Simple Steps for Better Preparations
Tips to help dentist clients deliver better preparations for all-ceramic restorations.
By Gregg A. Helvey, DDS
As a dentist who became a laboratory technician, the author made many changes in the way he was practicing dentistry in order to keep the frustration level at the bench as low as possible. Although learning the continuously expanding techniques on the laboratory side of dentistry is enjoyable, some basic fundamentals for tooth preparations remain the same. Using these fundamentals has allowed the dentist to spend his time at the bench more productively, no longer wasting time searching for disappearing margins or trying to figure out what he had been thinking at the chair with an insufficient occlusal reduction situation.
This article will cover the types of burs that will help dentist clients create the ideal preparation, the finishing techniques that refine the preparation and provide better working models, and the immediate steps that clinicians can use to evaluate the preparation before taking the final impression.
All-ceramic anterior and posterior restorations, whether monolithic or bi-layered, are becoming more of the norm today. Many dentists still in practice started out with the ceramo-metal crown (PFM) as the workhorse restoration and are still influenced by its preparation parameters. This influence is reflected in the way many teeth are prepared, which is not always ideal for fabricating all-ceramic restorations.
Preparation parameters must be laid out in black and white to the dentist in order for the ceramist to produce a quality product. The old adage "garbage in… garbage out" really applies in this situation. Technicians can sometimes work miracles, but at other times, are forced to throw in the towel.
Prepping for All-Ceramic
The first area to address is the type of diamond bur that should be used for prepping all-ceramic restorations. All-ceramic restorations need to have a 90° exit angle.1 At the same time, the internal angle needs to be rounded.2 An appropriate bur would be a modified-shoulder diamond bur (Brasseler #6847 KR 018 or #8847 KR 016, www.brasselerusa.com), which allows for a rounded internal angle and a flat 90° exit angle. As with the use of any bur, a preparation glitch can happen, creating a trough or reverse margin. Often this occurs when the depth cut of the bur exceeds the diameter width at the tip. When the flat end leaves the outside wall of the tooth and is carried more internally, then a trough or edge is created on the margin. Many times, this reverse margin goes unnoticed until the impression is poured.
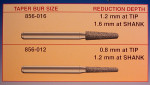
A simple solution is for clinicians to always use an end-cutting bur (SS White®, Piranha #10839 016, www.sswhiteburs.com) to finalize the margin or to select a bur size that corresponds to the desired preparation depth. Burs are measured at the widest part, which is at the hilt where the shaft and the diamond particles meet.3 The narrowest area is at the tip of the bur. A 018 taper-diamond bur, for example, measures 1.8 mm at the widest portion, but only 1.3 mm to 1.4 mm at the tip (Figure 1). Therefore, if the technician is asking for at least a 1.5-mm shoulder reduction, then a 018 size will need to be carried deeper into the tooth and off the marginal edge, which could possibly create a reverse margin. The alternative would be to advise the clinician to use a 021 size, which is 1.6 mm at the tip.
Finishing the Preparation
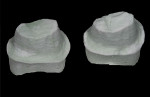
Using a carbide finishing bur after the gross reduction is completed will create a smoother surface and increase the wettability of the dentin.4 The smoother surface will be reflected in the surface of the working model die and create a more defined finish line (Figure 2 and Figure 3). If the clinician will be using a self-etching adhesive at the insertion appointment, studies have shown that a carbide finishing bur leaves a thinner smear layer that is more even in thickness over the dentin. The thicker the smear layer, the greater the buffering or neutralizing effect of the acid monomers in the self-etching resins.5 This results in less penetration of the adhesive. The deep grooves created by diamond burs can cause an uneven distribution of smear-layer debris, producing an uneven penetration by acidic resin monomers.6 One study showed a 33% increase in bond strength to dentin when a carbide bur was used compared to a diamond bur.7
Clinician Evaluation
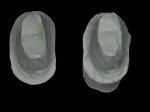
When viewing a single tooth or a number of prepared teeth intraorally, it is sometimes difficult to see undercuts, sharp line angles, or disappearing soft margins. This could be attributed to the fact that the prepared surfaces do not reflect light as well and details are hard to see. When a mirror is used to evaluate the preparation, there is no depth perception and trying to "eyeball" sufficient reduction is next to impossible. One way to counter this imposition is to fabricate a preview model by taking a quick alginate impression poured in Snap-Stone (Whip Mix Corp., www.whipmix.com). This gypsum product will set in 5 minutes. The clinician can then view the preparations, preferably under magnification, and determine if there are any inconsistencies to correct before the final impression (Figure 4 and Figure 5). The path of insertion and the angle of draw between abutments can also be evaluated for fixed partial dentures using this preview model. Areas to adjust can be marked in red and then brought to the patient for the correction.
One last suggestion would be to use an occlusal clearance tab (Figure 6). If clinicians could only sit on the tongue and look out, there would never be an under-reduced lingual cusp. But until that day happens, the use of a bite clearance tab works wonders. They are inexpensive and can be given as a gift or as a prize to accounts that have this problem and always try to make it the technician’s problem.
In summary, implementing these suggestions can change a laboratory technician’s day at the bench from frustrating to enjoyable. The overall winner, of course, is the patient, but the technician retains his heart muscle and stomach lining and the dentist provides an increased level of service.
References
1. McLaren EA, Vigoren G. Crown considerations, preparations, and material selection for esthetic metal-ceramic restorations. Esthetic Technique™: Clinical Case Studies and Technique Review. 2001;1(4):3-9.
2. Sorensen JA, Cruz M, Mito WT, et al. A clinical investigation on three-unit fixed partial dentures fabricated with lithium disilicate glass-ceramic. Pract Periodontics Aesthet Dent. 1999;11(1):95-106.
3. Priest G. Bur dimensions used to gauge porcelain veneer preparations. Dent Today. 2009;28(11):116,118,120.
4. Ayad MF, Johnston WM, Rosenstiel SF. Influence of dental rotary instruments on the roughness and wettability of human dentin surfaces. J Prosthet Dent. 2009;102(2):81-88.
5. Camps J, Pashley DH. Buffering action of human dentin in vitro. J Adhes Dent. 2000;2(1):39-50.
6. Barros JA, Myaki SI, Nör JE, et al. Effect of bur type and conditioning on the surface and interface of dentin. J Oral Rehabil. 2005;32(11):849-856.
7. Yiu CK, Hiraishi N, King NM, et al. Effect of dentinal surface penetration on bond strength of self-etching adhesives. J Adhes Dent. 2008;103):173-182.
About the Author
Gregg A. Helvey, DDS
Adjunct Associate Professor
Virginia Commonwealth University School of Dentistry
Richmond, Virginia
Private Practice
Middleburg, Virginia