Mandibular Arch Immediate Implant Loading Using a Modified-SLA Surface
A Series of 21 Cases in a Private Periodontal Practice Incorporating an Interdisciplinary Team Approach: Clinical Technique and Laboratory Protocol
Abstract:
This article describes a standardized technique for immediate loading of madibular arch cases using an interdisciplinary team approach. This approach has evolved over the past 15 years based on the authors' clinical experience with immediate loading. The technique can be applied to preexisting fully edentulous mandibular arches and full-arch extractions with immediate implant placement and loading. A clinical study of 21 similarly treated mandibular arches using the new SLActive surface (a modified hydrophilic SLA surface) in the primary author's private implant surgical practice has shown a > 99% cumulative survival rate at 2 years with commencing of final restoration after 4 weeks.
The use of dental implants to replace missing teeth has become the standard of care for edentulous spaces, as well as providing replacement for periodontally or restoratively hopeless teeth.1-6 Treatment planning decisions using a team approach to therapy involve the patient, restorative dentist, dental laboratory technician, and the oral plastic-reconstructive surgeon. This interdisciplinary approach has the patient's best interests in mind, as duties are assigned to each specialist in his or her respective field. This approach results in a seamless experience through the end of active treatment and into the maintenance phase of care. Treatment planning is the most critical phase because it focuses on the final restoration first and then flows backwards toward the surgical phase. This becomes even more important in immediate loading of single, partial, and full arch cases because each preceding step affects the subsequent step in a cascading fashion.7-16
The literature-based clinical studies and case reports on immediately loaded implants present techniques that have validity and similar outcomes to conventionally loaded implants.17,18 However, for the team and patient, the attention to detail and precision of each step is more critical than in a conventional loading protocol of 6 to 12 weeks.19 For immediately loaded cases, the authors' experiences have shown that working with clinicians outside of the team can significantly increase the risk of an unsuccessful outcome. The laboratory technician may not understand specific surgical needs when designing the surgical guide template or the provisional restoration. The restorative dentist or surgeon may be cavalier about the fine details needed to assure precise surgical implant placement or seamless fit of the provisional restoration. A demanding noncompliant patient may create "patient interference" during the healing phase by not following postoperative instructions.11 Assembling the proper team members and choosing the right patient at the outset of treatment are critical determinants as to whether an immediate load approach should be used or avoided.
Modified-SLA Implant Surface
The sand-blasted and acid-etched (SLA®) surface (International Team for Implantology [ITI], Basel, Switzerland) has become the gold standard in surface design since its inception in 1994.20 A clinical multicenter international study of 92 practitioners in 17 countries reported a cumulative survival rate of 99.26% at 5 years with the SLA-surface implant being restored 6 to 8 weeks after implant placement.
Implants are at their greatest risk between 2 and 4 weeks after surgery, when the initial "primary" bone stability is being eroded by osteoclastic activity. The new "secondary" bone is not far enough advanced by osteoblastic activity to produce new replacement bone that will be able to withstand excessive loading. This approximate 2 to 4 week postsurgical time period has been established as the weak link in implant healing.
