Maximum Custom Shade Matching for Laterals
Bring natural color back to life with the right material selection.
The patient presented with missing laterals that had been crowned many years previously. She had a very clear idea about what she wanted her teeth to look like, so she visited the author’s laboratory twice to discuss color, shape, and texture in order to make sure her teeth matched her expectations. Her old crowns were grey, and from a technician’s standpoint, it was going to be necessary to use the right material in order to match her natural dentition.
The author chose a B1 zirconia coping and matched her color in the laboratory setting. He noted some differences in the translucency/transparency between her canines and centrals. The central teeth had no mamelon, but there was a moderate lobe texture that would need to be recreated based on the maxillary teeth to result in a natural appearance and esthetically pleasing look. For the technician to match the laterals, he based his conclusions on the two central teeth, although he did not want to duplicate them exactly. Rather, he wanted to make the restorations slightly lighter, with a translucency modifier. The overall character of her color would therefore be lighter when the case was completed. Additionally, the canine translucency would also have a slightly lighter tone.
Some of the steps he took were to check the movement of the lateral and central teeth as well as the canine rise to determine the lateral incisal position. He then used a multilayered porcelain powder along with a zirconia coping. This article will demonstrate step-by-step porcelain layering techniques to build the final desired case.
The Case
Before preparation, the author took a photograph from the side of the lateral teeth (Figure 1), and another photograph was taken with a deep chamfer after preparation (Figure 2). The author used his own custom shade tabs to match the patient’s enamel two-thirds and gingival one-third color (Figure 3 through Figure 6). He also was able to match the surface texture of the natural dentition.
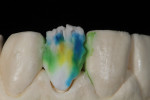
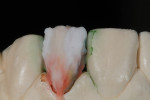
The zirconia copings for teeth Nos. 7 and 10 were placed on the cast model for a fit check (Figure 7). Ready for porcelain build-up, using the GC Initial ZR Porcelain System (GC America, www.gcamerica.com), the coping for tooth No. 10 was placed on the cast model (Figure 8). GC Initial ZR porcelain is pictured in Figure 9. The dentin and enamel opal colors were applied to the coping (Figure 10). Inside dentin color was then layered over that (Figure 11), followed by the enamel effective (Figure 13 and Figure 14). An application of enamel 59 was layered all the way to the gingival (Figure 15 and Figure 16).
Using articulating paper on the cast model, the technician performed a surface texture check. After firing, the surface texture markings were created based on negative and positive spacing (Figure 17). He simply followed the direction they provided when formulating the texture.
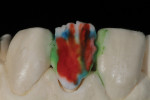
The technician then began to build up the restoration (Figure 18). He then applied regular dentin in A1 and translucency modifier 4 (Figure 19 and Figure 20). EOP4 was then applied (Figure 21 through Figure 23) followed by IN 44 (Figure 24 and Figure 25). Next, he applied an EOP1 layer over the IN 44 (Figure 26 and Figure 27). Immediately after, TM05 (Figure 28) was applied to the restoration followed by EN59 and 70 (Figure 29).
In order to make sure the texture matched the natural dentition, the author compared what he had created to that of the adjacent teeth (Figure 30). He then checked it against a mirrored image as a final restoration (Figure 31). On the cast model, with Renfert gold powder die spacer (Renfert, www.renfert.com), the technician checked the restorations again and found that he still needed to make some modifications (Figure 32). He applied GC Lustre Paste (GC America) staining LA to the gingival and incisal one-third area (Figure 33 and Figure 34). After the staining was completed, the clinician tried the restorations into the mouth to ensure that he had sufficiently mimicked her natural dentition (Figure 35). With different light sources, the technician checked the color balance and translucency (Figure 36 through Figure 39). Upon insertion, he noted good tissue response as well. The author then illustrated the lobe in comparison to the adjacent teeth for the readers (Figure 40).
The author created a pink, grey, and white Lustre paste mixture that best matched the patient’s existing dentition (Figure 41). He put a final touchup on tooth No. 10 in the bisque bake stage and then applied slightly more as needed (Figure 42).
In order to create color and texture, he applied a pink, grey, and white layer that matched the tone of the natural color (Figure 43 and Figure 44). For balance, he sought a slightly different color tone, as shown in immediately taken shots (Figure 45 and Figure 46). The author then checked the balance of the teeth, color, and surface texture during the final insertion (Figure 47 through Figure 49).
Conclusion
As mentioned, the technician looked carefully at his material selections for this specific situation, along with the stump color, and ordered his coping accordingly. He also took a close look at the opacity and translucency as well as the balance of color from the gingival to the incisal and body area. This also had to be compared to the canines and centrals in order to determine the correct amount of translucency.
Along with that, the author considered the texture between the teeth, the long axis, margin design, and the occlusion. All of these considerations led to success with his color shade matching, and more importantly, with his very happy and satisfied patient (Figure 50).
Acknowledgment
The author would like to thank Dr. Jack Manikowski of Lincoln Park Smiles in Chicago, Illinois, for presenting the case.
About the Author
Luke S. Kahng, CDT
Owner
LSK121 Oral Prosthetics
Naperville, Illinois