Guidelines for the Selection and Application of Intracoronal Restorations
Douglas A. Terry, DDS; Cynthia P. Trajtenberg, DDS, MS; Karl F. Leinfelder, DDS, MS
Abstract
This article will discuss the use of direct and indirect composite and ceramic restorative systems for posterior intracoronal restorations, as well as such influences on their application as operator skill, experience, and clinical judgment. The authors offer a discussion of the consideration factors for their use and comparison of the properties and capabilities of each system that enable proper case selection by the patient, technician, and restorative dentist.
Technological advancements driven by dental material research have provided the restorative dentist with myriad opportunities to apply significant developments in material science and adhesive technology to the treatment process. The utilization of direct and indirect systems for the intracoronal restoration of posterior teeth has increased dramatically with the improvements in physical and mechanical properties of these systems and patient demand for tooth-colored restorations. Direct composite resin restorations and laboratory processed inlays fabricated with composite resin or porcelain represent esthetic restorative solutions for intracoronal restorations. Modern adhesive restorative materials and techniques allow preservation and reinforcement of remaining tooth structure and conservation of tooth structure during preparation, while improving the longevity and esthetics of the restoration. Each of these systems (i.e. direct, indirect composite and ceramic) can provide precise marginal integrity, ideal proximal contacts, wear resistance similar to tooth structure, reduced polymerization shrinkage, excellent anatomical morphology, optimal esthetics, and the ability of being conditioned to increase adhesive strength,2 Based on these premises, these intracoronal restorative systems can provide predictable clinical results. The authors offer a discussion of the consideration factors for their use and comparison of the properties and capabilities of each system that will enable proper case selection by the patient, technician, and restorative dentist.
Direct Intracoronal Restorations
As patients seek conservative treatment that is more biocompatible, durable, safe, and esthetic, increased utilization of direct composite resin materials for the restoration of the posterior dentition has drawn more attention to the technological advances in the dental profession. In the past, use of composite resins in the posterior area was limited due to low wear resistance to abrasion, shade instability, increased polymerization shrinkage, low compressive and flexural strength, and a high incidence of fracture. Therefore, the placement of these direct systems was limited to smaller restorations. Newer formulations of enhanced filler size, geometry, composition, and concentration have significantly improved the physical, mechanical, and optical properties of these resin systems and increased their use in medium to larger restorations. However, there are several consideration factors for the utilization of direct composite resin in medium to larger restorations. These include polymerization shrinkage, cavity dimension, anatomical morphology, and financial constraints of the patient. Each will be discussed below.
A. Polymerization Shrinkage
When using composite resins in a direct restorative procedure, the monomer polymerization shrinkage depends on both the filler loading and the percentage of conversion. This leads to a significant volumetric change. Shrinkage stress may not be well offset by adhesive systems and contributes to postoperative challenges, such as inadequate marginal adaptation, microleakage, marginal breakdown fractures, secondary caries, marginal staining, pulpal irritation, postoperative sensitivity, and possible need for endodontic therapy.3,4
To overcome these negative clinical challenges of direct resin composite materials, several methods can be considered for the reduction of polymerization stress. These include application of adhesive liners or base materials that act as shock absorbers, selection of curing techniques (eg, light intensity layering )5 according to the configuration factor or “C-factor,” appropriate use of adhesive systems, incremental layering of small amounts of composite resin, and selection of contemporary nanoparticle, low-shrinkage composite resin systems.6
B. Cavity Dimension
Tooth preparation for direct composite restorations differs from the indirect fabricated inlay/onlay. The direct composite preparation design preserves as much sound tooth structure as possible and requires no extension for resistance. The preparation is limited to the access and removal of infected/affected tissue and pre-existing defective restoration and requires less volume of material to resist clinical fracture than a metallic restoration (i.e. amalgam) or laboratory processed inlay (i.e. composite or ceramic). The cavity dimension for medium to large occlusal and approximal cavity preparations for direct composite restorations can be more conservative than laboratory fabricated restorations because the preparation does not require the removal of undercuts for proper path of insertion and adaptation to the cavity walls. In addition, the direct placement method can be used with minimal preparation because it uses the undercuts and surface irregularities to increase the macro- and micro-retentiveness for bonding.