In 2004, further SLA surface chemical modification began, along with a series of animal and human studies which tested this new modified-SLA surface (SLActive, Straumann USA LLC, Andover, MA). These studies are proving that when the surface chemistry is altered to become hydrophilic, the osseointegration process is jump-started and the "stability dip" at 2 to 4 weeks becomes almost immaterial. This preconditioned surface enhances protein attraction, which allows blood cells to use the SLA surface topography optimally and move into the deep micropores of its surface. This initiates the osseointegration process.21 The "wetability" of the SLActive surface improves the adhesion and stability of the initial blood clot, which begins to initiate within 24 hours. This leads to earlier angiogenesis and formation of blood capillaries, which precedes the formation of new bone.22,23 Because of these important hydrophilic surface characteristics of the SLActive surface, implants reached full stability 2 weeks earlier than with SLA. When compared with SLA implants, histological observations in miniature pigs showed significantly more bone-to-implant contacts with SLActive at 2 and 4 weeks of healing.24
An ongoing 5-year clinical study on the SLActive surface, which has passed the 2-year point at the time of this publication, also has shown that the implants have the ability to go to restorative completion at 3 weeks (mandible) and 4 weeks (maxillae) in single posterior sites. This was accomplished when 35 Ncm torque or greater was delivered successfully at implant insertion and retested at 3 weeks (mandible) and 4 weeks (maxillae) with 35 Ncm reverse torque, thus confirming secondary bone stability.25 As far as time of completion is concerned, this now converts implant dentistry to crown-and-bridge dentistry. A study also has confirmed that the soft tissues are ready at 3 weeks.26 The final ideally contoured crown acts as a provisional, sculpting the tissues and allowing the residual interproximal spaces to fill in over time. This has been observed in the first 6 months following implant crown insertion.25 The benefits with this new chemically active surface theoretically will be seen in type IV bone (posterior areas, especially in the maxillae), where primary stability is minimal, and will enable patients to go to restorative completion in approximately half the time (3 to 4 weeks) in nontype IV bone when compared with the SLA surface (6 to 12 weeks). Immediately loaded cases, especially in the maxillae, where documented failures of distal abutments in type IV bone and sinus augmentation procedures are more common, also would benefit from this improved chemically modified implant surface.11,25,27
Immediate Loading of Mandibular Full and Partial Arches Using SLActive Implants
The Third ITI Consensus Conference (August 2003) defined immediate loading as the placement of a restoration in occlusion with the opposing dentition within 48 hours of implant placement.12 Ganeles and colleagues9 noted the indications and benefits for immediate loading.
Indications
- When removable temporization may cause excess transmucosal loading of the implants or the patient may not be able to nor desire to wear a removable appliance.
- When the clinician is concerned that the patient may be without teeth for any length of time because he or she is not able to predict the patient's ability to wear an immediate denture comfortably after surgery. (An immediately loaded fixed prosthesis can be worn almost immediately after surgery.)
- When there are time concerns with the patient. (Significant chair time reduction has been seen when the authors avoid a removable provisional appliance, which usually needs multiple postsurgical restorative appointments and adjustments for the patient to become comfortable. With an immediately loaded fixed provisional, inserted 3 to 5 days after surgery, the authors have noticed that the patient is significantly more comfortable, and requires far fewer restorative adjustments. Further, the patient's self-esteem, comfort, and overall satisfaction are significantly greater with an immediately loaded provisional.)
- With the SLActive surface there is less time to restorative completion and greater potential for improved implant survival.25,27
- A biologic rationale now exists. (Bone-to-implant contacts have been shown to be increased significantly with immediate loading.13,28,29)
- Clinical studies have shown similar results as with a conventional leading protocol.17
Benefits
Between April 2006 and December 2007, 21 cases of SLActive immediately loaded mandibular full and partial arch cases have been treated in a private periodontal practice setting using a team approach. The following case report is an example of the procedure and the provisional technique used in the authors' daily practice.
Case Report
On referral from his restorative dentist, a 47-year-old male registered nurse presented to the authors' periodontal office with a chief complaint of wanting to replace his missing teeth (Figure 1, Figure 2, Figure 3, Figure 4 andFigure 5). He had recently lost a tooth in his upper right area and was concerned with the health of his remaining loose teeth. After the completion of a comprehensive clinical examination and full mouth digital radiographs, his restorative dentist discussed his advanced periodontal disease and the probable loss of his remaining teeth. He then reviewed the restorative options with the patient. The team approach starts in the restorative office and, through communication with the patient and the periodontal office, enables a fluid discussion, resulting in a more informed patient. The patient stated the desire "to turn his life around" medically and dentally, with eventual smoking cessation, weight loss, and better control of his diabetes and hypertension. For the final restoration, he expressed a strong desire for a fixed restoration in both arches.
Medical and Dental Histories
1. Poor compliance to prevention, a known risk factor for periodontal disease progression.30 He had not had any routine care for a number of years.
2. Hypertension and insulin-dependant diabetes, a condition associated with periodontal disease and a risk factor for successful implant treatment.31-33
3. Two-pack per day smoking habit. At presentation he was aware of the surgical concerns with smoking (a risk factor for successful implant treatment34) and had started cutting back with a goal of eventual cessation. By the time of the surgical visit he had reduced his smoking to less than half a pack per day.
