Two Options for Class II Primary Molar Restoration
Faster, easier restorations need not compromise reliability
In a survey of 1,043 dentists, CR Foundation asked, “What material would the respondent use in a 7-year-old patient for repair of a mandibular primary first molar that had a prior occlusal amalgam and radiographic evidence of new proximal caries?”1 The dentists surveyed responded with a variety of material options, including stainless steel crown (32%), resin-based composite (RBC) with no liner/base (30%), resin-modified glass-ionomer (RMGI) restorative cement (9%), RBC overlying a RMGI liner/base (8%), silver amalgam without a base (7%), silver amalgam with glass-ionomer base (6%), and conventional glass-ionomer cement (4%). The remaining percentage of dentists gave some other option.
As experienced pediatric dentistry clinicians, the authors believe that the survey results identify two trends in restorative dentistry for children. The first is that dental students often do not receive enough experience with preformed stainless steel crowns during their training to foster comfort and confidence using them once they progress into practice. Surely more than one third of dentists should know that stainless steel crowns are often the best option for severely damaged or malformed primary molars and, in certain cases, permanent posterior teeth.2
The second trend is that RMGI restorative cements have not universally caught on with dentists in the past 20 years. This trend is likely related to the remarkable improvements in resin-based composites over the decades. The best of the RMGI cements have inherent properties that give them advantages over other direct application restoratives and make restorative dentistry for children faster and easier with proven reliable results.3-5
Case 1
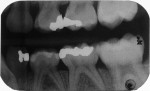
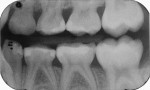
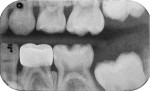
A 6-year-old was seen for initial examination. He had been treated previously in another pediatric dentistry office. Medical history was noncontributory. Head and neck findings were all unremarkable except that intraoral examination revealed multiple silver amalgam and RBC restorations in each quadrant in varying states of repair. Dental caries was observed clinically and on bitewing radiographs at the margins of most restorations, and the four Class II amalgams in the maxillary primary molars had isthmus fractures (Figure 1 and Figure 2). Records from the prior dentist revealed that the restorative care had been completed between 1.5 and 2 years ago.
After advising the patient’s mother that pulpotomy and stainless steel crown repair was a possibility for any or all of the maxillary primary molars, it was decided to first attempt restoration using RMGI restorative cement. A RMGI liner would be used for additional protection of the pulps. The patient’s mother related that she preferred tooth-colored restorations, but readily consented to whatever restorative method that proved necessary.
Treatment
The maxillary molars were treated in two appointments. The patient was most cooperative, and cushioned earphones with children’s music were used for his comfort.
After appropriate anesthetic injections in the maxillary left molar region, the rubber dam was placed using the “slit dam” method.6 The silver amalgams were cut away using a water-cooled high-speed diamond bur with high volume evacuation of debris. Much carious dentin was revealed (Figure 3). Using slow-speed round burs, all carious substance was debrided. There was no pulp space exposure, although the lesions penetrated deeply.
RGMI liner (Vitrebond™ Plus, 3M ESPE, www.3mespe.com) was injected internally, spread in a thin layer over the dentin surface, and hardened by visible light exposure. Excess RMGI liner was trimmed with a slow-speed inverted cone bur. Stainless steel matrix strips (Strip T, Denovo Dental, www.denovodental.com) were contoured and wedged into position (Figure 4).
After applying and air-drying the RMGI primer, it was exposed to the curing light beam for 10 seconds, according to manufacturer’s instructions. The RMGI “nano-ionomer” (Ketac™ Nano, 3M ESPE) was injected into the first molar preparation, with care to avoid air inclusion (Figure 5). The manufacturer also recommends injecting and curing the material in layers of 2 mm or less.
The material was hardened with 20 seconds exposure to the visible light beam (1,200 mW mm2) (Figure 6). The most mesial matrix strip was removed (Figure 7) and the remaining strip was re-wedged into place. The second molar preparation was then filled in the same manner. The occlusal surfaces were trimmed and shaped with slow-speed round diamond burs (Figure 8) and the marginal ridge was carved with a fine pointed carbide bur (Fissurotomy® Micro NTF, SS White, www.sswhiteburs.com) (Figure 9). After an additional 20 seconds of light exposure for each tooth to ensure through and through hardening, occlusal contacts were evaluated and adjusted (Figure 10).
The identical technique was used to restore the maxillary right primary molars. The restored teeth are shown clinically 10 months after treatment in Figure 11 and Figure 12; they are shown radiographically in bitewing films before treatment (Figure 13) and 10 months after treatment (Figure 14).
