Done in a Day: Immediate Tooth Replacement with Definitive Prosthesis
Mickel A Malek, DDS
Research of root form implants has advanced surgical protocol comprising two stages, to a one-stage procedure, to immediate loading with provisionaliztion. This article covers the final step of this journey toward simplifying implant placement. In the two cases presented, a protocol of immediate placement and definitive restoration is described. With this technique, the clinician can extract a tooth and replace it with an immediately functioning definitive prosthesis, hence completing the whole process in one single dental visit.
Dental implant therapy has progressed considerably over the last decade. Single-tooth implants have become the gold standard of care for replacing missing teeth. The predictability and elimination of the need to prepare adjacent teeth with this method thus increase the efficiency of oral hygiene.1 Implant stability, as dictated by the quality of the surrounding bone and its subsequent effect on its survival, was the main focus of the surgeon. The most dramatic advance in improving implant treatments was the implant surface evolution from machined/polished to rough-textured surfaces.2 Moreover, the mastery of routine-guided tissue regeneration procedures has elevated the degree of confidence in osteointegration and allowed clinicians to shift their emphasis to the final esthetics outcome. Today, many protocols exist to enhance the esthetic outcome of the prosthetic component of implant dentistry. The concept of site preservation, where the height and width of the alveolus is preserved through socket grafting for the purpose of maintaining favorable tissue contour, is one way to enhance the desired appearance of the prosthetic crown. Another protocol calls for the immediate placement of the implant with the rationale that the buccal-lingual dimension of the extraction socket is preserved and bone resorption is reduced.3 This traditional two-stage surgical procedure was eventually modified to become a single stage, where a healing abutment allowed the implant platform to communicate directly with the oral cavity, thus supporting the free gingival tissue and limiting the potential for posttreatment shrinkage.4,5 The unpredictable gingival recession and crestal bone resorption are among the disadvantages linked to the duration of the treatment; hence, research continues to point to shorter, more definitive courses of treatment.6 Ultimately, researchers concluded that the single most critical factor that correlated to the preservation of the soft tissue architecture and, eventually, the ideal esthetic outcome was the duration and the steps involved in any particular treatment.7 It is the author’s opinion that, when it comes to ideal esthetics, where the restoration must mimic its replacement and be indistinguishable from its surroundings, immediate implant placement and definitive restorations have become the coveted treatment of choice. One of the undeniable benefits is the ability to compress 12 months of treatment into a single dental visit. This procedure uses the concept of implant stabilization, where the immediate loading of the implant becomes possible. A coefficient of friction is assumed at the bone-implant interface that becomes the basic influence on forced transmission that is concentrated in the peri-implant bone, taking advantage of the fact that micro-motion of less than 30 micro-strains at the implant-bone interface can be beneficial in the promotion of osteogenesis and mature bone formation.8,9 When this approach is joined with the seating of a definitive prosthesis, the practice of provisionalization is skipped, thereby eliminating all of the instabilities and adversities associated with maintaining proper biological width, which is often invaded with multiple prosthetic procedures. Not only does this procedure drastically reduce morbidity by eliminating multiple surgical procedures, it incorporates the advancement of osseointegration and plastic soft tissue surgery. Perhaps the ultimate beneficiary of this procedure is the patient who can come in and have a hopeless tooth extracted and a definitive tooth replaced in the same visit, without the need for further treatment.
CASE PRESENTATIONS
The following case presentations demonstrate a step-by-step protocol that allows the clinician to remove a hopeless tooth and replace it with a fully functional, implant-supported crown.
Case 1
A 40-year-old female in good general health presented with a peri-apically involved maxillary incisor resulting from a failed root canal (Figure 1A and Figure 1B). Treatment options were reviewed and informed consent was obtained. Based on the patient’s desire to reduce trauma and treatment time, it was decided to perform immediate implant placement with a definitive restoration after tooth extraction.
Surgical Protocol
A local anesthetic of lidocaine with epinephrine was administered. Avoiding the reflection of a flap, osteotomes were used to perform an atraumatic extraction (Figure 1C and Figure 1D). Maximum care must be taken to avoid the fracture of the buccal plate. This can best be accomplished by pinching the ridge between the thumb and index finger, using light pressure to detect any micro-movement of the underlying bone. The socket and lamina dura were aggressively debrided to promote bleeding points. The osteotomy began with an initial pilot hole on the most apical part of the lingual wall with a line of draw bisecting the mesial-buccal and distal-lingual dimension of the socket (Figure 1E and Figure 1F). The osteotomy was completed in accordance with the manufacturer protocol and in reference to the adjacent teeth cemento-enamel junction (CEJ). The implant was torqued until it achieved 35 Ncm, and its platform was 5 mm apical to the adjacent central CEJ. The diameter of the implant platform at that depth intimately approximated all bony walls. This placement allowed the implant abutment connection to be 5 mm apical of the antici-pated gingival margin (Figure 1F).10
Restorative Protocol
Once proper torque was achieved, the definitive ceramic abutment was prepared to facilitate the design of a CAD/CAM restoration. The abutment can optionally be prepared outside the oral cavity to allow for a 2-mm shoulder to meet the requirements of a CAD/CAM restoration (Figure 1G). The ridge was dusted, and an optical impression was taken according to CEREC® 3D (Sirona Dental Systems, Inc, Charlotte, NC) specifications (Figure 1H). After the desired design of the restoration was completed, it was conveyed to the manufacturing unit and a crown was milled out of a feldspathic block.
