How Clinicians Can Facilitate Predictable Outcomes with Shade Selection for Indirect Restorations
Luke S. Kahng, CDT
Abstract
Difficulties with custom shade matching occur whether prescribing single- or multiple-unit restorations. Despite subjective factors that could contribute to shade discrepancies between what the patient/clinician expect and what the technician delivers, the use of a checklist that outlines what to do and provide during the communication and restoration prescription process can help ensure predictable outcomes when treatment planning indirect restorations. This article provides a step-by-step to-do list for clinicians to facilitate the custom shade matching process.
Introduction
When the dental technician is given a work slip that says, “Tough shade; you’ll need to see the patient for a custom color,” most often the struggle results from a single anterior tooth, but sometimes it can occur with multiple units, too. The difficulty can be that the technician’s perception of the requested color is different from what the patient and clinician see. Without a strategy for color matching, everyone involved can become frustrated and discouraged when the shade of the restoration does not look as intended. The truth is that custom shade taking is an art, and there is always something new to learn.
This article examines a number of factors that may hinder the selection of a proper color match. Subjective faults can range from differences in color perceptions to ocular fatigue. However, with a practical plan and goal from the outset, as well as a checklist to follow, the custom shade matching process for indirect restorations can be simplified and the results more successful. In the same manner that we plan for quality control by using standards for double-checking our work, we can give ourselves a method to double check the custom shading process. The following outlines a to-do list to help ensure accurate custom shade matching.
1. Select Surface and Texture
Technicians must make sure that the surface texture will match after they apply natural glaze to the finished restoration. A young person’s teeth tend to look coarse (Figure 1 and Figure 2), while an older patient’s surface texture may be considered “medium” (Figure 3 and Figure 4). However, an older patient may also present with a glossy “before” surface texture that should also be replicated in the final restoration (Figure 5 and Figure 6). Therefore, it would be helpful if clinicians provide their laboratory technicians with their description of teeth’s surface texture.
2. Determine the Value
Technicians must understand clear and enamel dentin segmentation. When technicians build up the dentin and then cut it back, the technique they use is very important. If they cut back too much, they will need to replace it with enamel (clear) in order to create low value. If they do not cut back, they will produce a restoration with high value due to the dentin color. When submitting your custom prescription, be sure to indicate what the value of the shade is.
The value of a color is defined by the amount of white light that is absorbed or reflected. A tooth high in value is bright and vital in appearance. A low value tooth is gray and will appear less vital. Value is the only dimension of color that may exist alone (Figure 7, Figure 8 and Figure 9).
3. Determine Hue
Hue is the intensity of a color (eg, red, blue, green), but white, gray, and black do not possess any hue. Chroma is the amount of saturation or strength of a hue. For example, a certain red and a certain pink may have the same hue. However, the red may have a stronger saturation of hue and, therefore, a higher chroma. The pink is really a diluted red and has a low chroma.
So, what color is the tooth? Technicians must learn to utilize enamels effectively in order to correctly cover the restoration’s surface. Does it need stain? This may help to define the hue. When providing your custom shade description, be sure to determine the hue and any related characteristics.
4. Identify Where the Tooth is Translucent or Transparent
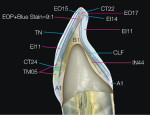
Divide the tooth into seven segments to determine where it’s translucent or transparent, as well as by how much (Figure 10, Figure 11 and Figure 12). A shade mapping guide will facilitate this process and help you chart the colors and determine areas of translucency and transparency. Be sure to share this with your technician, in addition to why you think the translucencies exist.
If technicians check the dentin and color on the inside of the tooth, they may find that it changes the translucency. This leads to overlaying color on the inside of the restoration. Technicians must understand the porcelain powders they are using and what roles they will play in the “look” of a restoration, something that becomes easier with experience.
5. Document the Stump Shade
Always check the stump shade, especially with a complex case, in order to ensure the best material selection (Figure 13 and Figure 14). A dark stump shade color will result in show-through and alter the appearance of the final restorative shade. The use of one universal shade tab is preferable over a different shade tab for every type of material. Technicians can then be certain that the same translucency modifier, enamel effects, enamel opals, enamel occlusion colors, and/or cervical translucencies will work for all types of restorations. You can document the stump shade in writing and also photographically.
6. Observe and Communicate Symmetry Reflection/Tooth Morphology Characteristics
Surveying natural teeth reveals information about symmetry and answers questions about emergence profile from the gingival level. Are the teeth concave or convex? Which areas show reflection?
