Perio-Prosthetic Synergy in Implant Dentistry
Digitally merging surgical and prosthetic modalities leads to more predictable, esthetic outcomes
Bobby Birdi, DMD, MSc; Sundeep Rawal, DMD; and Sajid Jivraj, BDS, MSEd
During the last 10 years, dental implant therapy has progressed tremendously with regard to new innovations, techniques, and materials. This progression has taken place both on the surgical and prosthetic fronts and most importantly, with the development and utilization of digital technology. Many techniques, including guided surgery, immediate implant placement, soft- and hard-tissue augmentation, and immediate loading, have been developed and utilized in various applications with varying success and predictability. However, with the use of digital technology and workflow, it is now possible to combine multiple surgical and prosthetic modalities to begin with the end in mind and provide implant therapy in a streamlined, atraumatic manner.
Perio-prosthetic synergy begins by digitizing the patient prior to any therapy. When planning implant surgery, the use of cone-beam computed tomography (CBCT) technology alone is no longer sufficient. CBCT technology needs to be united with digital impressions to not only evaluate the surgical anatomy but also relate this information to the contours of where the final restoration will be. The fusion of these two technologies allows the clinician to properly plan both the implant placement and final restoration prior to any surgical therapy. Furthermore, the specific design of the final abutment and restoration can be chosen prior to surgery, and this will influence the exact placement of the dental implant.
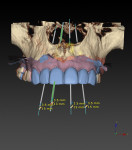
Digital Planning
The use of planning software that allows for the fusion of CBCT technology (ie, DICOM files) and digital impressions (ie, STL files) is important. However, it should not be a complex process to get the data into the program. Software now allows clinicians to take a single CBCT scan and a single digital impression of a partially edentulous patient and combine this information to properly plan the case digitally (NobelClinician SmartFusion, Nobel Biocare) (Figure 1). This digital workflow begins by accurately planning the contours of the final restoration (ie, through digital wax-up) and the technical aspects of the final design (eg, screw-retained versus cement-retained) to allow for proper implant placement. Ideally, the implant connection should be placed 3 mm apically and 2 mm palatially from the gingival zenith of the final restoration (ie, 3 x 2 rule) (Figure 2).1-3 This will allow for the proper "running room" needed to create an ideal emergence profile for the final implant restoration. After proper implant placement is planned in four dimensions2, the plan can then be transferred from the digital world to the patient's mouth via guided surgery.
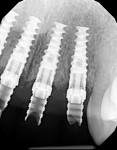
Implant Selection
The ideal implant position can only be attained if the implant chosen is the correct size for the tooth to be replaced.2 With the advent of platform switching in many current implant designs, it is important to understand that the emergence profile of the restoration begins from the width of the implant connection and not the width of the actual implant.4 As a result, a large offset between the width of the implant and the width of the connection can result in the need to place the implant deeper to allow for more running room to create the ideal emergence profile. Similarly, if an implant is chosen that is too narrow for the size of the tooth to be replaced, it also will need to be placed deeper to allow for this running room. It is important to understand that utilizing multiple implant widths with the same connection size does not change the emergence profile starting point. Proper depth of implant placement is paramount to long-term esthetic success, as placing an implant too shallowly will never allow for a proper emergence profile, bone stability, and tissue harmony.3 This may lead to long-term maintenance issues. Lastly, in today's implant therapy, it is vital that the implant connection type utilized lends itself to being restored in numerous ways, including those involving new innovations and technologies. Restorative flexibility is the key (Figure 3).