4. Nocturnal bruxing habit.
Clinical Exam
Clinical examination revealed heavy plaque and calculus deposits with very heavy bleeding on probing, generalized deep probing depths (> 7 mm), and generalized severe mobilities (2+ to 3 degrees) in the remaining teeth (Nos. 6 through 9, 11, 13, 20, and 22 through 31).
To evaluate buccal and lingual undercuts, it would be necessary to examine hard and soft tissue, both facially and lingually, as well as areas of mucogingival defects. This would be confirmed with subsequent computed tomography (CT) scans. The examination was completed with a full series of digital photographs and a panoramic radiograph to view the vertical height of bone in the lower jaw, as well as other anatomical areas of concern (maxillary sinus and mandibular canal). This information was downloaded into the patient's digital picture file and a computerized case presentation was produced with pictures and radiographs to review with the patient at the consultation visit.
A CT scan is recommended as standard procedure in the authors' office for all immediate load full and partial arch cases to reduce and/or eliminate any guessing. The patient was informed that final treatment planning would be dependant on his bone quality and quantity and would be reviewed with him at his next visit. Proposed treatment plans, treatment times, and fees, along with the patient's digital pictures, were reviewed with him at the second visit. As part of the case presentation, any treatment options, as well as other similarly treated and documented digital case presentations, were shared with the patient. This way the patient had a very good visual picture of how the final restorations would appear. It has been shown that in customized case presentations, visual aids can be very powerful tools for patients, helping them understand their problems, necessary treatment, and options—allowing them to make a final educated and informed decision.35
After receiving the CT scan, a thorough review was then completed with regard to proposed implant sites, lengths, widths, and areas in possible need of guided bone regeneration (GBR) or socket preservation. The anticipated surgical vertical reduction (osteoplasty) of the alveolar bone height needed for restorative and patient posttreatment plaque control ease also was determined. This vertical hard-tissue reduction was communicated with the laboratory to facilitate better stability of the surgical guide stent. Final discussions regarding proposed implant sites, and provisional and final case designs were discussed with the restorative dentist and the laboratory technician. Lastly, the patient returned to the office for his case presentation, which included possible alternative treatment that might be necessary if the implants could not be immediately loaded. No promises are ever made, except that the authors will do the best they can to deliver the desired restoration. A discussion relating the systemic link between periodontal infection and heart disease, along with diabetes, was reviewed with the patient. His diabetes also would be better controlled through the treatment of his periodontal condition, which in his case would involve full mouth extractions and dental implants.
The final treatment plan for a fixed restoration was developed and reviewed with the patient.
1. Final restorative discussions with fabrication of a full upper denture (FUD) and surgical guide stent. In addition, medical clearance for the proposed treatment plan with further reduction and/or smoking cessation was advised.
2. In one surgical visit: extraction of the eight remaining maxillary teeth with socket preservation to promote ridge maintenance for future implant placement in 6 months,36,37 and surgical extraction of the remaining 11 mandibular teeth with immediate implant placement. Placement of eight implants in the lower jaw with evaluation for GBR as needed at the time of implant placement, along with socket preservation as needed. Proposed implant sites included Nos. 18, 19, 21, 23, 26, 28, 30, and 31. The authors generally place six implants for a mandibular fixed-hybrid case. Because the patient presented with a large body frame and history of bruxism with secondary occlusal trauma, the authors decided to engineer his case with eight implants (four per quadrant). In addition, placing eight implants would enable second molar occlusion without the need for cantilevers or long spans between implant abutments. If adequate insertion torque of at least 35 Ncm25,38,39 was able to be delivered at insertion of at least four well-spaced sites, then the restorative dentist, who would be in attendance for patient convenience, would take impressions and bite registration during surgical visit. Based on presurgical bone availability, a fixed screw-retained metal-reinforced provisional was presented to the patient as probable, but not definite.
3. Delivery of the fixed screw-retained provisional restoration11,16,27 in the restorative dentist's office within 3 to 5 days after surgery. The surgical date was scheduled and prebooked with the laboratory technician who had set aside time to ensure that the provisional could be delivered to the restorative office in 4 days.