C. Anatomical Morphology
In the past, clinicians encountered difficulty in achieving precise marginal integrity, ideal proximal contacts, and anatomical contours for large cavity preparations. Advances in proximal contouring devices (i.e. sectional matrices) and improved sculptability of the all-purpose, microhybrid composites have complemented incremental layering techniques (i.e. horizontal, vertical, and oblique layering techniques) and light curing methods (i.e. three-sited light-cure method). This has resulted in improved proximal contact, elimination of overhangs, ideal tooth contours, minimizing or eliminating excess resin at the proximal line angles, improved marginal integrity, a reduction in microleakage at the susceptible gingival margin, and simplification of occlusal adjustments and finishing procedures.7
D. Financial Constraints of the Patient
There are clinical situations in which patients desire tooth-colored restorations but are financially unable to accept the clinician’s ideal recommendations (i.e. indirect inlays/onlays or porcelain crowns). These larger occlusal and approximal cavity preparations can be restored with the aforementioned stress reduction techniques and the optional use of reinforcement fibers as transitional restorations. The transitional restoration is defined as one that will serve as an intermediate procedure, but which has the potential for longevity in specific clinical situations (i.e. areas of low occlusal stress and where there is minimal potential of tooth flexure).
From the wide range of restorative biomaterials available, direct composite resin systems provide an esthetic alternative for intracoronal posterior restorations. Their primary attributes include that they require only single-appointment procedures; no impressions or provisionals are required; and the operator has total control of the restorative process and the esthetic outcome, since the surrounding dentition serve as comparisons.
Indirect Intracoronal Restorations
The aforementioned consideration factors should be reviewed for the utilization of laboratory fabricated inlays/onlays in medium to larger restorations, also. Because laboratory processed inlays and onlays are fabricated on a model, the polymerization shrinkage can be controlled outside the micropreparation, and the amount of shrinking material is minimal, involving the cementing interface. The cavity preparation requires the removal of tooth structure (i.e. undercuts) for proper path of insertion and adaptation of the restoration to the cavity walls, as well as for ease of insertion and removal during fabrication.
The cavity dimension includes medium to large preparations and provides an alternative solution for consideration for cuspal coverage (i.e. onlay) when the isthmus preparation exceeds one half of the distance from the central fossa to cusp tip. The anatomical morphology details and occlusion can be controlled to a higher level on the laboratory model and with the use of a microscope. In addition, the surface finish of the proximal surfaces can be polished to a higher degree and can provide an ideal contour and a positive contact. However, these indirect restorations require two appointments and a larger financial investment by the patient.
Both direct and indirect restorative systems can provide precise marginal integrity, ideal proximal contacts, wear resistance similar to tooth structure, reduced polymerization shrinkage, excellent anatomical morphology, and optimal esthetics.1,2 Therefore, because both of these restorative systems can provide predictable clinical results, a comparison of the attributes and capabilities of processed composites vs. porcelain will enable proper case selection by the patient, technician, and restorative dentist.
Laboratory Processed Composite vs. Ceramic
Factors that should be considered to ensure a proper clinical case outcome when selecting ceramic or processed composite resin restorations include:
- material with optimal mechanical properties for the posterior dentition
- stable optical properties
- wear compatibility with natural tooth structure
- preservation of cavosurface margins
- acceptable thermal expansion coefficient and dimensional stability
- chairside structural and color modifications (eg, monochromatic vs. polychromatic changes)
- easy intraoral polishability
A. Physical and Mechanical Properties
Ceramic is a stiff and brittle material with a high elastic modulus. Therefore, this type of restorative material does not tolerate high levels of elastic deformation.2 Clinically, this can result in fracture of the ceramic margins at the try-in stage. Ceramic material has high compressive resistance and low tensional stress resistance.8,9,10 This represents a challenge for inlay preparations because these limited-size preparations do not provide tensile resistance. The flexural strength of second generation composite resins ranges from 120 MPa to 150 MPa, which is higher than that of feldspathic ceramic (i.e. 65 MPa). This slight elasticity of the composite resin helps absorb some of the strains, therefore protecting the adhesive bond at the tooth/restorative interface.2
B. Wear Compatibility
Porcelain is harder than tooth structure and, when not polished properly, has the potential to abrade natural teeth at an accelerated rate, whereas second generation laboratory composite resins are softer and exhibit more favorable wear compatibility with the opposing natural dentition.11,12
C. Cavosurface Margins
Porcelain margins have the potential for microchips at the tooth/restorative interface, whereas second generation laboratory composite restorations can be made with smaller gaps. These cavosurface margins in ceramic restorations have a propensity for fracture.13
D. Thermal Expansion
Composite inlays have excellent marginal integrity because of the similar thermal expansion rate as the luting cement. Conversely, there is a variation in coefficients of thermal expansion for porcelain inlays and the composite luting cement, resulting in an increase width of the luting gap.14
E. Chairside Modifications
Porcelain modifications (eg, contacts, fractured margins) are time-consuming at chairside, whereas indirect resin restorations can be easily modified chairside.15
F. Monochromatic vs. Polychromatic
Injectable ceramics are monochromatic and color can be altered with external stains that can be removed with occlusal adjustment or occlusal wear. Second generation composite resins can be internally layered for a polychromatic effect.
