primary cuspids and permanent maxillary cuspids in the lateral incisor position. Also, these cuspids were slightly underdeveloped on their mesial aspect. The patient had a history of regular dental care and excellent oral hygiene, requiring continual care and preventive dental procedures only (Figure 2).
Occlusal Notes
The occlusion is diagnosed as skeletal Class I with a mild Class II tendency. She presented with a dental Class II molar relation on the right and a Class I molar relation on the left. Maxillary lateral incisors were congenitally missing, and the maxillary primary canines were retained. The maxillary canines were in the position of the missing lateral incisors. The maxillary left first premolar was in buccal crossbite. The overjet was mildly increased, and the overbite was 60%. The maxillary dental midline was displaced 3 mm to the left, and the mandibular midline was coincident with the facial midline.
Radiographic Assessment
Adult dentition was not fully erupted, the primary cuspids were evident with minimal residual root present, only one third molar (No. 16) was developing, and the maxillary laterals were absent (Figure 3).
Diagnosis
Periodontal: AAP type 1
Biomechanical: No biomechanical compromises
Functional: Normal function consistent with current degree of total eruption of teeth
Dentofacial: Intra-arch malposed teeth, gingival tissue levels not harmonious, and the teeth too dark
Medical: WNL
Risk Assessment
Dentofacial: Moderate
Periodontal: Low
Biomechanical: Low
Functional: Low
Prognosis
The prognosis for this dentition was considered good but was highly dependent on the successful achievement of the orthodontic treatment to place the teeth in acceptable occlusion and to provide enough space for the placement of im plants in the maxillary lateral spaces. In addition, the prognosis depended on the placement of implants in adequate bone and management of the hard and soft tissues for the patient’s esthetic demands.
Concerns
- Can the teeth be positioned properly, not only to achieve normal acceptable occlusion but also to provide a minimal 6.5 mm of space for each maxillary lateral incisor, as well as having parallel roots at teeth Nos. 6 to 8 and Nos. 9 to 11 to facilitate implant placement?
- After moving the canines to their normal position, will the bone have adequate thickness facially and lingually at tooth position Nos. 7 and 10?
- If the thickness of the maxillary ridge is inadequate postorthodontically, then a form of bone-augmentation treatment will be required (a ridge split with simultaneous expansion procedure, guided bone regeneration, or conventional onlay bone grafting).
- The tissue type is relatively thin, the teeth are more triangular than square, the relative tissue levels must be managed, and the resultant osseous crest preferably should be normal or high.
- Enhancing the tissue volume and quality on the facial of Nos. 7 and 10 is a consideration for esthetics and long-term tissue stability.
Treatment Goals
- Maintain oral health during treatment phases.
- Predictable, minimally invasive, prosthetic replacement of the missing lateral incisors.
- Meet the patient’s esthetic goals.
- Answer the psychological need to have a “normal” dentition.
- Provide a stable, protective, and acceptable occlusion.
Treatment Plan
To address her needs, several options were offered to the patient:
- Orthodontic treatment and resin-bonded bridges to replace the lateral incisors.
- Conventional bridgework. (This was not encouraged because of the inevitable biomechanical compromise and long-term guarded prognosis.)
- Orthodontic treatment, followed by dental implants and implant-supported crowns.
The patient and her parents chose option 3.
Phase I: Orthodontics
Orthodontic appliances (MBT™ Versatile + Appliance System, 0.018 slot 3M Unitek, St. Paul, MN) were bonded into place. A Herbst appliance was fabricated and delivered 3 weeks later. Primary canines were extracted after all orthodontic hardware was in place, and composite was bonded onto the mesial of the maxillary first premolars to fill the vacancy of the extracted primary canines (for esthetics). The Herbst appliance was advanced on the left slightly and the right at 4-week intervals to achieve anterior-posterior correction and to distalize maxillary molars during canine retraction. As the canines were retracted, the composite was removed from the premolars. Eventually, prosthetic lateral incisors were placed on the archwire.
The maxillary canines were fully retracted in 8 months, and the Herbst appliance was removed 1 month later. Then, rubber band wear was used to detail occlusion and finalize midline correction. After most of the vertical growth had occurred, resin-bonded bridges were cemented and Essex retainers fabricated for retention until the implant phase could be started (Figure 4, Figure 5 and Figure 6).