Case 2
A 4-year-old boy had large disto-occlusal caries lesions of the mandibular primary first molars. The carious damage involved approximately one third of the distal half of both teeth with penetration close to the pulp spaces. Considering that these teeth needed to be retained for 6 to 8 years, stainless steel crown repair was recommended to the mother as the best treatment option, and she readily consented.
Treatment
Behavior guidance of the young patient during treatment was facilitated by using nitrous oxide and oxygen inhalation, along with earphones with children’s music for comfort and distraction. Each of the mandibular primary molars was restored with the following technique.
After local anesthetic injections and rubber dam placement (Figure 15), the marginal ridge was cut away using a water-cooled small-diameter diamond bur, revealing the caries lesion (Figure 16). A standard Class II preparation was cut and all carious tooth substance debrided with a slow-speed round bur.
The exposed mesial surface of the adjacent primary second molar was not carious. Without a matrix strip, Vitrebond Plus liner was injected to fill the preparation (Figure 17). Excess liner was cut away during tooth preparation. With a high-speed water-cooled diamond bur, the molar was “miniaturized” in such a way that the selected preformed stainless steel crown would replace that which was lost to caries and tooth preparation (Figure 18).2 The proper sized crown was selected by comparing the mesial/distal size of the tooth on the preoperative bitewing film with sizes of available crown forms.
Once the correct crown form was selected, the margins were cut to proper length with a straight diamond wheel (Figure 19). Proper crown height was determined by aligning marginal ridges of the adjacent second molar. Marginal crimping was initiated using flat-beaked pliers to bend the edges of the crown form inward a bit, replicating the original anatomical form of the molar (Figure 20). The crimped margins are designed to engage the cut axial surfaces of the tooth and maximize retention of the cemented crown form. Additional “mini” crimping was achieved with a heatless stone spinning counterclockwise, followed by smoothing of the margins with a rubber wheel (Figure 21). Figure 22 shows a comparison of the crown form as supplied by the manufacturer with a manipulated crown ready for cementation.
The crown form was filled with RMGI luting cement, and pressed firmly into place with a mirror handle (Figure 23). The spatula handle also can be used for this purpose. Excess cement was cleared away with an explorer and a small-tipped Hollenback carver. Interproximal cement excess was cleared away while still somewhat soft using a knotted double strand of dental floss (Figure 24). Knotted floss or dental tape is most helpful to engage and expel hardened particles of cement that are loosened with the hand instruments. The stainless steel crown was photographed 1 year after treatment and is shown in Figure 25.
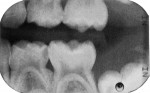
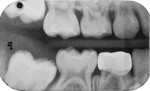
The left primary first molar was also restored using the same method. The left primary second molar did have a small mesial carious lesion that was observed during preparation of the first molar. Prior to crown cementation, the second molar was repaired using direct access RMGI restorative cement (Ketac Nano). A wooden wedge was used to control bleeding. The three restored molars are shown on bitewing films preoperatively in Figure 26 and Figure 27 and 1 year after treatment in Figure 28 and Figure 29.
Discussion
RMGI restorative cement has all the advantages of other glass-ionomer systems. These include chemical bonding to dentin and enamel; a coefficient of thermal expansion similar to that of tooth structure; fluoride ions in the calcium alumino-fluro-silicate glass particles that are released into the tooth structure, rendering it less soluble to acid challenge; injectability for easy application; tooth coloration; and good biocompatibility. In addition, inclusion of the photo-polymerizable resin component enhances its physical properties when compared with conventional glass-ionomers and allows for rapid light-hardening of the material.
Since the early 1990s, RMGI materials have proven most useful for primary teeth and in certain applications for permanent teeth as well.3 Ketac Nano was introduced in 2007. Its inclusion of nanoparticles and nano “clusters” further improved RMGI’s physical properties, natural appearance, and polishability. In a retrospective study of 684 restorations using Vitremer™ (3M ESPE) RMGI restorative material, a success rate of 94% was observed after 4 years.4 Although no similar study has been performed evaluating the nano-ionomer, the authors logically assume that results would be as good or better because the physical properties of Ketac Nano exceed those of Vitremer. The authors' combined clinical experience since 2007 has shown this to be true anecdotally, but scientific verification would be welcome.
One may question the use of a RMGI liner underneath the nano-ionomer. A Class II preparation being restored with the nano-ionomer is not routinely lined.5 In case 1, however, caries penetration was excessive and pulp spaces were nearly exposed. Because the liner flows easily and saturates the exposed dentin completely, the authors felt that an extra layer of protection for the pulp was warranted. Ruiz and Mitra succinctly documented the advantages of a RMGI liner, citing its high fluoride content, chemical bonding properties, biocompatibility, and proven ability to eliminate postoperative tooth sensitivity.7 Indirect pulp therapy in primary molars that includes use of a RMGI liner has been shown to have higher long-term success and lower cost than pulpotomy when treating reversible pulpitis.8 In the stainless steel crown procedure in case 2, use of the liner as an internal filling material in the disto-occlusal region not only assures good coverage of the deeply exposed dentin, but also facilitates crown preparation. With the liner in place, the clinician has a “full” tooth to visualize during crown cutting and concern about air voids during cementation is obviated.