4. Commence completion of the final case 6 to 12 weeks later. The time to completion would be based on insertion torque values on the day of surgery, and the radiographic evaluation of implant healing at 6 weeks.
5. Commence periodontal maintenance phase, alternating every 3 months between the restorative and periodontal offices. There also would be a second CT scan of the maxillae taken at least 4 to 6 months after extractions to aid in final surgical and prosthetic treatment planning of the maxillary case.
Surgical Procedure
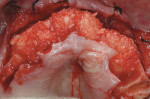
Because the patient reduced his smoking habit to less than five cigarettes per day and his diabetes was stable, he was viewed as surgically ready to proceed with treatment as proposed. The patient was premedicated with amoxicillin, chlorhexidine rinses, and naproxen sodium 1 hour before surgery and was dosed for 10 days with amoxicillin (500 mg q.i.d.) and 5 days with naproxen sodium (550 mg b.i.d.). The patient was given hydrocodone with acetaminophen postsurgically for management of any additional pain. Steroids were avoided because of his diabetes status. Surgical anesthesia was completed with local infiltration in the maxillae as well as posterior superior and bilateral mandibular nerve blocks. With the aid of ultrasonic bone surgery, all remaining teeth were removed in one visit.40-43 Piezosurgery® extraction tip inserts EX 1 and EX 2 (Piezosurgery®, Inc, Columbus, OH) were used for buccal osseous preservation, followed by thorough debridement with OT 4, OP 3, OP 4 inserts of all infected sites after tooth removal by extraction forceps (Figure 6, Figure 7 and Figure 8). When used with copious amounts of sterile saline solution, the vibration frequency in the range of 20 kHz to 32 kHz has the ability to cut hard tissues (teeth and bone) without damaging soft tissues.41,43 This approach has been used routinely in the authors' office for the past 2 years with excellent postoperative surgical results. The technique is minimally invasive, causing less trauma and more predictable buccal bone maintenance and postoperative healing than conventional extraction techniques.41,43 The key is using light continuous pressure and keeping the tip inserts in constant movement along the long axis of the tooth. This prevents any heat-related damage to the osseous tissues. In addition, autogenous osseous chips were saved during mandibular vertical ridge reduction (using OP 3 insert) and used for socket preservation in site Nos. 22 through 24. After thorough socket debridement with the specified Piezosurgery tips, socket preservation was completed in the maxillary sites by lightly packing Regenaform® bone graft material (Exactech, Inc, Gainesville, FL) and covering it with resorbable collagen membranes. This technique promotes GBR44 (Figure 9 through Figure 17). Site No. 23 was originally treatment planned by CT analysis as an implant site, but was found to be unusable because of significant osseous loss in the Nos. 22 and 23 areas. Site No. 24 was used as the alternative site. Even with high-tech diagnostic aids, the final implant position needs to be decided after flap entry and osseous reevaluation. Based on what the surgeon finds clinically at the time of implant placement, surgical flexibility is necessary for all members of the team. This may require an alteration in final prosthetic and surgical fees. Implant sites, lengths, widths, and the insertion torque values were:
Site No. 18: 10 mm Wide Neck (WN) x 4.8 mm SLActive; 35 Ncm torque delivered
Site No. 19: 10 mm WN Tapered Effect (TE) x 4.8 mm x 6.5 mm SLActive; 20 Ncm
Site No. 21: 12 mm Regular Neck (RN) x 4.8 mm SLActive; 20 Ncm
Site No. 24: 12 mm RN x 4.1 mm SLActive; 35 Ncm
Site No. 26: 12 mm RN x 4.1 mm SLActive; 35 Ncm
Site No. 28: 10 mm RN TE x 4.1 mm x 4.8 mm SLActive; 20 Ncm
Site No. 30: 10 mm WN TE x 4.8 mm x 6.5 mm SLActive; 15 Ncm
Site No. 31: 10 mm WN TE x 4.8 mm x 6.5 mm SLActive; 15 Ncm
Because adequate lengths and widths were placed, it was decided to immediately load this case from site Nos. 19 through 30, while leaving site Nos. 18 and 31 to heal unloaded. First molar occlusion would be sufficient for the healing phase. Ideally, a 35-Ncm torque on all six implants to be loaded would be preferred for immediate loading. After the treatment decision was made, possible risks of immediate load failure because of initial torque values of only 15 Ncm to 20 Ncm (sites Nos. 19, 21, 28, and 30) were discussed with the restorative dentist and the patient. The decision was made to place the fixed provisional because it would not be prone to transmucosal loading of the unsplinted implant underneath it.