Restorative Design
The digital workflow requires planning the 3-dimensional position of the final restoration as well as the design of the final abutment prior to finalizing the surgical implant planning. The ideal position and contour of the final restoration are the most important factors to establish. Once they have been established, the position and size of the foundation required (ie, the dental implant and any hard- or soft-tissue grafting) can then be properly planned. Similar to the construction of a new house, the implant tooth replacement complex is planned from the top down and is begun with the end result in mind. The material choice and technical design of the restoration also can be planned prior to surgery. With new innovations in screw-retained technology such as angulated screw channels (Nobel Biocare), it is now possible for more than 95% of implant restorations to be screw-retained (Figure 4 through Figure 6). Documented issues involving the retention of excess cement around cement-retained final implant restorations leading to peri-implant mucositis and peri-implantitis have led many clinicians to regard screw-retained final restorations as the preferred design.5,6
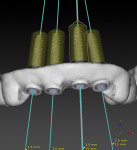
Guided Implant Surgery
After the 3D position and contour of the final restoration have been established and approved, the implant position and need for any hard- or soft-tissue augmentation can be determined. Selecting an implant platform that correctly relates to the size (ie, both mesio-distally and bucco-lingually) of the tooth to be replaced is crucial.7 Next, the "3 x 2 rule" can be used to establish the implant position and trajectory. This ideal position of the dental implant is then transferred from the digital planning software to the patient via computer-guided implant surgery. It has been demonstrated that fully guided implant surgery is the most accurate and predictable method of transferring the digitally planned implant position to the oral cavity during surgical placement.8,9 The surgical guide is designed in the planning software and then fabricated using a 3D printer (Figure 7). In partially edentulous cases, these surgical guides can be tooth supported, which makes them very easy to seat and stabilize. Moreover, they allow for many surgeries to be performed utilizing a flapless protocol. Implant placement utilizing a fully guided protocol facilitates ideal implant placement based on the digital restorative plan and also better prepares implant surgeons regarding the need for hard- and/or soft-tissue augmentation either prior to or during implant placement (Figure 8). This precision and predictability in surgical planning results in fewer surprises during surgery and allows for more accurate treatment planning for the patient. The benefits of guided surgery include increased accuracy and decreased surgical time.8,9 Furthermore, the procedure is often less invasive as it may involve a flapless protocol or at the very least, a more conservative flap design and reflection.
Tissue Augmentation and Biologics
Ideal implant placement based on the 3D position and contour of the final restoration is of paramount importance. Oftentimes, the placement of the dental implant in the ideal position is only possible after augmentation of the existing anatomy. In most instances, this involves osseous augmentation using various techniques and materials. Minimally invasive modalities generally provide the best esthetic results. Soft-tissue profile and thickness are also very important in planning implant cases.2,3 Due to the lack of strong periodontal tissue attachment, the presence of immobile tissue around the final implant restoration is necessary for long-term implant success. As a result, any tissue deficiencies, such as a lack of attached thick soft tissue, must be addressed. Therefore, it is essential that the software utilized to plan implant cases is able to indicate the current position of the soft tissues. Each case must be evaluated for the need for soft-tissue augmentation prior to implant surgery. In many cases, it is best to complete the soft-tissue augmentation prior to any osseous augmentation to allow for better tissue biotypes surrounding the osseous graft materials.
Recently, the use of blood biologics such as platelet rich fibrin and platelet rich plasma has become more commonplace in the profession (Figure 9). Recent research has indicated that the use of platelet rich fibrin and platelet rich plasma in augmentation procedures and implant surgery may benefit both hard and soft tissues in terms of healing time, surgical results, and osseointegration.10,11 To these ends, the adjunctive use of biologics in implant surgery is recommended whenever indicated.
Immediate Provisional Restoration
The placement of an immediate implant restoration provides many benefits. The immediate osseous stimulation around the dental implant enhances integration. Shaping the ideal emergence profile for the final restoration is the main purpose of the provisional restoration. However, to shape the soft-tissue profile, it is essential that the implant is placed at the proper depth and that the soft-tissue thickness is adequate. Furthermore, if the implant is placed too far facially, it is almost impossible to recover esthetically, and facial recession with bone loss is a long-term concern.12 When a provisional restoration is immediately placed on an immediately placed implant, it also provides the added benefit of maintaining the natural anatomic emergence profile that was established by the natural tooth root.12 Provisional restorations may be either screw-retained or cement-retained. Ideally, screw-retained provisional restorations are preferred in most cases. With the use of digital implant planning and fully guided implant surgery, it is now possible to fabricate a screw-retained provisional restoration prior to the surgery and deliver it intraorally with some slight modifications on the day of surgery (Figure 10 through Figure 12).
