Tissue Management in Restorative Dentistry
J. William Robbins, DDS, MA
Abstract
Despite an increased emphasis on the perio-restorative interface in restorative dentistry, many clinicians have been unable to utilize the concept of biologic width in a practical manner. This article will describe an approach for diagnosing four categories of biologic width—Normal Crest, High Crest, Low Crest Stable, and Low Crest Unstable—using the procedures of bone sounding and sulcus probing. Treatment strategies for each category are also suggested.
In recent years, there has been an increased emphasis on the perio-restorative interface in restorative dentistry. During past decades, the restorative dentist has acknowledged the importance of biologic width. However, due to the lack of a truly operational definition, clinicians have been unable to utilize the concept of biologic width in a practical manner.
In 1961, Gargiulo et al1 published their now classic data on attachment measurements. They reported the mean measurement of epithelial attachment plus connective tissue attachment was 2.04 mm. In 1977, Ingber et al2 described “Biologic Width” and credited D. Walter Cohen for first coining the term. This measurement was repeated over and over again in the dental literature until the restorative dentist forgot that this number was an arithmetic mean, and not an actual patient. This led to four decades of an erroneous belief about the perio-restorative interface.
Based on the conventional definition of biologic width, it was impossible to explain why three different patients receiving crowns would have different gingival reactions. In one patient, the tissue around the crown would be healthy and exhibit long-term stability (Figure 1 and Figure 2). In a second patient, there would be chronic inflammation around the crown (Figure 3 and Figure 4). Finally, a third patient would experience gingival recession around the crown (Figure 5 through Figure 7). The inability to predict or understand the gingival response to a crown was frustrating for the restorative dentist. However, in the mid 1990s, Kois published his classic papers on biologic width.3,4 He proposed three categories of biologic width based on the total dimension of attachment plus the sulcus depth.
Categories of Biologic Width
In order to operationally define biologic width, Kois suggested that the restorative dentist must determine the total distance from the gingival crest to the alveolar crest. This procedure is termed bone sounding. The patient is anesthetized and the periodontal probe is placed in the sulcus and pushed through the attachment apparatus until the tip of the probe engages alveolar bone (Figure 8). Based on this measurement, the three categories of biologic width he described are Normal Crest (Figure 9), High Crest (Figure 10), and Low Crest (Figure 11). The measurements are made on anterior teeth mid-facially and at the facial/interproximal line angles.
Normal Crest Patient
In the Normal Crest patient, the mid-facial measurement is 3.0 mm and the proximal measurement is a range from 3.0 mm to 4.5 mm (Figure 9). Normal Crest occurs approximately 85% of time. In this patient, the gingival tissue tends to be stable long term. The margin of a crown should generally be placed no closer than 2.5 mm from alveolar bone. Therefore, a crown margin which is placed 0.5 mm subgingivally tends to be well-tolerated by the gingiva and is stable long term in the Normal Crest patient.
High Crest Patient
In the High Crest patient, the mid-facial measurement is less than 3.0 mm and the proximal measurement is also less than 3.0 mm (Figure 10). In this patient, it is commonly not possible to place an intracrevicular margin because the margin will be too close to the alveolar bone, resulting in a biologic width impingement and chronic inflammation. High Crest is an unusual finding in nature and occurs approximately 2% of the time. There is one area where High Crest is seen more often: in a proximal surface adjacent to an edentulous site. If a tooth is removed and the interproximal papilla is not supported, it will collapse, commonly resulting in a High Crest situation.
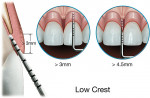
Low Crest Patient
In the Low Crest patient group, the mid-facial measurement is greater than 3.0 mm and the proximal measurement is greater than 4.5 mm (Figure 11). Low Crest occurs in nature approximately 13% of the time. Traditionally, the Low Crest patient has been described as more susceptible to recession secondary to the placement of an intracrevicular crown margin. When retraction cord is placed subsequent to the crown preparation, the attachment apparatus is routinely injured. As the injured attachment heals, it tends to heal back to a Normal Crest position, resulting in gingival recession.
Low Crest, Stable or Unstable
However, the Low Crest attachment is actually more complex because all Low Crest patients do not react the same to an injury to the attachment. Some Low Crest patients are susceptible to gingival recession while others have a quite stable attachment apparatus. The difference is based on the depth of the sulcus, which can have a wide range.1,5
For example, patient A (Figure 12) is bone sounded and the mid-facial distance from the gingival crest to the alveolar crest is 5.0 mm. Patient B (Figure 13) is bone sounded and the measurement is again 5.0 mm. By definition, both of these patients are Low Crest. However, they are not the same. Patient A has a 3.0-mm sulcus and a 2.0-mm attachment (ie, epithelium and connective tissue). In contrast, Patient B has a 1.0-mm sulcus and a 4.0-mm attachment (ie, epithelium and connective tissue).
Patient A has 3.0 mm of unsupported tissue from the base of the sulcus to the gingival crest. This amount of unsupported gingival tissue does not tend to be stable, and this patient is susceptible to gingival recession. However, Patient B has a more substantial attachment apparatus (4.0 mm) and a significantly shallower sulcus (1.0 mm). This patient is much less susceptible to gingival recession. Patient A is classified as an Unstable Low Crest because the patient is more susceptible to gingival recession. Patient B is classified as a Stable Low Crest because this patient reacts more like a Normal Crest patient and is not as susceptible to gingival recession.
