Anterior Biomechanical and Esthetic Failure Leading to Success
Using creative restorative care to accommodate a patient’s lifestyle needs
Hugh Flax, DDS, AAACD, MICOI
Successful smile design depends not only on the artistic skills of the dentist and the ceramist, but also on the management of biomechanical strength, periodontal support, and occlusal function vectors.1 This is especially critical with esthetic restoration of an endodontically treated tooth. As Kois says, “Preservation of tooth integrity and strength is important for the long-term survival of endodontically treated teeth. Endodontic post space preparation requires reduction of the remaining supportive tooth structure. Restorative modalities following root canal must provide sufficient strength for the prosthetic material and tooth structures.”2 When the biomechanical limits have been exceeded by fracture or tooth resistance, and/or crown lengthening either compromises the one-to-one stability ratio or creates an esthetic liability, the tooth should be removed and ideally replaced by an implant-supported tooth replacement, as was done in the following case.3,4
Case Presentation
A healthy 47-year-old man injured tooth No. 9 as a teenager playing basketball. The tooth was chipped and eventually underwent endodontic therapy. About 2 years prior to this case, the tooth turned dark and the patient’s dentist advised that he needed a crown. While on a business trip with a temporary crown, he bit into a protein bar and fractured the tooth close to the gumline (Figure 1). The emergency dentist said the tooth broke inside the temporary and needed a post. When the patient returned to Atlanta, his regular dentist delivered the crown without a post. When the patient went out of town again, the crown dislodged, and another emergency dentist adjusted the bite and recemented the crown.
Frustrated and hoping for a solution that would not compromise his busy schedule and image, the patient sought our assistance. In addition, he wanted a whiter smile and to possibly close the diastema in his smile non-orthodontically, and as efficiently as possible, to not interrupt his demanding personal and professional schedules that frequently included international travel.
Examination and Treatment Planning
Prior to our examination, a full series of diagnostic photos, radiographs, and models were assembled.
Our exam discovered that esthetically, the patient displayed the majority of his upper and lower teeth and a large amount of gums when smiling with a scalloped triangular architecture and thin biotype. There were multiple diastemata due to tooth size and arch form (Figure 2). Functionally, though the patient was aware of a clenching habit from stress, there was no fremitus or muscle tenderness evident.
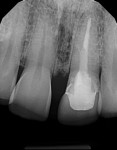
Periodontally, bone levels were adequate, but there was generalized recession in the bicuspid and molar regions, as well as irritated dark tissue around tooth No. 9 that indicated a biologic width issue from restorative infringement of the periodontal complex. Restoratively, the lack of ferrule at tooth No. 9 was inadequate for long-term stability of the restoration. Endodontic care and restorative procedures had decreased dentinal volume and made the tooth less fracture resistant as well (Figure 3). The rest of the dentition was intact with abundant enamel to resist decay risk factors as long as home care was excellent and the saliva remained non-acidic.
Diagnostically, tooth No. 9 was a liability to all four areas of potential risk. It was determined that the tooth should be removed and meticulously replaced to blend esthetically with the rest of his smile. The following treatment options were given to the patient:
• Do nothing (which didn’t solve any of his problems, but at least offered less pressure to make a decision).
• Remove tooth No. 9 and use Invisalign® (Align Technology, www.aligntech.com) to temporarily replace the tooth and close spaces prior to implant placement and crown restoration.
• Replace tooth No. 9 with an implant-supported crown, an Essix® (DENTSPLY Raintree Essix, www.essix.com) retainer to replace the tooth, and possible veneers.
• Replace tooth No. 9 with a fixed prosthesis and possible veneers.
The patient was very distressed about potentially losing his front tooth as a result of a lack of ferrule space and enough physical tooth structure to allow retention. The options of a bridge or implant for tooth replacement were discussed. The patient’s biggest concerns were that a lengthy treatment time would disrupt his professional schedule and that the Essix tooth replacement or Invisalign treatment would make eating difficult at business functions. He understood that placing an implant to replace failing tooth No. 9 was the most conservative and predictable option from a dentistry standpoint, but it did not meet the needs of his lifestyle.
