Esthetic Replacement of Maxillary Central Incisors Using Immediate Implants and Atraumatic Surgical Techniques
Douglas H. Mahn, DDS; Jose Aunon, DDS
Esthetic replacement of maxillary anterior teeth remains a great challenge in implant dentistry. Before crown fabrication, a natural and esthetic appearing gingival architecture must be developed. A crown can be only as esthetic as the surrounding gingiva permits.
Of particular concern has been the preservation of full gingival papillae and stable gingival margins.1,2 An understanding of the biologic width around implants is critical in the esthetic management of these tissues. The stability of the bone and gingival papillae between dental implants is influenced by the biologic width associated with implants.3 It is the microgap and the depth of implant placement that determines the amount of crestal bone remodeling.4-6
Furthermore, because implants may be adjacent to teeth or other implants, each with their own biologic width, the space between adjacent implants or teeth and implants also affects the height of the interdental bone crest.7 Given our current under-standing of the effects of interproximal bone, esthetic strategies for positioning interproximal contact of crowns relative to the interproximal bone have been developed.8
The biologic width can also be seen affecting the stability of the facial gingival margin and the esthetic outcomes of implant dentistry. Bone resorption after implant placement9 and implant position relative to the lateral alveolar bone10 has been reported to affect the stability of the gingival margin and lead to gingival recession. Thicker gingival biotypes have been noted to be more stable than thinner ones.11
Surgical procedures to develop lost bone support and natural gingival contours in the esthetic zone have been challenging.12-16 Because of the difficulty in re-creating a natural and esthetic architecture, preventing its loss seems prudent.17-19 Atraumatic surgical techniques and immediate implant placement have been used to preserve and develop esthetic soft-tissue profiles.17,20-22 A combination of these techniques have been shown to be successful in the development of esthetic soft tissue architecture around several adjacent implant sites in the esthetic region.23
This case report describes the replacement of hopeless maxillary central incisors with immediately placed dental implants. Atraumatic surgical techniques allowed for the preservation of natural gingival contours. These contours permitted restoration of the adjacent implants with highly esthetic restorations.
CASE REPORT
A 39-year-old woman, a nonsmoker, presented with the chief complaint of crowded and highly mobile central incisors. Teeth Nos. 8 and 9 were found to have resorbed roots and class II mobility (Figure 1 and Figure 2). After discussing the findings and treatment plan options, the patient agreed to have teeth Nos. 8 and 9 replaced with dental implants.
Profound local anesthesia was achieved using 7.2 mL of 2% lidocaine with 1:100,000 epinephrine. Incisions were made circumferentially around teeth Nos. 8 and 9 using a No. 15 surgical blade. Using periotomes and forceps, teeth Nos. 8 and 9 were carefully removed (Figure 3). Care was taken not to traumatize the surrounding soft tissues (Figure 4). The extraction sockets were carefully curetted and the socket walls were found to be intact (Figure 5). Implant osteotomes were prepared in site Nos. 8 and 9 using surgical implant drills with copious saline irrigation. Regular-diameter, 4-mm x 13-mm dental implants were placed (PrimaConnex®, Keystone Dental, Inc, Burlington, MA) (Figure 6). These threaded implants have resorbable blast media textured surfaces and internal prosthetic connections with medialized microgaps. Impression screws placed into each implant clinically confirmed the desired angulation of the implants (Figure 7). Healing abutments with 6-mm flares and 5-mm cuffs were placed on each implant (PrimaConnex® Healing Abutment, Keystone Dental, Inc) (Figure 8). Because of the slight gap between the healing abutments and the surrounding gingival margin, one 4.0 chromic gut suture was placed between the implants. Radiographs confirmed implant position and complete seating of the healing abutments (Figure 9). An interim removable partial denture was adjusted and delivered. No contact between the prosthesis and implants was present (Figure 10).
After 3 months of healing, the implant sites were found to be healing well (Figure 11). Removal of the healing abutments found the gingival cuffs to be free of inflammation (Figure 12). The 3-mm to 5-mm gingival cuffs did not show signs of collapse despite removal of the healing cuffs. The original soft-tissue contours and gingival papillae were maintained (Figure 13). The patient was referred for final restoration of the dental implants.
An open-tray technique was used to make an impression of the dental implants. UCLA abutments were used to fabricate custom abutments (PrimaConnex® Abut-ment, Keystone Dental, Inc). The abutments were secured to the implants and single-unit, porcelain-fused-to-metal crowns were cemented onto each implant (Figure 14). Radiographs confirmed complete seating of the abutments and crowns (Figure 15).
