CT Scanning in Implant Placement
Used in critical anatomic situations and for placing implants in an ideal position in bone, CT scanning software eliminates possible manual placement errors and matches planning to prosthetic requirements.
Timothy Kosinski, DDS; Mark Langberg, DDS
CT scanning software is an incredible tool for determining implant position and placement. Using a computer, implants can now be placed virtually in the ideal position before the patient is ever touched, making surgical placement of implants less invasive and more predictable. Prosthetic reconstruction is made simpler because implants are ideally angled.1
The fabrication of any stable maxillary removable appliance begins with careful diagnosis and case planning. Regardless of the patient’s age, it is imperative that his or her concerns and desires be taken into account in order to make the final prosthesis acceptable. Improving form and function can be a difficult challenge in any complete denture situation, and fortunately implants have provided an outstanding treatment option for dramatic improvement in denture stability and increased chewing ability. Endosseous implant designs have proven to offer an outstanding prognosis and are reliable as retainers for overdentures.1
Case Report
The patient was a 79-year-old man who had worn a conventional complete maxillary denture opposing reconstructed mandibular natural teeth for many years. He suffered from cardiovascular disease, so he experienced shortness of breath upon mild exertion. No other significant medical findings were indicated. The patient was unable to function properly with his existing denture because of a severe gagging reflex, and so he sometimes simply did not use his upper appliance. Form and function had diminished over the years.
Several options were discussed with the patient, including an attempt at a new conventional case. After deliberation, it was determined that it was worth trying to gain stability of the maxillary prosthesis using dental implants to retain a palateless denture.
The patient had obvious anxiety concerning surgical intervention and even the possibility of being a candidate for implants because of observable bone loss. Because of the facial resorption in the maxilla, it was decided to restore the patient’s upper arch using the Straumann® Dental Implant System (Straumann, www.straumann.us). In the author’s opinion, reliability and innovation are two strong qualities of the Straumann surgical and prosthetic techniques that made this the implant of choice in this situation. The implant provides an 8° Morse taper internal connection, and the flared neck implant design is ideal for soft tissue contouring.
There are often concerns with any surgical procedure, especially in the sinus area or in bone where nerves are located.2 These concerns have popularized a newer concept in implant dentistry.3 Implant planning software can now be used to visualize the patient’s entire mouth anatomy in three dimensions, often in less than 10 minutes. The computer software accurately simulates the placement of implants before ever touching the patient. A surgical guide, created from the 3D images, helps the clinician to place the implants in the proper positions, often without ever making a flap incision. This technique is a cost-effective solution to assist in planning an esthetic and functional final result and minimizing any surgical challenges.
Implant planning technology is based on planning algorithms used clinically for more than 11 years.4,5 CT scans and 3D planning software can improve predictability and safety. Techniques can be used for single-tooth edentulous spaces, single-tooth immediate extraction cases, partially edentulous spaces, fully edentulous maxillary and mandibular overdenture cases, or fully edentulous maxillary or mandibular full-arch permanent restorations. The surgical cases are, therefore, driven by the final esthetic and functional result. It is important to listen to the patient carefully to determine his or her goals and desires and design the implant reconstruction accordingly. It is critical to make sure that the final tooth reconstruction is established before any surgical intervention. Placing implants before understanding tooth–implant position and the final result is a big mistake.
Implant planning and placement software provides a high level of comfort and safety for the patient by reducing surgical and restorative time by using an accurate 3D plan before implant placement.1 There are obvious advantages, including: easy visual understanding for clear case presentations; reduced surgical chair time; reduced restorative chair time in certain cases because of ideal implant positioning; reduced stress for the clinician and the patient; the avoidance of surprises during surgery; optimal implant placement for long-term implant and prosthetic success; and, most importantly, an improved esthetic result.2
Before the CT scan, a radiographic guide is fabricated, which aids in visualizing the optimal prosthetic outcome. The teeth are positioned properly in wax and then a hard model to illustrate what the case will look like finished, before it even begins. All appropriate dental anatomy is included. The radiographic guide is placed in the mouth during the CT scan. This allows the clinician to see the ideal position of the teeth on a 3D model. The entire 3D image is analyzed, and the planning and simulation of placement is completed using the computer. The surgical placement of the implants can be done in a conventional manner using the newly created surgical guide to help direct the implants in the ideal position, but surgery can often be completed without making any incisional flap.2 The implants are placed in the desired depth using the computer software and the surgical guide.
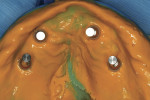
It is imperative that the implants be placed parallel to the long axis of the bone and to each other. In this case, a clear surgical guide was fabricated using the information created using the CT scanning software. The guide was used to correctly position the implants in the first molar and cuspid areas to maximize stability of the final implant-retained prosthesis. No retraction of the soft tissue was needed, since the CT indicated in three dimensions the length and width and position of the implants to be used.
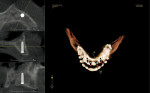
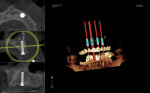
Figure 1 and Figure 2 illustrate the closed vertical dimension of occlusion resulting in improper lip support and a poor frontal and lateral esthetic profile. It is possible that the patient’s decrease in function was a result of the poor plane of occlusion and tooth position. Gagging was caused by the basic design of the conventional denture and poor fit. Figure 3 and Figure 4 show how the CT scanning software was used to virtually place the four implants, their angulation, and how the implants would be restored. To achieve the best functional and esthetic result, as well as increase stability of any prosthesis, it was decided to parallel the implants and place them in the cuspid area and as posterior as the bone would allow.
