Endodontic Treatment Strategies
Principle-driven approaches for successful outcomes
Endodontic therapy is an integral part of natural tooth retention in general dentistry. Risk assessment in endodontics is a critical skill, especially for general practitioners (GP) as they make treatment-planning decisions to retain natural teeth. Treatment planning for nonsurgical initial endodontic therapy involves deciding if treatment will be handled by the GP or referred to a specialist; planning the actual endodontic procedure (assessing risk factors, choosing needed materials, opting for particular cleansing, shaping, and obturation techniques); and deciding on the post-endodontic restoration (posted/non-posted, crown/no crown).
This discussion of principle-driven treatment strategies aims to make the practitioner’s clinical decision-making process and overall experience more predictable, efficient, and ultimately successful.
Patient Assessment
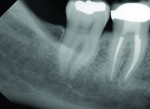
Determining which patients and which teeth to treat depends upon each clinician’s skill and comfort level and is a significant indicator of long-term endodontic success.When treatment is delivered properly the first time, chances for success are optimized. Alternatively, mishaps such as an iatrogenic event or failure to profoundly anesthetize the patient lead to anxiety and frustration for all parties (Figure 1).
It is the author’s personal bias that speed and excellence in endodontics are usually mutually exclusive. Anticipating, planning for, and meeting challenges—such as patients who gag or cannot be reclined, have limited openings, dental phobia, curved and calcified roots, atypical anatomy, tooth rotation, or tipping—are essential to optimize the result. Decisions regarding whether the tooth is restorable, whether referral is the best option, and, if treatment is decided upon, how it should be performed, should be made early on. Almost without exception, it is better for clinicians with appropriate resources and experience to start cases that can be completed rather than starting treatment and hoping to finish without referral. Starting treatment with the hope of finishing is rarely in the best interest of the patient.
Specifically, when contemplating treatment, clinicians should ask themselves these questions: Is the tooth restorable? Is the problem endodontic and will an endodontic procedure solve the patient’s problem? Do I have the skills, time, equipment, and desire to treat this patient and tooth optimally? What risk factors are present in this given clinical situation? How will I overcome these risk factors—in other words, what specific instrumentation and obturation methods will meet the challenges present? And finally, post-endodontics, how will I restore this tooth to full function and esthetics?
Although a comprehensive discussion of endodontic diagnosis is beyond the scope of this article, it is important to mention that the clinician and patient are best served if the chief complaint is reproduced. For example, if the patient has pain to cold, all the teeth in the quadrant and the contra lateral tooth should be tested to cold to reproduce the patient’s symptoms. At times, delaying treatment until symptoms localize or choosing referral may be best until the diagnosis is confirmed.
Treatment Strategies
If the clinician considers the questions above and opts to treat the patient, the principle-driven, time-honored treatment strategies discussed below can improve clinical predictability. These strategies are universal and independent of any particular commercial system.
Anesthesia Administration and Testing
Once treatment has been decided upon and informed consent obtained, profound anesthesia is essential. Irreversible pulpitis routinely requires supplemental anesthesia—either periodontal ligament injections or intraosseous anesthesia. To perform single-tooth anesthesia (STA), the author has found The Wand® from Aseptico (www.aseptico.com) to be indispensible for local anesthesia, especially for the difficult-to-anesthetize, irreversibly inflamed lower molar. The author finds the device is more comfortable for patients, has a low rate of aspiration, and that it efficiently and predictably enables the periodontal ligament injection. Intraosseous injections (eg, X-Tip™, DENTSPLY Maillefer, www.maillefer.com, Anesto; W&H Group, www.wh.com) required after use of The Wand are few.
Once an adequate volume and placement of local anesthetic is administered, it is advisable to test the patient before initiating treatment. For example, if the patient was sensitive to cold, before starting the procedure, testing the tooth to cold (eg, Endo-Ice®, Coltene, www.coltene.com) can confirm complete anesthesia.
Canal Location
Once treatment is initiated, a rubber dam is essential for visual and microbial control. It is the legal and ethical standard of care. Visual and tactile control is ideally optimized with a surgical operating microscope or loupe. Access, using the rubber dam and enhanced visualization and magnification, can be carried out with any number of burs. However, a universal bur kit might contain, among others, a round #2 diamond for porcelain access; a 557 carbide (or safe-ended similar bur); #2, #4, and #6 long shank rounds; a diamond chamfer; and fine and coarse composite football-shaped finishers for composite and glass ionomer access fillings.
Access should be straight-line and result in a canal path that allows hand K-files to be placed to the point of first canal curvature without deflection off canal walls. In practical terms, this means the cervical dentinal triangle should be removed first as the coronal third is shaped with orifice openers. Means to shape the orifice vary, but rotary nickel-titanium (RNT) orifice openers (.08/25) are generally more than adequate to shape the coronal third. They also allow optimal volumes of irrigant to flow into the canal and provide easy insertion for subsequent hand file negotiation. Such orifice openers should be used in a brushing motion up and away from the furcation toward the canal wall of greatest bulk.