Phase II: Management of the Hard and Soft Tissue—Dental Implant Placement
The dental implant phase began in January 2008. The following five diagnostic keys for implant success in the esthetic zone are critical for formulating a treatment plan:
- Relative tooth position (both apical/coronally as well as buccal/lingually)
- Tissue biotype (thick, medium, thin)
- Tooth shape (square, ovoid, triangular)
- Osseous crest level (high, normal, low)
- Scallop form (flat, normal, high)1,2
The significant findings relative to these five diagnostic keys:
- The tissue biotype was relatively thin.
- The teeth were more triangular than square.
- The bone thickness buccal-lingually at the surgical sites was deficient, precluding a conventional implant-placement technique.
Hard- and soft-tissue augmentation was required. The technique of splitting the edentulous maxillary ridge (sandwich graft), expanding the bone, along with a simultaneous pediculated connective soft-tissue graft, was chosen to address these concerns. The rationale for expansion of the ridge, with simultaneous soft-tissue augmentation, was not only to provide enough bone volume for implant placement, but also to provide a more pleasing soft-tissue framework for the implant-supported crown. A concave soft-tissue contour creates a slight shadow, whereas a convex soft-tissue profile allows light reflection for the viewer. This increased light reflection/light creates a more pleasing esthetic outcome.
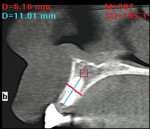
The bone was well-suited for the ridge split as the Hounsfield reading from the cone-beam computed tomography (CBCT) scan was in the range of 340 Hounsfield units (HUs) to 400 HUs. (It is understood that these readings are relative gray levels and not pure HUs as determined by medical-grade computed tomography.)
The surgeries were initiated with a 10-mm long supraperiosteal incision lingual to the osteotomy site. With internal mesial-, distal-, and apical-releasing incisions, as well as a full-thickness flap elevation over the crest and toward the buccal, a pediculated connective soft-tissue graft was harvested and access to the osteotomy site gained.
The center of the ridge was located with a fitted Vassos Implant Position System ring (VIPS, Edmonton, AB, Canada) and a precision drill (Nobel Biocare,™ Göteborg, Sweden) was used to initiate the osteotomy. The ANKYLOS® surgical kit twist drill (DENTSPLY Friadent Ceramed, Lakewood, CO) was used to a depth of 9 mm and the angulations verified radiographically with a position indicator (Nobel Biocare). The ridge was split with an 1169 bur mesial-distally (Figure 7). Access for a diamond disk was insufficient.
The exposed alveolar ridge was expanded horizontally, using a split-control kit (Meisinger USA, LLC, Centennial, CO), taking care not to fracture the cortical plates. The site was refined further with an ANKYLOS® size A osteotome (DENTSPLY Friadent Ceramed) to condense the bone and shape the osteotomy prior to final preparation with the conical reamer. An ANKYLOS A11 implant (DENTSPLY Friadent Ceramed) was placed 1 mm below the bone crest because of the significant platform-switch design of this implant system. There was 1.5 mm of bone mesial and distal to the implant and 2 mm to the facial. These are critical parameters for health and long-term retention of the hard and soft tissues. The pediculated graft was rolled under the facial flap to augment the soft-tissue volume. This augmented soft tissue was then sutured to the palatal gingiva. The resin-bonded bridge provisionals were re-cemented with a self-adhesive resin cement (Figure 8).
Phase III: Restorative
The restorative phase was initiated 10 weeks after implant placement. After the resin-bonded were removed, an incision was made lingual to the implants and the tissue released to the facial. The ANKYLOS A11 cover screws were removed, and standard analog abutments were tried in using an Essex retainer to evaluate space. A 1.5-mm to 4-mm straight standard abutment was chosen for each implant (Figure 9). Bis-acryl provisionals were made and cemented with a temporary crown-and-bridge cement. The tissue was approximated around the provisional and sutured (Figure 10).
After 2 weeks of healing, the provisionals were removed and a closed-tray polyvinyl siloxane impression was taken. Two weeks later, porcelain fused to metal crowns were tried in and cemented with Premier Implant Cement (Premier Dental, Plymouth Meeting, PA) (Figure 11).