Before the preparation of the osteotomies, the surgical guide was created with aligning chambers which would allow the various size drills to penetrate the stent, through the soft tissue into the bone to the predetermined depth. The stent depth and tissue depth was compensated for in this process. No tissue flap was needed. Figure 5 shows this guide with aligning chambers. Various-width keys were placed into the aligning chamber to guide the initial 2.2-mm pilot drill (Figure 6 and Figure 7 ). The drills were used at approximately 800 rpm to the hub of the bur. No error can occur if the surgical guide is stable. Remember, the depth into bone has been determined by the CT scanning software. Soft tissue depth has been compensated for. All angles are also predetermined with the virtual placement of the implants.
All four implants in the first molar and cuspid areas were drilled to 10 mm. Implant site preparation continued with a 2.8-mm pilot drill to the 10-mm depth. A Straumann Standard Plus 3.3-mm X 10-mm implant was threaded into place in the area of tooth No. 10 only; 4.1-mm X 10-mm implants were threaded into the areas of teeth Nos. 3, 6, and 14 . The implants were ratcheted into their final position (Figure 8 ). Figure 9 illustrates the parallel position of the implants. The shoulder of the implant is left slightly coronal to the crestal bone to allow for easy access, and 1.5-mm closure screws were placed into each implant (Figure 10 ). The radiograph (Figure 11 ) demonstrates good bone adaptation around the implants. After 3 months of integration, the tissue around the closure screws were pink and firm (Figure 12 ). A closed custom-tray impression of the implants was made using the Straumann impression cap and synOcta positioning cylinders (Figure 13 ). A master impression was sent to the laboratory to have the proper analogs placed into the impression and placed into the impression for a master model pour up. The master cast was poured duplicating all peripheral borders. A bite registration was used to position the casts.
In this case, Locator® (Zest Anchors, www.zestanchors.com) attachments were intended to act as retentive devices for overdentures. Because of their design, the patient is able to easily align and seat the overdentures easily. It is important, however, that the implants be placed in a parallel position to each other, to simplify the prosthetic construction. According to the manufacturer, the attachments resist wear and maintain satisfactory retention for up to 56,000 cycles of function. Only 3.17 mm in total height, it is appropriate to use in situations where occlusal clearance is an issue.6 The male portions can be easily changed chairside with minimal inconvenience to the patient. The Locators come in a variety of retentions from extra light (blue) to heavy (clear). In this case, the average-retention orange attachment was used (Figure 14 ). The Locator attachment position can be attached to a stable record base using pick-up caps. Conventional denture techniques were used to create the final esthetic contours. In this case, the gagging reflex caused by the old full palate conventional complete denture was totally eliminated (Figure 15 , Figure 16 , Figure 17 , Figure 18 ).
This type of prosthesis allowed for excellent retention and stability for this patient. The Locator attachments are positioned extracoronally to allow for good tissue adaptation and easy maintenance with a toothbrush or end-tuft brush. If manual dexterity becomes a concern, the implants can be maintained at home using a washcloth or cotton applicators. Follow-up care includes clinical assessment for abutment stability, mobility of the implants, and plaque accumulation. Because the perimucosal seal is vital to protecting the underlying connective tissue and borne from migrating forces, probing a healthy implant is not advised. Radiographs are taken yearly to determine bone position and contour. Metal scalers and ultrasonic instruments may damage the titanium abutment surface; therefore, plastic, gold, or graphite scalers should be used as necessary.
This patient exhibited a positive end result because of his understanding of the limiting factors involved in this case and the final prosthesis. He is, however, able to chew more efficiently and speak clearly without worry of the prosthesis loosening or any of the abutments decaying. The gagging reflex he experienced before treatment was totally eliminated, and his quality of life was dramatically improved.
The general dentist has an obligation to provide patients with the most innovative, proven techniques available. CT scans and scanning software makes surgical placement of implants rather routine. Anatomical anomalies are virtually determined before ever touching the patient. With better implant placement comes more routine and predictable prosthetic reconstruction. Because the general practitioner is the professional the patient consults concerning their dental condition, all clinicians must educate themselves on the newest treatment modalities. Many surgical therapies can be performed by the trained general dentist and certainly all general dentists should be able to restore these cases simply and easily.
References
1. Fortin T, Bosson JL, Coudert JL, Isidori M. Reliability of preoperative planning of an image guided system for oral implant placement based on 3 dimensional images: an in vivo study. Int J Oral Maxillofac Implants. 2003;18(6):886-893.
2. Fortin T, Bosson JL, Isidori M. Effect of flapless surgery on pain experienced in implant placement using an image guided system. Int J Oral Maxillofac Implants. 2006;21(2):298-304.
3. Widmann G. Accuracy of computer aided implant surgery. J Oral Maxillofac Implants. 2006;20:305-313.
4. Wanschitz F, Birkfellner W, Watzinger F, et al. Evaluation of accuracy of computer aided intraoperative positioning of endosseous oral implants in the edentulous mandible. J Clin Oral Implants Res. 2002;13(1):59-64.
5. Hurwitz J, Zuabi O. Accuracy of a computerized tomography guided template assisted implant placement system: an in vitro study. J Clin Oral Implants Res. 2009;20(10):1156-1162.
6. Data on file. Zest Anchors, Inc. Locator Overdenture Attachment. Escondido, CA.
About the Authors
Timothy Kosinski, DDS
Adjunct Assistant Professor
University of Detroit Mercy School of Dentistry
Detroit, Michigan
Mark Langberg, DDS
Private Practice
Southfield, Michigan