Although the manufacturer of Ketac Nano recommends applying the primer for 15 seconds, air drying it, and then light-curing for 10 seconds before injecting the nano-ionomer, the first author has restored primary molars without curing the primer separately before injection of the cement. There has been no apparent difference in performance using that method. An in vivo study would be useful to determine scientifically if the 10-second primer light-curing step is necessary.
Another recommendation by the manufacturer is to layer the injected cement in increments of 2 mm or less. After experimenting with restored then sectioned extracted teeth, the authors have found that a high-energy visible light beam (1,200 mW mm2) actually hardens the nano-ionomer to a depth of 4 mm. Layering in 2-mm increments as the manufacturer suggests, however, remains the best way to ensure through and through hardening.
The preformed stainless steel crown for restoration of significantly damaged primary molars is the most durable and reliable method of tooth repair in the primary dentition. When accomplished well, with adequate pulp protection, stainless steel crowns are a virtual guarantee to the dentist that the treated tooth will not require additional attention until exfoliation or necessary extraction.2
When selecting the best size crown form, the goal is to pick one that recreates proximal contacts and occlusal relationships and functions as closely as possible to the original anatomical crown. If the selected crown does not seat easily, either the crown form is too small or the tooth was not prepared sufficiently. In some cases, both factors are involved. Evaluating crown size on a bitewing radiograph is helpful, but once a clinician develops experience with stainless steel crowns, rapid crown size selection is easily achieved by trial and error.
Final Thought
With all their advantages, stainless steel crowns sometimes pose one major practical difficulty: certain parents object to the silver appearance. New high-strength, preformed zirconia anterior and posterior crowns have come to the dentistry marketplace and give promise of a solution to the color problem.9 These crowns challenge the dentist to make precision marginal fit and to cement them in a field of bleeding gingiva, but methods of doing so will undoubtedly evolve.
Whether the molar zirconia crowns will be able to hold up for the long term against the functional forces germane to posterior teeth is currently unknown. However, in our experiences, when advised of the advantages of posterior stainless steel crowns, most parents readily accept them as the best alternative. In addition, the young girls seem to enjoy their “princess” teeth, and the boys show off their “Superman” molars to their pals.
Disclosure
Theodore P. Croll, DDS, has financial interest in the Strip T matrix system by virtue of a patent licensing agreement with Denovo Dental.
References
1. CR Foundation. Tooth repair for children and teens: best materials and techniques. Gordon J. Christensen Clinicians Report. 2011;4(9):1,3-4.
2. Croll TP. Preformed stainless steel crowns: an update. Compend Contin Educ Dent. 1999;20(2):89-106.
3. Nicholson JW, Croll TP. Glass-ionomer cements in restorative dentistry. Quintessence Int. 1997;28(11):705-714.
4. Croll TP, Bar Zion Y, Segura A, Donly, KJ. Clinical performance of resin-modified glass ionomer cement restorations in primary teeth. A retrospective evaluation. J Amer Dent Assoc. 2001;132(8):1110-1116.
5. Killian CM, Croll TP. Nano-ionomer tooth repair in pediatric dentistry. Pediatr Dent. 2010; 32(7):530-535.
6. Croll TP. Alternative methods for use of the rubber dam. Quintessence Int. 1985;16(6):387-392.
7. Ruiz JL, Mitra S. Using cavity liners with direct posterior composite restorations. Compend Contin Educ Dent. 2006; 27(6):347-351.
8. Coll JA. Indirect pulp capping and primary teeth: is the primary tooth pulpotomy out of date? Pediatr Dent. 2008;30(3):230-236.
9. CR Foundation. Pediatric crowns are growing up. Gordon J. Christensen Clinicians Report. 2012;5(11):1,3-4.
About the Author
Theodore P. Croll, DDS
Private Practice, Pediatric Dentistry
Doylestown, Pennsylvania
Affiliate Professor, Department of Pediatric Dentistry
University of Washington School of Dentistry
Seattle, Washington
Adjunct Professor, Pediatric Dentistry
University of Texas Health Science Center at San Antonio Dental School
San Antonio, Texas
Constance M. Killian, DMD
Private Practice, Pediatric Dentistry
Doylestown, Pennsylvania
Adjunct Associate Professor of Pediatric Dentistry
University of Pennsylvania
Philadelphia, Pennsylvania