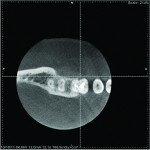
Canal location is obviously enhanced with cone-beam computed tomography (CBCT) technology. Indications for CBCT scans include resorption; atypical root numbers and configuration; need for approximation of vital structures—(eg, mandibular canal and mental nerve); suspicion of vertical fracture, etc. Although not every endodontic case requires a CBCT, the value of having CBCT capability when needed cannot be overstated (Figure 2 and Figure 3).
Prior to initiating canal negotiation and instrumentation, it is important to verify that all canals have been located. Caution and clinical judgment are required, as atypical and unexpected canal anatomy is the norm, not the exception. For example, the distal root of many lower molars often has a second canal starting below the pulpal floor, which can be located by searching laterally in a buccal and lingual direction. The same is true of the mesial root of lower first molars, which often contain a third canal, found by ultrasonic troughing between the mandibular and mesiolingual canals.
Canal Negotiation and Shaping
Canal negotiation with hand files is an integral and essential component of endodontic therapy and sets the stage for excellent cleaning and shaping results. Once the canals are ready for negotiation—whether the clinician is using RNT files or reciprocated nickel-titanium instruments (ReNT) for bulk canal shaping—the canal should be negotiated and opened to the size of a #15 to #20 hand K-file from the orifice to the minor constriction (MC) of the apical foramen to create a glide path. If desired, .05 tapered nickel titanium hand files (Mani Flare #15 and #20 nickel titanium hand files; Mani, Inc; www.mani.co.jp) can be used to finalize the glide path after negotiation and initial enlargement of the glide path either manually or via reciprocation. Regardless of whether RNT or ReNT instruments are used, entry of nickel-titanium instruments into canals without prior hand file exploration and glide path creation is the harbinger of instrument fracture, transported canals, and iatrogenic events.
Although hand file options differ for obtaining and maintaining patency, in general, small, stiff, pre-curved hand files are optimal for early canal negotiation, such as Mani’s #6 and #8 hand K-files. There are also files designed specifically for calcified canals (Mani D Finders). Once negotiated to the MC with a small hand K-file and an electronic apex location (iRoot, Meta BioMed Co, www.meta-biomed.com) is made, the canal is enlarged with hand files to prepare the glide path.
Although a RNT glide path can be prepared, a safe and reliable alternative is to reciprocate small hand K-files sequentially from #6 through #15 as required by the case. Safe-ended K-files can also be reciprocated as desired (eg, Mani SEC O K files). Reciprocation can be performed using the W&H WA 62A reciprocating handpiece, which fits on an E type coupling of an endodontic motor (AEU-27A, Aseptico, www.aseptico.com) (Figure 4 and Figure 5).
Different canal anatomies require different shaping strategies; shaping every canal the same way will inevitably lead to clinical misadventure. For example, always using a crown-down instrumentation approach, or always using ReNT files in every anatomy encountered can lead to canal blockage, extruded debris, canal transportation, possible instrument separation, and other untoward events. It is beyond the scope of this article to describe every anatomy possible and each shaping strategy to manage every variable. In general, there are four primary methods of canal shaping using nickel titanium instruments: crown down, step back, reciprocated technique, and a hybrid of these.
It is a foundational concept that the clinician may wish to move between these different strategies—especially when a given method is not proving effective during treatment. For example, in a 3-dimensional (3D) multi-planar apical curvature, the coronal two thirds of the root may often be shaped crown down using instruments from larger to smaller tapers and tip sizes (.08/25, .06/25, .04/25, .03/25, .02/25, etc). After the apical third is shaped, the clinician may switch to a step-back technique (.02/25, .03/30, .03/40, etc) until the desired taper of the canal is prepared and the chosen master apical diameter subsequently shaped. In this scenario, clinicians wishing to prepare the apical third using reciprocation for the apical third—instead of a step-back method—certainly could do so.
Inherent in moving between such shaping techniques is conceptual awareness—ie, clinicians should know at all times in the process, both literally and figuratively—where they are, where they need to go, and how they will get there in the treatment process. Because canal instrumentation occurs to one degree or another (beyond the limits of the surgical operating microscope) via tactile feedback, clinicians must understand the potential risks involved in choosing any given way forward in the clinical process. Aside from the preoperative risk assessment, they should have some idea of the desired master apical taper and diameter of the prepared canal. It is axiomatic that more complex root forms will have smaller final prepared tapered tapers and apical diameters and vice versa for less complex root forms. The above notwithstanding, the endodontic literature is nearly unanimous that larger apical diameters and tapers provide improved canal cleanliness.1-10
Irrigation and Obturation
Irrigation should be copious and activated throughout the treatment process. Irrigating after every insertion of a nickel-titanium instrument and recapitulating with small hand files to assure patency is the greatest protection against canal blockage and possible subsequent canal transportation. Means of activating irrigation include passive ultrasonic irrigation, negative pressure irrigation, sonic irrigation, and mechanical activation, among others. Heating irrigating solutions and alternating the primary bactericidal irrigant with liquid ethylenediaminetetraacetic acid (EDTA) has merit.