CAD/CAM-Milled Final Restorations
The material choice (eg, zirconia or lithium disilicate) and the restorative macro design (eg, monolithic or layered) of the final restoration can also be planned digitally prior to the surgery. Soft tissues have been shown to perform more favorably in the presence of a highly polished zirconia or titanium surface.13 Therefore, it is recommended that the subgingival portion of the implant restoration be comprised of highly polished zirconia or titanium. Whenever possible, ceramic material should not be used subgingivally.14 Now, monolithic designs can readily be utilized. In esthetic areas, designing all restorations to be monolithic on the palatal aspects with ceramic layering on the facial aspect allows for the best blend of structural integrity and esthetics. Overall, implant restorations should be designed to minimize prosthetic complications such as chipping. With the existence of esthetic, polychromatic monolithic materials such as zirconia and lithium disilicate, it is very possible to provide anterior implant restorations that are monolithic in design, but still very esthetic in appearance (Figure 13 through Figure 14).
Conclusion
Utilizing dental implants and a digital workflow has made tooth replacement therapy better today than it ever was before. The entire process can now be idealized and executed with great accuracy and predictability. Fully digital implant therapy using minimally invasive surgical procedures and precise prosthetic delivery using new materials and mechanics will soon become the standard of care. To master the ability to digitally merge the surgical and prosthetic modalities, practitioners will need to become familiar with and knowledgeable about the technologies and techniques available. Digital perio-prosthetic synergy is the future.
References:
1. Cooper LF, Objective criteria: guiding and evaluating dental implant esthetics. J Esthet Restor Dent.2008;20(3):195-205.
2. Funato A, Salama MA, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27(4):313-323.
3. Salama H, Salama MA, Garber D, et al. The interproximal height of bone: a guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998;10(9):
1131-1141.
4. Cappiello M, Luongo R, Di Iorio D, et al. Evaluation of peri-implant bone loss around platform-switched implants. Int J Periodontics Restorative Dent. 2008;28
(4):347-355.
5. Korsch M, Walther W. Peri-implantitis associated with type of cement: a retrospective analysis of different types of cement and their clinical correlation to the peri-implant tissue. Clin Implant Dent Relat Res.2015;17(Suppl 2):e434-e443.
6. Korsch M, Robra BP, Walther W. Cement-associated signs of inflammation: retrospective analysis of the effect of excess cement on peri-implant tissue. Int J Prosthodont. 2015;28(1):11-18.
7. Rosa AC, da Rosa JC, Dias Pereira LA, et al. Guidelines for selecting the implant diameter during immediate implant placement of a fresh extraction socket: a case series. Int J Periodontics Restorative Dent. 2016;36(3):401-407.
8. Pettersson A, Kero T, Gillot L, et al. Accuracy of CAD/CAM-guided surgical template on human cadavers: part 1. J Prosthet Dent. 2010;103(6):334-342.
9. Ozan O1, Turkyilmaz I, Ersoy AE, et al. Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg. 2009;67(2):394-401.
10. Kotsakis GA, Boufidou F, Hinrichs JE, et al. Extraction socket management utilizing platelet rich fibrin: a proof-of-principle study of the "accelerated-early implant placement" concept. J Oral Implantol. 2016;
42(2):164-168.
11. Öncü E, Alaaddinoğlu EE. The effect of platelet-rich fibrin on implant stability. Int J Oral Maxillofac Implants. 2015;30(3):578-582.
12. Kinaia BM, Ambrosio F, Lamble M, et al. Soft tissue changes around immediately placed implants: a systematic review and meta-analyses with at least 12 months follow up after functional loading. J Periodontol. 2017;88(9):976-886.
13. Linkevicius T, Vaitelis J. The effect of zirconia or titanium as abutment material on soft peri-implant tissues: a systematic review and meta-analysis. Clin Oral Implants Res. 2015;26(Suppl 11):139-147.
14. Linkevicius T. The novel design of zirconium oxide-based screw-retained restorations, maximizing exposure of zirconia to soft peri-implant tissues: clinical report after 3 years of follow-up. Int J Periodontics Restorative Dent. 2017;37(1):41-47.