DISCUSSION
Because a high degree of esthetics was necessary for this case to be deemed successful, preservation of the natural and esthetic soft-tissue architecture was critical. In particular, maintenance of the interdental papillae was an important concern.
A classification developed by Salama et al8 identified the expected heights of papillae between different types of restorations. In their research, more esthetic results were achieved when adjacent implants were avoided. In their classification, predicted heights of interdental papillae between adjacent implants (3.5 mm) are significantly less when compared with those between an implant and a pontic (5.5 mm) and a tooth and an implant (4.5 mm).
Collapse of the interdental papillae and flattening of the osseous crest is expected when multiple teeth are simultaneously removed.17,18 Surgical procedures to reconstruct lost osseous support and scalloped gingival contours in the esthetic zone can be challenging.12-16 Preservation of the natural osseous and gingival architecture, therefore, is important to the success of an esthetic case.17-19
In this case, teeth Nos. 8 and 9 were removed as atraumatically as possible and dental implants were immediately placed into the sites. Immediate implant placement techniques and their ability to preserve esthetic soft-tissue profiles have been documented.17,20-22 In this case, the implants were placed along the palatal aspect of the extraction sockets. Their long axes directed lingual to the incisal edges of the crowns.24,25
In the case presented, the osseous and gingival architecture was managed in several ways. First, the adjacent implants were placed approximately 3 mm apart and 2 mm from the adjacent teeth, as measured at the osseous crest. The purpose of this treatment plan was to accommodate the expected bone remodeling that would be caused by the development of biologic width and to preserve the interdental papillae.7,8
Second, the implants used had medialized microgaps. The goal with medialized microgaps is to minimize the vertical component of the biologic width, thus preserving crestal bone heights that support the gingiva and interdental papillae.13,17
Third, the implants were placed so that their prosthetic tables would be approximately 4 mm below the facial gingival margin.26 Stock flared healing abutments were placed because they had esthetically contoured emergence profiles. By placing the implants deep to the gingival margin and using flared healing abutments, natural emergence profiles were developed. By not placing the implants too deeply, concerns regarding hygiene were averted. As expected, minimal gingival changes were found because the biotype was not thin.11
Cement-retained single-unit crowns were used to restore the implants in sites Nos. 8 and 9. To stabilize the gingival margins, the final abutments and crowns had natural emergence profiles.27,28 The interproximal contact points were positioned to create the appearance of full interdental papillae. The final results were highly esthetic.
CONCLUSION
Maxillary central incisors can be replaced successfully using dental implants. The use of atraumatic surgical techniques and immediate implant placement can preserve the natural soft-tissue architecture. With this foundation, highly esthetic restorations can be achieved.
DISCLOSURE
The author has no financial interest in, or relationship with, Keystone Dental, Inc.
References
1. Grossberg DE. Interimplant papilla reconstruction: assessment of soft tissue changes and results of 12 consecutive cases. J Periodontol. 2001;72(7):958-962.2. Chaoquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
3. Cochran DL, Hermann JS, Schenk RK, et al. Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontol. 1997;68(2):186-198.
4. Hermann JS, Schoolfield JD, Schenk RK, et al. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001;72(10):1372-1383.
5. Hermann JS, Schoolfield JD, Nummikoski PV, et al. Crestal bone changes around titanium implants. A methodologic study comparing linear radiographic with histometric measurements. Int J Oral Maxillofac Implants. 2001;16(4): 475-485.
6. Hartman GA, Cochran DL. Initial implant position determines the magnitude of crestal bone remodeling. J Clin Periodontol. 2004;75(4):572-577.
7. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4): 546-549.
8. Salama H, Salama MA, Garber D, et al. The interproximal height of bone: A guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998;10(9):1131-1142.
9. Small PN, Tarnow DP. Gingival recession around implants: A 1-year longitudinal prospective study. Int J Oral Maxillofac Implants. 2000;15: 527-532.
10. Grunder U, Gracis S, Capelli M. Influence of 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005; 25:113-119.
11. Maynard JG Jr, Wilson RD. Physiologic dimensions of the periodontium significant to the restorative dentist. J Periodontol. 1979;50: 170-174.
12. Matthews DP. Soft tissue management around implants in the esthetic zone. Int J Periodontics Restorative Dent. 2000;20(2): 141-149.
13. Nemcovsky CE, Moses O, Artzi Z. Interproximal papillae reconstruction in maxillary implants. J Periodontol. 2000;71(2):308-314.