In order to diagnose a Low Crest patient as Stable or Unstable, the dentist must perform sulcus probing in addition to bone sounding. It is well known that sulcus probing is an inexact art.6 There are several variables in sulcus probing, including probe diameter, probing force, angle of the probe, and amount of inflammation in the attachment. However, a determination of sulcus depth is necessary to determine if a Low Crest patient has a tendency to be long-term Stable or Unstable in the face of an insult to the attachment.
Importance of Determining the Crest Category
When preparing anterior teeth for indirect restorations, it is essential that the dentist know the Crest category. This allows the operator to determine the optimal position of margin placement, as well as inform the patient of the probable long-term effects of the crown margin on gingival health and esthetics. For example, if bone sounding reveals a Normal Crest situation, the dentist can place an intracrevicular margin that is no closer than 2.5 mm to the alveolar crest, with a reasonable expectation of long-term gingival health and esthetics. If bone sounding reveals a High Crest situation, the dentist knows that the placement of an intracrevicular margin will likely result in chronic inflammation secondary to impingement on the biologic width. If bone sounding reveals a Low Crest situation, the dentist must also determine the sulcus depth.
If the sulcus is in the shallow range, the dentist may treat this Stable Low Crest patient like a Normal Crest patient. An intracrevicular margin can be placed with a reasonable expectation of long-term stability and esthetics. However, if the sulcus is in the deeper range, the dentist would expect that an intracrevicular crown margin placed in this Unstable Low Crest patient would result in gingival recession.
The periodontal surgeon must also be aware of the crest position prior to performing esthetic crown lengthening in the patient with altered passive eruption. In order to diagnose altered passive eruption, two criteria must be met.7 First, the tooth is short by measurement (ie, normal length of a central incisor is between 10.0 mm and 11.0 mm).8 Second, the dentist cannot feel the cementoenamel junction (CEJ) in the sulcus. If both of these criteria are met, a diagnosis of altered passive eruption is made and the surgeon can be confident that there is a significant amount of enamel that is covered by the gingiva (Figure 14).
The goal of esthetic crown lengthening is to surgically expose most of the anatomic crown without exposing the root surface. At the completion of the procedure, the CEJ should not be visible, but should be palpable with an explorer in the sulcus. In order to achieve these goals, a facial full-thickness flap is reflected, leaving the interproximal tissue intact (Figure 15). Using rotary (Figure 16) and hand instruments (Figure 17), the alveolar bone is then moved 2.0 mm apical to the CEJ from line angle to line angle. The facial alveolar bone is recontoured and thinned (Figure 18), and the tissue is repositioned and sutured so that the gingival crest is 3.0 mm from the alveolar crest. In most patients, the tissue will heal at this new position and remain stable long term (Figure 19).
However, the Stable Low Crest patient requires more than 3.0 mm from the gingival crest to the alveolar crest because of his/her unique requirement for a longer attachment apparatus. If the bone is moved 2.0 mm apical to the CEJ and the gingival crest is placed 3 mm from the alveolar bone, as is usually done, the tissue will not remain where it was placed and will rebound in the Stable Low Crest patient (Figure 20, Figure 21, Figure 22). Therefore, the surgeon must be aware of the crest position and stability type prior to surgery. If the patient is Stable Low Crest, the distance from the CEJ to the alveolar bone must be greater than the traditional 2.0 mm in order to attain long-term stability of the position of the tissue.
Conclusion
It has been the purpose of this article to describe a current approach to the diagnosis of biologic width using the procedures of bone sounding and sulcus probing. Four categories of biologic width—Normal Crest, High Crest, Low Crest Stable, and Low Crest Unstable—have been described. In addition, treatment strategies for each category of biologic width have been suggested.
Acknowledgement
The author thanks John Bonfardeci for his assistance in the preparation of this manuscript.
References
1. Gargiulo A, Wentz F, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32:261-267.
2. Ingber JS, Rose LF, Coslet JG. The "biologic width" – a concept in periodontics and restorative dentistry. Alpha Omegan. 1977;70:62-65.
3. Kois J. Altering gingival levels: The restorative connection, Part 1: Biologic Variables. J Esthet Dent. 1994;6:3-9.
4. Kois JC. The restorative-periodontal interface: biological parameters. Periodontol 2000. 1996;11:29-38.
5. Vacek JS, Gher ME, Assad DA, et al. The dimensions of the human dentogingival junction. Int J Periodontics Restorative Dent. 1994;14:154-165.
6. Weisgold AS. Contours of the full crown restoration. Alpha Omegan. 1977;70:77-89.
7. Dolt AH, Robbins JW. Altered passive eruption: an etiology of short clinical crowns. Quintessence Int. 1997;28:363-372.
8. Gillen RJ, Schwartz RS, Hilton TJ, et al. An analysis of selected normative tooth proportions. Int J Prosthodont. 1994;7:410-417.
About the Author
J. William Robbins, DDS, MA
Clinical Professor
University of Texas Health Science Center at San Antonio Dental School
San Antonio, Texas
Private Practice
San Antonio, Texas