Using Cone-Beam Computed Tomography and 3-Dimensional Implant Planning Software: The Restorative Dentist’s Role
James B. Wooddell, DDS; Joseph C. Passaro, DDS
Abstract:
It is the responsibility of the restorative dentist to be the architect of the comprehensive plan for the oral health of patients. This is especially true when implants are being considered as a treatment option, particularly in the esthetic zone. Successful therapies must include a complete understanding of the esthetic, functional, structural, and biologic needs of the patient. This article provides an overview of the recent advancements in 3-dimensional diagnostic and planning techniques, which provide the restorative dentist with unprecedented accuracy in the planning and delivery of successful implant dentistry.
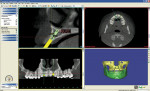
Cone beam computed tomography (CBCT) is a radiographic technique that records the density of the targeted area of the beam in three dimensions. This data is stored as a “digital imaging and communications in medicine” (DICOM) file. The acquired data require specialized software for viewing. Essentially, two types of software are used to manage the DICOM files: viewing software and interactive software. Viewing software assembles the data into 2- and 3-dimensional views of the imaged object and allows for height, width, density, and depth measurements. Interactive software performs the same functions as viewing software; however, in addition, it produces 3-dimensional volumetric renderings, which can be moved to view the imaged object from any perspective, allowing for virtual implant placement (Figure 1).
CBCT Use in Diagnosis and Treatment Planning
The challenge for the restorative dentist when evaluating a patient for treatment, particularly in the esthetic zone, is to analyze the patient’s current condition and compare it to a visualization of what the treatment outcome should be. In comparisons of the current and desired conditions, when a difference is noted, that difference represents the scope of treatment. Typically, the patient’s problems that have resulted in these differences represent a loss of structure, whether it is tooth, gingiva, or bone—all of which represent a loss of volume. These issues are 3-dimensional problems. Therefore, because CBCT represents a measurement of volume1 and allows 3-dimensional analysis, it can be surmised that CBCT is an efficient diagnostic tool to provide essential volumetric information for analyzing the patient’s physical presentation.
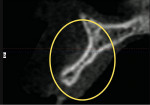
As an example, consider a patient who presents with congenitally missing lateral incisors. Clinical evaluation and a conventional radiograph (Figure 2) demonstrate what would appear to be adequate bone height for implant placement. Upon analysis of the CBCT image (Figure 3), a deficiency of bone volume is readily diagnosed, thereby providing essential information for the scope of treatment.
Of even greater value is when a patient is scanned while wearing an accurate provisional prosthesis of the desired definitive restorations, whether fixed or removable. Depending on the software’s requirements, these appliances can either be scanned separately or made of a radiopaque material that is seen on the CBCT. This process gives the restorative dentist the ability to visualize 3-dimensionally the existing bone and soft tissue relative to the desired tooth position (Figure 4).
Key Point
When combined with the thorough and precise use of classic diagnostic and restorative techniques to provide accurate information at the time of the CBCT scan, the restorative dentist is able to acquire the necessary data to determine the requirements for prosthetic success. The dentist is then able to lead the interdisciplinary team in a collaborative effort, establishing the correct treatment plan and sequence.2
Case 1
A 74-year-old female presented for mandibular posterior implants. A comprehensive examination and diagnosis was performed. The surgeon and restorative dentist decided because of the resorbed posterior mandibular ridge, guided implant placement would be the safest way to avoid inferior alveolar nerve damage.3,4 Provisional restorations were placed (Figure 5) to remove recurrent decay, open the vertical dimension, idealize the occlusion, and improve esthetics. At that point, a diagnostic wax-up of the mandibular posterior teeth was performed to determine their desired restorative positions before implant placement.