Although losing tooth structure is not ideal, in this case, it was cost/risk that the patient was willing to take for peace of mind during the process. A “blended” option was offered with a bone-sparing grafted extraction and a transitional bridge, eventually leading to three separate units (No. 9 being implant-supported) so that his business life would not be compromised. Tooth No. 7 would be bonded and eventually replaced with a porcelain veneer. This option was not the most conservative option but blended with the patient’s temperament and needs. A transitional bridge instead of a flipper or Essix seemed to be a “better answer” for him.
Due to the scalloped thin tissue and high lip line, the literature5-7 indicated delayed implant placement as the most predictable surgical approach in this circumstance, even though immediate replacement would have been more efficient.8
Surgical Phase
Since implant placement is ideally prosthetically driven,9 facial planning records were taken to establish midline and incisal edge placement using a stickbite and a Kois Dento-Facial Analyzer (Panadent, www.panadent.com). This was done after the patient had been equilibrated using an anterior deprogrammer to give the lab technician an accurate centric relation bite record. While a functional wax-up (Figure 4) was being created, the patient had power bleaching performed to establish a prior to this case, whiter and more attractive yet still natural color for his smile.
Upon approving the wax-up and getting a vital sign baseline for oral conscious sedation, the patient was scheduled for removal/grafting of tooth No. 9 and esthetic restorative augmentation of the adjacent teeth Nos. 7, 8, and 10 to close the spaces and create a gingival-friendly environment. Teeth Nos. 6 and 11 were scheduled for a mesioincisolingual bond to improve canine guidance and close the mesial diastema.
Under triazolam conscious sedation and local anesthesia, teeth Nos. 8 and 10 were conservatively prepared for full coverage1 and the crown on No. 9 was removed. A provisional bridge was made with a bis-acryl material reinforced internally with Ribbond® (Ribbond, www.ribbond.com) and an ovate pontic created at No. 9. At teeth Nos. 6, 7, and 11 mesially, the soft tissue architecture was atraumatically sculpted with an erbium laser to create the framework for the proposed bonding using a setting of 2 W and a 20% water/air mix. To create the bonded modifications on teeth Nos. 6, 7, and 11, minimal tooth preparation was done with slight beveling with coarse diamond burs, air abrasion with 40-μm aluminum oxide, chemical etching with 37% phosphoric acid, and a coating of resin that was cured for 30 seconds. Using a linguoincisal matrix of the wax-up, enamel and dentin opacities of a nanofilled B1 composite were adapted and polished to match the provisional.
Tooth No. 9’s root was carefully elevated and removed using a bone-sparing removal technique and socket repair V-shaped cone graft to maintain the buccal plate as outlined by Elian and Tarnow.2 The graft consisted of 50% demineralized cortical bone mixed with 50% mineralized cancellous bone that was wetted by sterile saline. The site was closed with 5-0 resorbable gut sutures. Very carefully, the provisional bridge for teeth Nos. 8 through 10 was placed with a disinfectant/desensitizer and a thin coat of reversible cement. The patient was comfortable and returned for his postoperative care. He was very pleased that the change was comfortable and invisible to his colleagues (Figure 6).
Four months later, after planning with a CBCT and while sedated with triazolam 0.25 mg, aseptic surgical placement of a 3.7 mm x 13 mm hydroxyl-apatite coated implant was performed with a papilla sparing flap using Misch’s technique3 of osteotomes and slightly to palatal to maintain strength and anatomy to the buccal tissues (Figure 6). To further optimize the labial, AlloDerm® GBR membrane (BioHorizons, www.biohorizons.com) was placed under the flap and over 50% demineralized cortical bone mixed with 50% mineralized cancellous bone mixed into plasma rich in growth factors derived from the patient’s own plasma. Full closure was achieved by placing six PGA dissolvable sutures and the provisional was stabilized initially with an antibiotic ointment and then recemented more conventionally 3 days later at his postoperative visit (Figure 7). He was comfortable and happy with the results.
Restorative Phase
Three months later, to develop the restorative soft tissue profile around the implant, the provisional bridge was converted to a screw-retained crown by carving a shell out of the pontic and luting it to a temporary abutment that was placed on the implant,4 accessed with a tissue punch and erbium laser. After meticulous contouring and polishing of the screw-retained portion (Figure 8), the provisional was recemented on the abutments on teeth Nos. 8 and 10. The author then hand tightened the abutment on tooth No. 9 and sealed the lingual with cotton and composite to protect the abutment. The patient was given detailed home care instructions by our staff prior to a 2-month international trip.