The finished restorations must demonstrate the same symmetry reflection as the teeth they border. Therefore, clinicians and technicians must always study the adjacent teeth. The cast model is the beginning of this process and shows the direction in which technicians should go. Natural teeth have at least 10 to 12 colors; their restorations will sometimes require as many as 18. If technicians do not recognize the tooth’s frame design, they may add too many porcelain layers, resulting in a restoration that appears too lustrous due to porcelain shrinkage during the baking process.
7. Suggest Your Selected and/or Preferred Restorative Material
There is a multitude of indirect restorative material choices available today, and clinicians are encouraged to discuss the benefits and limitations of each with their laboratory technicians. For the purposes of determining custom shades, it’s important to recognize how each material’s optical properties may affect the desired esthetic outcomes. Pressed ceramics have made all-ceramic, metal-free restorations popular (Figure 15, Figure 16, Figure 17). However, it is possible to produce an esthetic result with the placement of a restoration fabricated using a non-oxide metal (Figure 18).
An initial material component of pressed ceramics was leucite, which has been used in veneers and crowns based on its translucent quality. Today, for crowns and bridges, these pressed ceramics have been enhanced by the stronger lithium disilicate component, although it is not as translucent.
Alternatively, zirconia is another metal-free material available from many manufacturers that is beneficial because it can be used in a variety of computer-aided design/computer-aided manufacturing (CAD/CAM) systems. With strength rivaling metal, zirconia appears very low in translucency and demonstrates higher opacity. Before zirconia there was alumina and it, too, was low in translucency, with only moderate opacity.
In the area of metal-ceramics, a composite gold materialc that doesn’t oxidize—according to the manufacturer—demonstrates a warm gold color that enhances the appearance of porcelain. Because it is a non-oxidizing metal, it produces no oxide show-through commonly observed with oxidizing metals.
8. Note any Mamelons or Craze Lines
Each patient may present with unique tooth characteristics that can affect the manner in which shades are perceived. Therefore, it’s important for clinicians to note any mamelons or craze lines that are perceived to potentially influence the appearance of the tooth color (Figure 19, Figure 20, Figure 21).
9. Take Photographs
The camera—either a digital or instant Polaroid model—has become important to dentists and technicians because it allows evaluation of tooth color, craze lines, stains, surface texture, and luster. Multiple pictures should be taken at different angles and under different lighting conditions to facilitate the best matching results. Provide these images to the laboratory so that the technician can develop a true sense of what the patient’s teeth look like. Computers have also become valuable communication tools. If clinicians take photographs with an intraoral camera, they can be sent immediately to another location via the internet. The film development step is eliminated, which translates into a savings of time and money.
However, digital photography and computers do not solve all of the problems of shade selection. Photographs need to be taken with shade tabs in the picture, preferably held at 90° to the tooth (ie, perpendicular) for best results so that there will be no reflection. The shade tab provides a definite guide to the shade and color changes from different computer monitors and printers, since one office monitor may show a completely different color than another. The same can be said of printers. A laser printer is different from an inkjet printer, but a color difference can be observed among various laser printers, also.
10. Communicate
Communication among the clinician, technician, and patient facilitates the best outcome. Additionally, the use of my anterior/ posterior characterization guide (Figure 22) provides a common ground for the clinician and patient during conversations about anticipated restorative outcomes. Finally, it may also be helpful to provide the patient with my smile selection book for use in making choices about his or her final smile appearance and/or shade (Figure 23).
Matching Composite Resins
Composites have changed dramatically in recent years in terms of their physical and mechanical properties. An indirect composited can be a material of choice to create a life-like and durable esthetic restoration. The colors presented by the different composite manufacturers give dental technicians the ability to apply the similar layering techniques that are utilized in porcelain powder build-ups. A good technician can apply advanced layering techniques using composites to create a highly esthetic restoration.
Conclusion
If dental professionals have different tools at their disposal—a photograph, a shade map, and a checklist—they can approach shade selection with confidence. You will feel better about the outcome of your work, and patients will feel secure that they’re in good hands. The patient will sense that the clinician and the technician will meet their expectations.
Also, in this author’s opinion, if the patient wants “best of the best” shade matching, one full day’s appointment is recommended. This should include viewing the patient in different lighting situations, eating lunch together, and getting to know the patient’s lifestyle and habits. The technician can make different understructures and the different copings can be prepared from all the different information. The different restorations can be tried in the patient’s mouth, enabling a final decision about shade selection to be made at that time.
a Zirconium Oxide Ceramic, Etkon USA, Arlington, TX
b GC America, Inc., Alsip, IL
c Captek™, Precious Chemicals Company, Inc., Altamonte Springs, FL
d Tescera ™, Bisco, Inc., Schaumburg, IL
About the Author
Luke S. Kahng, CDT
Owner, Capital Dental Technology Laboratory, Inc.
Naperville, Illinois