G. Impact Absorption
Composite materials have shown a greater capacity to absorb compressive loading forces and reduce the impact forces by 57% more than porcelain. Therefore, composite more uniformly distributes the applied load to the underlying structures (i.e. tooth, implant fixture, alveolar bone).16,17
H. Intraoral Polishability
Since the occlusion is equilibrated after cementation, the processed laboratory composite resin offers an advantage over porcelain because of its ease of intraoral polishability. It is more difficult to establish a highly polished surface intraorally on porcelain after the glaze has been removed by intraoral adjustments.11,18 This unpolished surface has been shown to increase wear of the opposing dentition and undergo color changes.13,19
Although laboratory processed composite resins provide important clinical advantages in many situations, there are several factors that should be considered for the use of porcelain intracoronal restorations. Those factors include the efficiency and ease of fabrication in the laboratory as a result of advanced technology [eg, injectable ceramics and computer-aided design/computer-aided manufacturing (CAD/CAM) systems], the availability of these systems in laboratories, and the technician’s expertise with this technology. Composite systems for CAD/CAM technology are not as common. In addition, porcelain systems are unsurpassed in stability of color, gloss, and wear resistance.
A review of the last decade of clinical studies of posterior restorations indicates that the annual failure rates in posterior stress-bearing restorations for these different systems are 0% to 9% for direct composites, 0% to 11.8% for composite inlays, 0% to 7.5% for ceramic restorations, and 0% to 4.4% for CAD/CAM ceramic restorations.20 However, the clinician should consider that improvement in the longevity of each of these restorations is not only influenced by material selection, but by numerous other factors that include restorative placement techniques, pulp protection, restorative finishing and maintenance, operator skill, and individual patient selection.
Clinical Application
The clinical success of a direct or indirect bonded restoration requires accomplishing function, esthetics, biocompatibility, and longevity.21 The attainment of these four criteria begins at the adhesive interface. A restorative material properly bonded to the enamel and dentin substrates will reduce marginal contraction gaps, microleakage, marginal staining, and caries recurrence; improve retention; reinforce tooth structure; and dissipate or reduce functional stresses across its interface throughout the entire tooth, while also improving natural esthetics and wear resistance.22
The objective of presenting each of the following three clinical cases is to provide the clinician with the fundamental concepts for preparation and placement of direct and indirect intracoronal posterior restorations.
Case #1
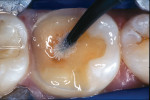
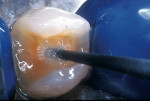
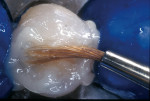
A patient presented with a defective composite restoration on the maxillary left first molar with recurrent decay (Figure 1). The treatment of choice involved a Class II preparation (Figure 2). After acid-etching the preparation, a light-cured adhesive was applied for 20 seconds with continuous motion, reapplied every five seconds, air-thinned for five seconds, and light-cured for 20 seconds (Figure 3). The direct composite resin increment was applied to the cavity wall with a ball-tipped instrument; an oblique layering technique was employed (Figure 4). The completed direct composite restoration demonstrated optimal marginal integration (Figure 5).
Case #2
A patient presented with a large composite resin restoration with recurrent decay on the mandibular right first molar (Figure 6). An indirect onlay preparation was completed (Figure 7). An adhesive agent was applied, air-thinned, and light-cured (Figure 8). Excess resin cement was removed with a sable brush (Figure 9). The postoperative view of the laboratory processed composite resin restoration revealed harmonious integration of the composite resin with the existing tooth structure (Figure 10).
Case #3
A patient presented with a fractured amalgam restoration with interproximal decay on the mandibular left second premolar (Figure 11). It was decided to treat the tooth with an indirect ceramic inlay, and the tooth was prepared accordingly (Figure 12). After acid-etching the preparation, a thin layer of adhesive was applied onto the primed surface with an applicator tip in two separate coats, air-thinned for 10 seconds, and light-cured for 10 seconds per surface (Figure 13). A sable brush was used to remove the excess resin cement; this left only a residual amount at the margin to compensate for polymerization shrinkage (Figure 14). The finished restoration exhibited harmonious integration of interproximal form and color. The marginal adaptation of the indirect ceramic restoration was evident (Figure 15).