Restorative Provisional Phase
In an edentulous patient, before surgical guide stent fabrication, a complete denture wax up is tried in the mouth. Phonetics, esthetics, and occlusion are checked by the dentist and approved by the patient. In a partially edentulous patient, teeth are set up in the edentulous areas for try in. Desired esthetic and occlusal changes are noted at this time and discussed with the laboratory. Tooth position and occlusion can be copied and incorporated into the surgical guide stent. A properly created implant guide stent will provide for proper implant positioning and a predictable final restoration.
The implant guide stent is used not only by the surgeon, but also by the restorative dentist to make the bite registration. A proper bite registration impression is critical to the success of an immediately loaded fixed provisional, and would be difficult to record without a well fitting guide stent. At the surgical visit, the patient was in the chair for an extended length of time, sedated, and under the influence of local anesthesia. Vertical studies at this stage were impractical and would not be reliable. Because the guide stent is a copy of the denture setup, occlusion can be checked and vertical dimension reestablished. The surgical flaps were lightly sutured back into place to allow for easy placement of the impression copings and temporary cylinders. Two temporary cylinders were screwed into the implants and radiographs taken to insure that they were completely seated. The stent was adjusted to passively seat around the cylinders and the cylinders were adjusted to allow for proper occlusion. Using a salt and pepper powder and liquid technique, acrylic was used to lute the stent to the cylinders. After the acrylic hardened, the occlusion was rechecked and a bite registration was made using fast-set polyvinyl siloxane bite registration material (Figure 18). The occlusal rim then was unscrewed and set aside.
Closed tray synOcta® plastic impression copings (Straumann USA LLC) were seated on the molar implants and open tray synOcta impression copings were screwed into the remaining four anterior implants (Figure 19). A polyether final impression was then made (Figure 20). The author chose polyether impression material because of its rigidity. Tall temporary healing caps were lubricated with antibiotic ointment and lightly hand tightened. The surgeon then completed suturing, and the surgical phase was finished (Figure 21). The final impression and occlusal rim were hand delivered to the laboratory. Because the laboratory already had the counter model and the necessary denture teeth, the technician immediately began fabricating the fixed provisional (Figure 22, Figure 23 and Figure 24).
The patient was seen for surgery on a Friday and the metal-reinforced provisional restoration was inserted the following Tuesday, 4 days after surgery, in the restorative office. Occlusion was checked, and periapical and panoramic radiographs were made to confirm the provisional's fit (Figure 25 and Figure 26). Digital photos also were taken at that time. Postsurgical plaque control techniques were reviewed with the patient, and a soft diet was recommended for 4 weeks. Additional postoperative visits were scheduled for every 2 weeks until 6 weeks after insertion, when a periodontal maintenance appointment was completed.
At 3 months after surgery, using radiographic evaluation and successful reverse torque of 35 Ncm for all sites (Figure 27), final determination was made to go to restorative completion. Reverse torque was accom-
plished using the implant carrier devices for RN and WN implants. This confirmed secondary bone healing and adequate bone-to-implant contacts. The implants were ready to accept the 35 Ncm of torque needed for final abutment placement. The final case was delivered uneventfully (Figure 28 and Figure 29). After radiographic confirmation of being fully seated, all abutments were torqued to 35 Ncm. The occlusion was checked in intercuspal and contacting movements, and a final digital photographic series was taken. By the end of treatment the patient had lost more than 30 lbs and his glycosylated hemoglobin (Hb A1c) level was 7% (Figure 30, Figure 31, Figure 32 and Figure 33).