The height of the interproximal gingival tissues around an implant-supported restoration is dependent on the bone level of the adjacent natural teeth.3 The bone on the facial of the implant determines the height of facial tissue. Conservative flap management,4 development of thicker tissue biotype,5 surgical and prosthetic selection of the implant and abutment design to minimize the micro-movement via a Morse taper internal connection and a platform (abutment/implant) switch to promote increased soft-tissue volume, and minimizing inflammation by medializing and decreasing the biologic width are all major factors that influence the final position of the tissues around the implant-supported restoration.6 Other factors include minimizing the number of disconnections and reconnections of the abutment/implant assembly.7 Complete maturation of the gingival tissue takes several months.8
At 1-year postsurgery, the peri-implant and interproximal tissues were maturing and a more normal gingival architecture was realized. Select contouring of the anterior teeth was accomplished to improve the overall esthetic result (Figure 12, Figure 13, Figure 14, Figure 15, Figure 16, Figure 17, Figure 18 and Figure 19).
Phase IV: Maintenance
Regular continuous care appointments were kept. No increase in risk factors had been realized.
Commentary
The patient achieved her goals of replacement of her missing lateral incisors, improved occlusion, and pleasing esthetic results. More importantly, the results afforded the patient a sense of completeness and improved confidence.
This interdisciplinary approach necessitated a treatment-planning process that started with the final outcome in mind. The incisal edge position, occlusal plane, orthopedic position, and esthetic factors were anticipated and planned from the start.
Respecting the five keys to esthetic success for implants in the esthetic zone and anticipating potential hard- and soft-tissue variables and how to address them during the surgical and prosthetic phases, assured the greatest likelihood for success, both in the short and long term. The detailed orthodontic placement of the teeth in the arch and face and with adequate interroot space for implant placement was equally important. Ideal esthetics requires ideal tooth position.
Although there can be only one correct diagnosis, various treatment options are possible, each with a different long-term prognosis. Surgically, other treatment modalities for splitting and expanding the ridge could have been the use of Piezosurgery® (Mectron s.p.a, Carasco, Italy) or a scalpel blade, with the use of D spreaders. Prosthetically, lab selected customized-machined and contoured abutments (ANKYLOS Balanced Abutment System, DENTSPLY Friadent Ceramed) also could have been selected.
The approach used for this patient, with missing and improperly aligned teeth, illustrates the rationale and execution of an interdisciplinary treatment plan. This treatment facilitated the management of the patient’s functional, esthetic, and psychological needs in a relatively noninvasive and long-term predictable manner. The results were very acceptable to the patient and exceeded her expectations.
References
1. Phillips KM, Kois JC. Aesthetic peri-implant site development. The restorative connection. Den Clin North Am. 1998;42(1):57-70.
2. Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001;22(3): 199-206.
3. Salama H, Salama MA, Garber D, et al. The interproximal height of bone: a guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998;10(9):1131-1141.
4. Gomez-Roman G. Influence of flap design on peri-implant in terproximal crestal bone loss around single-tooth implant. Int J Oral Maxillofac Implants. 2001;16(1):61-67.
5. Kan JY, Rungcharassaeng K, Umezu K, et al. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol. 2003;74(4):557-562.
6. Weigl P. New prosthetic restorative features of the Ankylos im plant system. J Oral Implantol. 2004;30(3):178-188.
7. Abrahamsson I, Berglundh T, Lindhe J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J Clin Periodontol. 1997;24(8): 568-572.
8. Small PN, Tarnow DP. Gingival recession around implants: a 1-year longitudinal prospective study. Int J Oral Maxillofac Implants. 2000;15(4):527-532.
About the Authors
Norman W. Ickert, DMD
Private Practice
Langley, British Columbia, Canada
Director of Ickert Teaching Centre
Langley, British Columbia, Canada
Clinical Instructor
Kois Center
Seattle, Washington
Perry H. Beeson Jr, DDS
Private Practice
Morganton, North Carolina
Clinical Instructor
Kois Center
Seattle, Washington
Kimberly L. Gragg, DDS, MS
Private Practice
Morganton, North Carolina