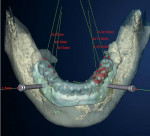
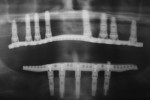
An overdenture scanning appliance (Figure 6) was fabricated and verified to fit the tissue. A CBCT scan was performed. Implant positions were determined relative to the desired prosthetic positions (Figure 7 and Figure 8). A surgical guide (NobelGuide™, Nobel Biocare, Göteborg, Sweden) was fabricated from the plan, and six implants were guided into position. Splinted screw-retained immediate provisionals were placed during surgery. All implants osseoin-tegrated successfully, and splinted definitive restorations were placed (Figure 9). Again, predictability was facilitated by using CBCT planning, but success was a result of proper diagnosis, planning, and interdisciplinary collaboration.
Case 2
A 73-year-old female presented with a hopeless dentition (Figure 10 and Figure 11). Preliminary impressions and interocclusal records were made and the casts mounted on an articulator in centric relation using a face-bow transfer. A full set of diagnostic photographs and a preliminary CBCT scan for volumetric analysis were taken. Treatment options were discussed, and it was determined that implant-supported maxillary and mandibular prostheses would be the desired treatment. The mounted casts and photographs were used to determine tooth position for ideal esthetics and occlusion. Tooth position and inclination, incisal plane, occlusal plane, and vertical dimension were all altered (Figure 12). Because changes in vertical dimension and tooth position require time to determine the adaptability of the patient, it was decided to approach implant therapy in stages.
The first phase of treatment involved fabricating an immediate maxillary complete denture and an immediate-load5,6 mandibular provisional prosthesis. The osseointegration period allowed time for assessment of the patient for esthetics, phonetics, and function. The patient was very comfortable with the new prostheses.
The patient’s maxillary denture was esthetically accepted (Figure 13) and in intimate contact with her tissues, and the occlusion was verified at the correct vertical dimension. Because the denture was an accurate and stable representation of the desired tooth positions in space, it was used as a scanning prosthesis for precise implant planning. A surgical template was fabricated from the virtual plan (Figure 14).
The laboratory technician fabricated a provisional prosthesis on a cast made from the surgical template. At surgery, the seating of the surgical template was verified and eight implants were placed through the template (Figure 15). The template was removed and the prosthesis placed directly on multi-unit transmucosal abutments, and the occlusion was verified. The definitive prosthesis (Figure 16, Figure 17 and Figure 18) was fabricated after osseointegration. Proper planning and restorative techniques before implant therapy provided a predictable path of prosthetic construction.
Conclusion
CBCT technology is one of the most promising tools in implant dentistry. Whether or not it is used to deliver implant fixtures through a computer-generated template, its volumetric information provides an additional dimension to diagnosis and treatment planning. It can help deliver accurate, functional, and esthetic results that enhance patients’ lives with techniques not previously possible. However, the technology cannot assume the restorative dentist’s roles of diagnosis and understanding basic restorative concepts such as vertical dimension, occlusion, and esthetic tooth position. It is the restorative dentist’s responsibility to be the architect and to lead the collaborative effort that is implant dentistry today.
References
1. Agbaje JO, Jacobs R, Maes F, et al. Volumetric analysis of extraction sockets using cone beam computed tomography: a pilot study on ex vivo jaw bone. J Clin Periodontol. 2007;34(11):985-990.
2. Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006;137(2):160-169.
3. Nickenig HJ, Eitner S. Reliability of implant placement after virtual planning of implant positions using cone beam CT data and surgical (guide) templates. J Craniomaxillofac Surg. 2007;35(4-5):207-211.
4. Sarment DP, Sukovic P, Clinthorne N. Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants. 2003;18(4): 571-577.
5. Misch CM. Immediate loading of definitive implants in the edentulous mandible using a fixed provisional prosthesis: the denture conversion technique. J Oral Maxillofac Surg. 2004;62(9 suppl 2):106-115.
6. Tarnow DP, Emtiaz S, Classi A. Immediate loading of threaded implants at stage 1 surgery in edentulous arches: ten consecutive case reports with 1- to 5-year data. Int J Oral Maxillofac Implants. 1997;12(3):319-324.
About the Author
James B. Wooddell, DDS
Joseph C. Passaro, DDS
Private Practice
Davidsonville, Maryland