After the patient returned, the tissue was very healthy and well adapted to the contours. Esthetically and functionally, the patient was very pleased with his progress. Records were made of the provisionals including incisal gingival lengths with digital calipers to augment photos and impressions. The provisionals were removed, and an open-tray impression coping was immediately placed into the implant and then the flowable composite was dispensed and cured around the coping and into the sulcus to preserve the anatomy for accurate emergence profile duplication (Figure 9) for a CAD/CAM customized hybrid abutment (zirconia luted to titanium). The veneer preparation on tooth No. 7 was refined and polished prior to a full-arch impression. The teeth were reprovisionalized and home care was reinforced. Detailed instructions and photography/impressions were sent to the lab.
Using matrices of the provisionals in addition to a soft tissue model and photos with shades of the preparations and adjacent teeth, the lab made lithium disilicate restorations and a customized abutment. The abutment was designed to preserve natural contours and crown margin only 2 mm below the gingival margin for easy clean-up of the cement-retained restoration. All materials were verified upon returning from the lab, and were seated in the patient’s mouth. A seating jig for the implant abutment (Figure 10) assured proper positioning. After signed patient approval, the abutment was torqued to 20 Ncm with a handpiece for accuracy. The access hole was sealed with Teflon tape and composite, and the crown was seated using contemporary implant crown cementation.1 The veneer and two crowns were luted with light-cured resin cements and margins meticulously cleaned and smoothed. The patient returned in 1 week for a nighttime appliance. The patient was very satisfied with the esthetics and quality of care (Figure 11).
Summary
Preservation of hard and soft tissue is mission critical in dentistry. Attention to detail prevents patients from suffering needless loss of time, money, and emotional capital. Often creativity is needed to mesh lifestyle requirements and patient temperament together with dental care. Blending today’s technology and materials can often take a failure and achieve a successful outcome.
Disclosure
Hugh Flax, DDS, AAACD, MICOI, has no relevant financial relationships to disclose.
About the Author
Hugh Flax, DDS, AAACD, MICOI
Private Practice
Atlanta, Georgia
References
1. Kois JC. Diagnostically Driven Interdisciplinary Treatment Planning Course December 12-14, 2007.
2. Baba NZ, Goodacre CJ, Daher T. Restoration of endodontically treated teeth: the seven keys to success. Gen Dent. 2009;57(6):596-603.
3. De Backer H, Van Maele G, Decock V, Van den Berghe L. Long-term survival of complete crowns, fixed dental prostheses, and cantilever fixed dental prostheses with posts and cores on root canal-treated teeth. Int J Prosthodont. 2007;20(3):229-234
4. Priest G. Single-tooth implants and their role in preserving remaining teeth: a 10-year survival study. Int J Oral Maxillofac Implants. 1999;14(2):181-188.
5. Kois JC. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2004:25(11):895-896, 898.
6. Pikos MA, Steigmann M. Myths vs. realities: flapless and flap implant surgery. Journal of Cosmetic Dentistry. 2012;28(2):54-66.
7. Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524-532, 534.
8. Funato A, Salama MA, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27(4):313-323.
9. Garber DA, Belser UC. Restoration-driven implant placement with restoration-generated site development. Compend Contin Educ Dent. 1995:16(8):796-802, 804.
10. Kois JC, McGowan S. Diagnostically generated anterior tooth preparation for adhesively retained porcelain restorations: rationale and technique. J Calif Dent Assoc. 2004;32(2):161-166.
11. Elian N, Cho SC, Froum S, et al. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104.
12. Misch CE. Anterior single-tooth replacement: surgical considerations. In: Misch CE, ed. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby; 2008:739-768.
13. Murphy K. Delivering a screw retained provisional for immediate implant placement. Journal of Cosmetic Dentistry. 2012;28(2):75-82.
14. Bunek S. Cement selection for cement retained implant prostheses. Journal of Cosmetic Dentistry. 2012; 28(2):140-141.