Tissue Fluoresence for Early Oral Cancer Detection
Cellular changes and mucosal abnormalities are more readily identified
Oral cancer rates have increased approximately 15% from the 1970s to 2004, according to the latest National Cancer Institute Survey. With 42,000 Americans being diagnosed with oral or oropharyngeal cancer annually, leading to more than 8,000 deaths, these conditions are killing one person per hour, 24 hours per day. Of those newly diagnosed patients, only half will survive in 5 years. Why? Because the standard oral cancer examination requires a change to be visible to the unaided eye or something that is palpable manually. Unfortunately, at this stage cancerous changes are typically advanced and prognosis worsens considerably.
The key to survival is detection of cell changes at the earliest possible stage, prior to the cells penetrating into blood vessels and allowing them to spread to deeper and more distant structures.1 Early detection of cellular changes has been reported to increase survival 80% to 90%.2
Examining the Causes
Age is frequently named as a risk factor for oral cancer, with increases in incidence with older populations. Recent data reveal, however, that the fastest growing segment of the oral cancer population are nonsmokers younger than 50 years, which suggests a shift in the cause of the disease. Oral cancer frequently occurs in the anterior of the mouth. In the past, tobacco- and alcohol-associated cancers were the major types identified, but these have declined along with a corresponding decline in smoking. Pharyngeal and tonsillar cancers are being identified more frequently. These occur in the posterior of the oral cavity and are associated with the human papillomavirus (HPV).
It does not appear that HPV acts synergistically with tobacco or alcohol, and HPV represents a completely unique and independent disease process. Studies report an HPV prevalence of 30.1%3 in oral squamous cell carcinoma and 91%4 in pharyngeal cancer, indicating this virus has a high connection to oral cancer. So how can oral healthcare professionals increase and improve detection of HPV and the cellular changes associated with oral cancer to help improve patient survival?
Detection Through Fluorescence
Tissue fluorescence has been demonstrated by the literature to aid in identification of cellular tissue changes that are not apparent with white light examinations and has been used in screening for lung cancer for more than 20 years. VELscope® Vx (DenMat, www.denmat.com) has been developed and subsequently reported in the literature to provide tissue fluorescence testing that can be safely and predictably performed in the dental office by either the dentist or hygienist. Like other diagnostic technologies, such as panoramic and intraoral radiography, VELscope is not a stand-alone test. Used in conjunction with a standard oral soft tissue exam, VELscope provides visual information that cannot be acquired in any other way. Sensitivity and specificity for VELscope has consistently been reported to be 92% and 77%, respectively.5
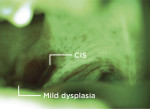
When VELscope’s safe blue light is illuminated into the oral cavity, this excites natural fluorophores from the surface of the epithelium through to the basement membrane, where premalignant changes typically begin, and into the stroma beneath, causing it to fluoresce. VELscope’s proprietary filter allows fluorescence visualization by blocking reflected blue light and enhancing the contrast between normal and abnormal tissue. Tissue that may have initiated dysplasia or is showing more advanced cellular changes appears dark (non-fluorescing) in contrast to normal tissue, which has a fluorescent glow under the VELscope.
In addition to the detection of oral cancers and pre-cancers, the VELscope can be a powerful tool for the discovery of mucosal abnormalities such as viral, fungal, and bacterial infections and inflammation from a variety of causes (including lichen planus and other lichenoid reactions), as well as squamous papillomas and salivary gland tumors.
Improved Oral Cancer Examination
A thorough examination involves traditional techniques, which include palpation and visual examination of the oral cavity with particular attention paid to the lateral borders of the tongue, tonsillar area, and oraphyranx, as these are high-risk areas for cellular changes. In the next step, VELscope is activated and the exterior lips are examined through the device for potential changes that may signify abnormalities. The interior of the lips are next examined with the VELscope, along with the buccal mucosa bilaterally, the hard and soft palates (Figure 1 and Figure 2), the tonsils (Figure 3 and Figure 4), the oraphyranx, the floor of the mouth, lateral borders of the tongue (Figure 5 through Figure 8), and dorsal of the tongue.
VELscope is available with a digital camera for documentation; when abnormalities are noted, images can be printed or e-mailed, aiding the practitioner in identifying where the biopsy should be performed.6 It has also been noted that VELscope aids in identifying the extent of the dysplastic changes when surgery is indicated, so that the area’s borders can be included in the excision and dysplastic tissue not left behind.
Conclusion
Early detection of cellular changes increases patient survival. Tissue fluorescence testing with the VELscope has shown a high sensitivity with oral cancer detection. Once identified, the area can be monitored over a short period to verify resolution or tissue biopsy can be performed to confirm precancerous or malignant conditions that will require further clinical treatment.
References
1. Oral Cancer Incidence (New Cases) by Age, Race, and Gender. National Institute of Dental and Craniofacial Research website. www.nidcr.nih.gov/DataStatistics/FindDataByTopic/OralCancer/OralCancerIncidence.htm. Accessed June 15, 2013.
2. U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, NIDCR, NIH; 2000.
3. Kansy K, Thiele O, Freier K. The role of human papillomavirus in oral squamous cell carcinoma: myth and reality [published online ahead of print December 16 2012]. Oral Maxillofac Surg. https://link.springer.com/article/10.1007/s10006-012-0383-0. Accessed June 15, 2013.
4. Carpenter DH, El-Mofty SK, Lewis JS Jr. Undifferentiated carcinoma of the oropharynx: a human papillomavirus-associated tumor with a favorable prognosis. Mod Pathol. 2011;24(10):1306-1312.
5. Marzouki HZ, Tuong Vi Vu T, Ywakim R, et al. Use of fluorescent light in detecting malignant and premalignant lesions in the oral cavity: a prospective, single-blind study. J Otolaryngol Head Neck Surg. 2012;41(3):164-168.
6. Kois JC, Truelove E. Detecting oral cancer: a new technique and case reports. Dent Today. 2006; 25(10):94, 96-97.
Gregori M. Kurtzman, DDS, MAGD
Private Practice
Silver Spring, Maryland
Former Assistant Clinical Professor
University of Maryland
Department of Endodontics, Prosthetics, and Operative Dentistry
Baltimore, Maryland