Conclusion
Knowledge of the attributes and capabilities of each of these restorative systems can provide insight for their selection as an intracoronal restoration. However, material selection is only part of the restorative solution, since the application of these systems is influenced by the operator’s skill, experience, and clinical judgment. By integrating this knowledge with precise technical application of these restorative systems, dental professionals can complement and broaden the scope of the alternative restorative modalities that are available to assist the patient, technician, and dentist in making an informed decision in different clinical situations.
References
1. Howard NY. Advanced use of an esthetic indirect posterior resin system. Compend Contin Educ Dent. 1997;18:1044-1046, 1048, 1050.
2. Touati B, Aidan N. Second generation laboratory composite resins for indirect restorations. J Esthet Dent. 1997;9:108-118.
3. Davidson CL, Feilzer AJ. Polymerization shrinkage and polymerization shrinkage stress in polymer-based restoratives. J Dent. 1997;25:435-440.
4. Bausch JR, de Lange K, Davidson CL, et al. Clinical significance of polymerization shrinkage of composite resins. J Prosthet Dent. 1982;48:59-67.
5. Feilzer AJ, Dooren LH, de Gee AJ, et al. Influence of light intensity on polymerization shrinkage and integrity of restoration-cavity interface. Eur J Oral Sci. 1995;103:322-326.
6. Asmussen E. Composite restorative resins. Composition versus wall-to-wall polymerization contraction. Acta Odontol Scand. 1975;33:337-343.
7. Liebenberg WH. Successive cusp build-up: an improved placement technique for posterior direct resin restorations. J Can Dent Assoc. 1996;62:501-507.
8. Dietschi D, Maeder M, Meyer JM, et al. In vitro resistance to fracture of porcelain inlays bonded to tooth. Quintessence Int. 1990;21:823-831.
9. Binns D. The chemical and physical properties of dental porcelain. In: McLean JW, ed. Dental Ceramics: Proceedings of the First International Symposium on Ceramics. Chicago, IL: Quintessence Pub. Co.;1983:41-82.
10. Jones DW. The strength and strengthening mechanisms of dental ceramics. In: McLean JW, ed. Dental Ceramics: Proceedings of the First International Symposium on Ceramics. Chicago, IL: Quintessence Pub. Co.;1983:83-141.
11. Miller M. REALITY 2001. 15th ed. Houston, TX: REALITY Pub.
12. Burke FJ, Watts DC, Wilson NH, et al. Current status and rationale for composite inlays and onlays. Br Dent J. 1991;170:269-273.
13. Jagger DC, Harrison A. An in vitro investigation into the wear effects of unglazed, glazed, and polished porcelain on human enamel. J Prosthet Dent. 1994;72:320-323.
14. Fuhrer N. Restoring posterior teeth with a novel indirect composite resin system. J Esthet Dent. 1997;9:124-130.
15. Jackson RD. Aesthetic inlays and onlays: a clinical technique update. Pract Periodontics Aesthet Dent. 1993;5:18-27.
16. Gracis SE, Nicholls JI, Chalupnik JD, et al. Shock-absorbing behavior of five restorative materials used on implants. Int J Prosthodont. 1991;4:282-291.
17. Brunton PA, Cattell P, Burke FJ, et al. Fracture resistance of teeth restored with onlays of three contemporary tooth-colored resin-bonded restorative materials. J Prosthet Dent. 1999;82:167-171.
18. Lyons K. Alternatives to amalgam. N Z Dent J. 1997;93:47-50.
19. Magne P, Oh WS, Pintado MR, et al. Wear of enamel and veneering ceramics after laboratory and chairside finishing procedures. J Prosthet Dent. 1999;82:669-679.
20. Hickel R, Manhart J. Longevity of restorations in posterior teeth and reasons for failure. J Adhes Dent. 2001;3:45-64.
21. Pameijer CH, Grossman DG, Adair PJ. Physical properties of a castable ceramic dental restorative material. J Dent Res. 1980;59(1):474 (Abstract #827).
22. Goracci G, Mori G. Esthetic and functional reproduction of occlusal morphology with composite resins. Compend Contin Educ Dent. 1999;20:643-648.
About the Authors
Douglas A. Terry, DDS
Assistant Professor
Department of Restorative Dentistry and Biomaterials
University of Texas Dental Branch
Houston, Texas
Private Practice
Houston, Texas
Cynthia P. Trajtenberg, DDS, MS
Assistant Professor
Department of Restorative Dentistry and Biomaterials
The University of Texas Dental Branch
Houston, Texas
Karl F. Leinfelder, DDS, MS
Adjunct Professor
Department of Biomaterials Clinical Research
University of North Carolina–Chapel Hill
Chapel Hill, North Carolina
Professor Emeritus
University of Alabama School of Dentistry
Birmingham, Alabama