Discussion
The presented case is a typical example of how the authors plan and treat mandibular cases that present for immediate loading of full and partial arches. Our approach to immediate loaded cases has become more standardized and has changed significantly since our first full arch immediately loaded maxillary and mandibular cases treated in 1994.8
The use of the "indirect technique" for provisonalization saves the patient and clinician an average of 2 hours when compared with the "direct technique" (pickup technique). Significant chair time is saved because the provisional is completed in the laboratory. When the screw-retained laboratory-processed provisional is inserted 3 to 5 days later, a 2- to 3-hour insertion visit is reduced to less than 1 hour. Also, the addition of a casted metal-reinforced bar in the provisional has eliminated the risk of provisional fracture. Acrylic fracture can occur when using the direct technique of converting the full lower denture (FLD) to a fixed screw-retained provisional. If for some reason, the case could not be immediately loaded, fabrication of a FLD within the same time frame would not be a problem because the laboratory already had an accurate denture setup from the fabrication of the surgical guide template. The patient is aware of this possibility and though he or she may be disappointed, it is not a surprise. Of all the possible immediate loaded cases the authors have treatment planned in the past 14 years, no patient has been disappointed. This outcome is largely created by constant communication between team members, rigorous comprehensive treatment planning, and routine CT scan analysis, along with the meticulous surgical and prosthetic procedures as outlined.19,45
Since converting from SLA to SLActive implants in April 2006, the authors have treated 21 mandibular full and partial arches (114 implants) in patients using the above surgical and prosthetic protocols. Of these implants, 101 were loaded within 3 to 5 days. One early loaded failure was seen in the area of site No. 26 in a 75-year-old woman with borderline osteoporosis. (Now, osteoporosis is noted as a contraindication for early and immediate loading and should be avoided to allow a conventional healing period of 6 to 12 weeks before loading.46) The cumulative survival rate is greater than 99% to date for our immediately loaded SLActive cases.
The importance of an ongoing periodontal maintenance phase cannot be understated with the presented case. Diabetes, poor compliance to prevention, smoking, bruxing, and a history of advanced periodontitis are significant risk factors for tooth loss as well as implant loss. At each periodontal maintenance visit (1 hour in length), the patient was checked for important indices of disease progression, such as bleeding on probing and probing depth measurements, as well as mucogingival and prosthetic changes, and the patient's plaque control performance. Clinical studies support the hypothesis that an increased susceptibility for periodontitis also may imply an increased susceptibility for peri-implantitis, as the microbial flora responsible for periodontitis also are associated with peri-implantitis and implant loss.47,48 A night guard to control parafunction, occlusal wear, and excessive loading of the implants would be appropriate after his maxillary FUD is replaced by a fixed-hybrid restoration. A second CT scan of the maxillae revealed a well healed ridge, which was maintained by the previous socket preservation/bone grafting that was completed at the extraction and implant placement visit. Planning for the future implant placement in the maxillae by using predictable ridge preservation techniques will enable a straightforward surgical visit to place the maxillary implants.
Comprehensive team treatment planning is recommended for all cases treatment planned for immediate loading. By doing so, this complex, complicated, interdisciplinary treatment is broken down into specific parts, where each team member excels in his or her respective area of expertise: ie, restorative, surgical, or laboratory. The experience becomes "seamless" for the patient, as all team members have discussed each phase thoroughly with each other throughout treatment, alleviating any untold surprises and stress to all members of the team. The level of respect for each member's area literally shines through to the patient as he or she experiences something truly exceptional and very often life-changing. The total investment in time and money for the patient is greatly valued and is matched only by the level of appreciation. This level of patient appreciation is so strong that when asked, the patient often states, "I would do it again without hesitation."
Disclosure
Dr. Levine receives honorarium from Straumann USA, LLC and Piezosurgery®, Inc. He is also a consultant for the International Team for Implantology.
References
1. Adell R, Lekholm U, Rockler B, et al. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416.
2. Laney WR, Jemt T, Harris D, et al. Osseointegrated implants for single-tooth replacement: progress report from a multicenter prospective study after 3 years. Int J Oral Maxillofac Implants. 1994;9(1):49-54.