It is noteworthy that viscous EDTA gel solutions are used differently than liquid EDTA. EDTA gels are used for lubrication, to help chelate dentin and to hold debris in suspension so that it will not be forced apically during repetitive file insertions early in the shaping process. Clinically, when a pulp chamber is opened and full of pulp, EDTA gel can help prevent its apical compaction.
Shaping procedures are complete when the final prepared canal shape can be adequately irrigated and obturated. For the vast majority of roots, this is a final prepared taper of .06. As mentioned, larger master apical diameters are correlated with cleaner final canals. Regardless of whether the clinician uses a master cone–based obturation technique or carrier-based product, the final result should 3D seal the canal from the orifice to the MC.
Not every obturation technique is ideal for every potential anatomy. Within the same tooth, different techniques may be valid. Once obturation is complete, the access should be sealed under the rubber dam, ideally at the same appointment, with or without a post, depending on the clinical indication. It is axiomatic that endodontic clinical success is improved with an early and appropriate coronal seal relative to exposing the obturation to coronal leakage.11-16
Conclusion
This article has described the key features of initial endodontic therapy from a clinically relevant perspective for GPs. Emphasis has been placed on preoperative risk assessment; straight-line access; obtaining patency; copious and activated irrigation; shaping strategies that are relevant to the anatomy encountered; 3D obturation; and immediate placement of a post-endodontic coronal seal.
The author would welcome reader feedback about this article (e-mail: RichardMounce@MounceEndo.com, Twitter: @MounceEndo).
Disclosure
Dr. Mounce owns MounceEndo, LLC, which markets the rotary nickel-titanium MounceFile in Controlled Memory© and Standard NiTi, as well as Mani, Meta BioMed, and Aseptico Products.
References
1. Shuping G, Orstavik D, Sigurdsson A, Trope M. Reduction of intracanal bacteria using nickel-titanium rotary instrumentation and various medications . J Endod. 2000;26(12):751-755.
2. Siqueira J, Lima KC, Magalhaes FA, et al. Mechanical reduction of the bacterial population in the root canal by three instrumentation techniques . J Endod. 1999;25(5):332-335.
3. Parris J, Wilcox L, Walton R. Effectiveness of apical clearing: histological and radiographical evaluation. J Endod. 1994;20(5):219-224.
4. Card SJ, Sigurdsson A, Orstavik D, Trope M. The effectiveness of increased apical enlargement in reducing intracanal bacteria. J Endod. 2002;28(11):779-783.
5. Rollison S, Barnett F, Stevens RH. Efficacy of bacterial removal from instrumented root canals in vitro related to instrumentation technique and size. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(3):366-371.
6. Tan BT, Messer HH. The quality of apical canal preparation using hand and rotary instruments with specific criteria for enlargement based on initial apical file size. J Endod. 2002;28(9):658-664.
7. Falk KW, Sedgley CM. The influence of preparation size on the mechanical efficacy of root canal irrigation in vitro. J Endod. 2005;31(10):742-745.
8. Dalton BC, Orstavik D, Phillips C, et al. Bacterial reduction with nickel-titanium rotary instrumentation. J Endod.1998;24(11):763-767.
9. Siqueira JF Jr, Lima KC, Magalhaes FA, et al. Mechanical reduction of the bacterial population in the root canal by three instrumentation techniques. J Endod. 1999;25(5):332-335.
10. Usman N, Baumgartner JC, Mashall JG., Influence of instrument size on root canal debridement. J Endod. 2004;30(2):110-112.
11. Torabinejad, M, Kutsenko D, Machnick TK, et al. Levels of evidence for the outcome of nonsurgical endodontic treatment . J Endod. 2005;31(9):637-646
12. Ray H, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration . Int Endod J. 1995;28(1):12-18.
13. Tronstad L, Asbjornsen K, Doving L, et al. Influence of coronal restorations on the periapical health of endodontically treated teeth . Endod Dent Traumatol. 2000;16(5):218-221.
14. Lazarski MP, Walker WA III, Flores CM, et al. Epidemiological evaluation of the outcomes of nonsurgical root canal treatment in a large cohort of insured dental patients . J Endod. 2001;27(12):791-796.
15. Kirkevang LL, Orstavik D, Horsted-Bindslev P, Wenzel A. Periapical status and quality of root canal fillings and coronal restorations in a Danish population . Int Endod J. 2000;33(6):509-515.
16. Dugas NN, Lawrence HP, Teplitsky PE, et al. Periapical health and treatment quality assessment of root-filled teeth in to Canadian populations . Int Endod J. 2003;36(3):181-192.
About the Author
Richard E. Mounce, DDS
Private Practice
Rapid City, South Dakota