14. Elian N, Cho SC, Froum S, et al. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-106.
15. Jovanovic SA. Bone rehabilitation to achieve optimal aesthetics. Pract Proced Aesthet Dent. 2007;19(9):569-576.
16. Rebaudi A, Giampiero J, Trisi P, et al. A new technique for bone augmentation and papilla reconstruction with autogenous free gingival-bone grafts. Int J Periodontics Restorative Dent. 2007;27(5):429-439.
17. Kan JYK, Rungcharassaeng K. Site development for anterior single implant esthetics: the dentulous site. Compend Contin Educ Dent. 2001;22(3):221-232.
18. Kan JYK, Rungcharassaeng K. Interimplant papilla preservation in the esthetic zone: a re-port of six consecutive cases. Int J Periodontics Restorative Dent. 2003;23(3): 249-259.
19. Spear FM. Maintenance of the interdental papilla following anterior tooth removal. Pract Periodontics Aesthet Dent. 1999;11(1): 21-30.
20. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9(5): 332-343.
21. Zeren KJ. Minimally invasive extraction and immediate implant placement: the preservation of esthetics. Int J Periodontics Restorative Dent. 2006;26(2):171-181.
22. Canullo L, Rasperini G. Preservation of peri-implant soft and hard tissues using platform switching of implant placed in immediate extraction sockets: a proof-of-concept study with 12- to 36-month follow-up. Int J Oral Maxillofac Implants. 2007;22(6): 995-1000.
23. Mahn DH. Development of natural soft tissue architecture and interdental papillae be-tween adjacent implants in the aesthetic zone. Pract Proced Aesthet Dent. 2008;20(4):249-255.
24. Lazarra RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26(1):9-17.
25. Saadoun AP, Le Gall M. Selection and ideal three-dimensional implant position in the anterior aesthetic zone. Ing Magazine Oral Implantol. 2003;4(4):8-18.
26. Funato A, Salama M, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007:27(4):313-323.
27. Saadoun AP, Le Gall M, Toutai B. Current trends in implantology: part II—treatment planning, aesthetic considerations, and tissue regeneration. Pract Proced Aesthet Dent. 2004;16(10):707-716.
28. Saadoun AP, Toutai B. Soft tissue recession around implants: is it still unavoidable?—Part II. Pract Proced Aesthet Dent. 2007;19(2):81-88.
 Figure 1 Facial view of maxillary central incisors. Rotation and crowding of teeth was evident.  |  | |
| Figure 3 The extracted teeth showed highly resorbed roots. | Figure 2 The periapical radiograph showed severe root blunting of teeth Nos. 8 and 9. The roots of teeth Nos. 7 through 10 were in close proximity. | |
 |  | |
| Figure 4 Atraumatic extraction techniques left the surrounding gingiva and interdental papillae intact. | Figure 5 Examination of the extraction sockets found all osseous walls to be intact. | |
 |  | |
| Figure 6 Dental implants were immediately placed into the extraction sites. The internal connection was identified easily. | Figure 7 Impression screws placed into the implants verified proper and parallel implant placement. | |
 | 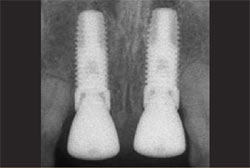 | |
| Figure 8 Healing abutments with 6-mm flares and 5-mm cuffs were placed on the implants. A suture was placed to secure close adaptation of the gingiva. | Figure 9 Radiographic confirmation showed implant position and complete seating of the healing abutments. | |
 |  | |
| Figure 10 No contact was present between the healing abutments and the interim removable partial denture. | Figure 11 After 3 months of healing, the implants sites were found to be healing well. | |
 |  | |
| Figure 12 When the healing abutments were removed, the gingival cuffs were found to be healthy and free of inflammation. | Figure 13 The facial view shows natural and esthetic soft-tissue architecture. The gingival papillae showed no signs of blunting. | |
 |  | |
| Figure 14 The facial view of the final restorations. The implants were restored with screw-retained abutments and cement-retained crowns. | Figure 15 A radiograph of the final restorations shows stable interproximal bone. The abutments and crowns are fully seated. The restorations have a natural emergence profile. | |
| About the Authors | ||
 Douglas H. Mahn, DDS Douglas H. Mahn, DDS Private Practice Manassas, Virginia | ||
 Jose Aunon, DDS Jose Aunon, DDS Private Practice Centreville, Virginia | ||