3. Buser D, Mericske-Stern R, Bernard JP, et al. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997;8(3):162-172.
4. Levine RA, Clem D, Beagle J, et al. Multicenter retrospective analysis of the solid-screw ITI implant for posterior single-tooth replacements. Int J Oral Maxillofac Implants. 2002;17(4):550-556.
5. Iacono VJ, Cochran DL. State of the science on implant dentistry: a workshop developed using an evidence-based approach. Int J Oral Maxillofac Implants. 2007;22(Suppl):7-10.
6. Hammerle CHF, van Steenberghe D. The first EAO Consensus Conference 16-19 February 2006, Pfäffikon, Switzerland. Clin Oral Implants Res. 2006;17(Suppl 2):1.
7. Tarnow DP, Emtiaz S, Classi A. Immediate loading of threaded implants at stage 1 surgery in edentulous arches: ten consecutive case reports with 1- to 5-year data. Int J Oral Maxillofac Implants.1997;12(3):319-324.
8. Levine RA, Rose L, Salama H. Immediate loading of root-form implants: two case reports 3 years after loading. Int J Periodontics Restorative Dent. 1998;18(4):333-343.
9. Ganeles J, Rosenberg MM, Holt RL, et al. Immediate loading of implants with fixed restorations in the completely edentulous mandible: report of 27 patients from a private practice. Int J Oral Maxillofac Implants. 2001;16(3):418-426.
10. Cooper LF, Rahman A, Moriarty J, et al. Immediate mandibular rehabilitation with endosseous implants: simultaneous extraction, implant placement, and loading. Int J Oral Maxillofac Implants. 2002;17(4):517-525.
11. Jaffin RA, Kumar A, Berman CL. Immediate loading of dental implants in the completely edentulous maxilla: a clinical report. Int J Oral Maxillofac Implants. 2004;19(5):721-730.
12. Ganeles J, Wismeijer D. Early and immediately restored and loaded dental implants for single-tooth and partial applications. Int J Oral Maxillofac Implants. 2004;19(Suppl):92-102.
13. Chiapasco M. Early and immediate restoration and loading of implants in completely edentulous patients. Int J Oral Maxillofac Implants. 2004;19(Suppl):76-91.
14. Jaffin RA, Kolesar M, Kumar A, et al. The radiographic bone loss pattern adjacent to immediately placed, immediately loaded implants. Int J Oral Maxillofac Implants. 2007;22(2):187-194.
15. Norkin FJ, Ganeles J, Sekler J, et al. Immediate loading of endosseous dental implants: a review of the evidence. Functional Esthetics and Restorative Dentistry. 2007;1(2):38-44.
16. Jaffin RA. Rehabilitating the failing dentition: full-arch immediate placement, immediate load therapy. Functional Esthetics and Restorative Dentistry. 2007;1(2):46-52.
17. Jokstad A, Carr AB. What is the effect of time-to-loading of a fixed or removable prosthesis placed on implant(s)? Int J Oral Maxillofac Implants. 2007;22(Suppl):19-48.
18. Morton D, Jaffin R, Weber HP. Immediate restoration and loading of dental implants: clinical considerations and protocols. Int J Oral Maxillofac Implants. 2004;19(Suppl):103-108.
19. Spear FM. It's all about relationships. Advanced Esthetics and Interdisciplinary Dentistry. 2005;1:1.
20. Cochran D, Oates T, Morton D, et al. Clinical field trial examining an implant with a sand-blasted, acid-etched surface. J Periodontol. 2007;78(6):974-982.
21. Rupp F, Scheideler L, Olshanska N, et al. Enhancing surface free energy and hydrophilicity through chemical modification of microstructured titanium implant surfaces. J Biomed Materials Res A. 2006;76(2):323-334.
22. Lang NP, Araujo M, Karring T. Alveolar bone formation. In: Lindhe J, Karring T, Lang NP, eds. Clinical Periodontology and Implant Dentistry. 4th ed. Oxford, UK: Blackwell Munksgaard; 2003:886-896.
23. Schwarz F, Herten M, Sager M, et al. Histological and immunohistochemical analysis of initial and early osseous integration at chemically modified and conventional SLA titanium implants: preliminary results of a pilot study in dogs. Clin Oral Impl Res.2007;18(4):481-488.
24. Buser D, Broggini N, Wieland M, et al. Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res. 2004;83(7):529-533.
25. Levine RA, Auty C, Keller W, et al. How can surface technology help you grow your practice? Presented at: Academy of Periodontology Annual Meeting; October 27-30, 2007; Washington, DC.
26. Morton D. Clinical results with the SLActive surface in a 2-center study. Presented at: International Team for Implantology World Symposium; June 18-20, 2005; Munich, Germany.
27. Levine RA, Makrauer Z, Burns R. SLActive and immediate loading: decreasing time while increasing confidence. Starget. In press.
28. Piattelli A, Corigliano M, Scarano A, et al. Immediate loading of titanium plasma-sprayed implants: a histologic analysis in monkeys. J Periodontol. 1998;69(3):321-327.
29. Testori T, Szmuckler-Moncler S, Francetti L, et al. Healing of Osseotite implants under submerged and immediate loading conditions in a single patient: a case report and interface analysis after 2 months. Int J Periodontics Restorative Dent. 2002;22(4):345-353.
30. Levine RA, Wilson TG. Compliance as a major risk factor in periodontal disease progression. Compend Contin Educ Dent. 1992;13(12):1072-1076.
31. Mealy BL. Commentary: managing patients with diabetes: first, do no harm. J Periodontol. 2007;78(11):2072-2076.
32. Nibali L, D'Aiuto F, Griffiths G, et al. Severe periodontitis is associated with systemic inflammation and a dysmetabolic status: a case-control study. J Clin Periodontol. 2007;34(11):931-937.
33. Lalla E. Periodontal infections and diabetes mellitus: when will the puzzle be complete? J Clin Periodontol. 2007;34(11):913-916.
34. Moy PK, Medina D, Shetty V, et al. Dental implant failure rates and associated risk factors. Int J Oral Maxillofac Implants. 2005;20(4):569-577.
35. Levine RA, Shanaman RH. Translating clinical outcomes to patient value: an evidence-based treatment approach. Int J Periodontics Restorative Dent. 1995;15(2):186-200.
36. Nevins M, Camelo M, De Paoli S, et al. A study of the fate of the buccal wall of extraction sockets of teeth with prominent roots. Int J Periodontics Restorative Dent. 2006;26(1):19-29.
37. Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for im-plant site development: a clinical and histologic study in humans. J Periodontol. 2003;74(7):990-999.
38. Ottoni JM, Oliveira ZF, Mansini R, et al. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants. 2005;20(5):769-776.
39. Molly L. Bone density and primary stability in implant therapy. Clin Oral Implants Res. 2006;17(Suppl 2):124-135.
40. Vercellotti T. Piezoelectric surgery in implantology: a case report—a new piezoelectric ridge expansion technique. Int J Periodontics Restorative Dent. 2000;20(4):359-365.
41. Vercellotti T, Nevins ML, Kim DM, et al. Osseous response following resective therapy with a Piezosurgery. Int J Periodontics Restorative Dent. 2005;25(6):543-549.
42. Vercellotti T, Pollack AS. The new bone surgery device: sinus grafting and periodontal surgery. Compend Contin Educ Dent. 2006;27(5):319-325.
43. Thomas J. Piezoelectric bone surgery: What is it? How does it work? Do I need it? Implant Realities. 2007;1:10-12.
44. Levine RA, Horowitz RA. Bone reconstructive surgery for implant site preparation. Functional Esthetics and Restorative Dentistry. 2007;1(2):20-28.
45. Rossein KD. Teaming up for successful implant dentistry. Functional Esthetics and Restorative Dentistry. 2007;1(2):12-14.
46. Ruskin J. Medical risk factors with an update on bisphosphonates. Presented at: International Team for Implantology World Symposium; April 26-28, 2007; New York, NY.
47. Karoussis, IK, Muller S, Salvi GE, et al. Association between periodontal and peri-implant conditions: a 10-year prospective study. Clin Oral Implant Res. 2004;15(1):1-7.