The crown was tried in for the verification of the contacts (Figure 1I). Minimal adjustment was necessary to eliminate any traumatic occlusion. After verification of the fit and occlusion, the ceramic was glazed in a furnace. The interior was then sandblasted and primed with a salinated material. The ceramic abutment was primed with a zirconium material, and resin cement was deployed for the seating of the definitive restoration (Figure 1J). Six months postoperatively, the interproximal bone level showed no change from the date of implant insertion. The gingival height of the restoration continues to mimic that of the original tooth (Figure 1K).
Case 2
A 27-year-old woman presented with a symptomatic maxillary left lateral incisor with a history of endotherapy with a core build-up and crown. Clinical evaluation revealed evidence of active infection and a perilous fistula and exudate at the gingival margin (Figure 2A and Figure 2B). The prognosis of the tooth was deemed hopeless.
Surgical Protocol
Atraumatic care was again taken to preserve the buccal plate. With the use of the osteotome, the root was delivered (Figure 2C and Figure 2D). The socket was debrided, and accomplished without flap reflection to preserve the interproximal papillae and the remaining buccal and lingual plates of bone. After socket debridement, the implant was guided into position for ideal prosthetic placement, and primary stability was achieved with the implant platform 3 mm apical to the anticipated free gingival margin (Figure 2E and Figure 2F). The implant was placed to project with a bias toward the lingual wall, to achieve primary stability. An Astra-type root form implant was used specifically for its flared design at the collar to allow intimate approximation to all bony walls. Thirty-two Ncm stability was achieved for the stability of the implant; a ceramic abutment was selected to meet the desired prosthetic dimension and torque to 25 Ncm per the manufacturer’s recommendation (Figure 2G).
Restorative Protocol
The prosthetic abutment was modified to allow for the design and placement of the CAD/CAM restoration (Figure 2H). After the optical impression for the acquisition unit, the design was finalized and relayed to the milling unit. After fit and occlusion verification, the ceramic was once again glazed in a furnace (Figure 2I). The interior was sandblasted and primed with a salinated material, the ceramic abutment was primed with a zirconium material, and resin cement was deployed for the seating of the definitive restoration (Figure 2J and Figure 2K).
DISCUSSION
Osteointegration of implants has been the standard by which implant survival and its success has been measured. In the esthetic zone, however, the key to successful implant restoration is the degree of preservation of the hard and soft tissue complex. After tooth loss, soft tissue shrinkage and bone resorption degrades this complex over time. For this reason, it is best to attempt implant placement, so long as the distance between the bony walls and the implant is less than 2 mm, so as to avoid the necessity for grafting.11 By placing the implant at least 3 mm from the anticipated free gingival margin, as described in the literature, better approximation of the bony walls can be achieved as the socket constricts in diameter. Furthermore, placement of the abutment?implant platform at this level is not only favorable for the biological width, but also for the creation of a contact point, no greater than 5 mm from the crest of bone, to prevent the collapse of the interproximal papillae.12 As the previous cases demonstrate, the contour of the restoration allowed the soft tissue to maintain position and prevent the sulcus from collapsing, and maintained the buccal soft tissue.
CONCLUSION
By combining the latest advancement in atraumatic extractions and immediate rough surface implant placement with the use of CAD/CAM in-office restorations, the natural hardened soft tissue complex was best preserved. In both cases presented above, this gingival level was maintained or demonstrated stability 9 months after implant placement. Moreover, time and morbidity was dramatically reduced. The satisfaction and enthusiasm of a patient who can condense a complex procedure traditionally requiring several visits into just one, not to mention the financial windfall in terms of reduced overhead to the providing clinician, testify to the benefits of this protocol.
References
1. Millennium Research Group. US markets for dental implants: executive summary. Annual industry report. Implant Dent. 2003;12(2):108-111.2. Georgiopoulos B, Kalioras K, Provatidis C, et al. The effects of implant length and diameter prior to and after osseointegration: a 2-D finite element analysis. J Oral Implantology. 2007;33(5):243-256.
3. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodent Rest Dent. 1989;9(5):332-343.
4. Froum SJ. Immediate placement of implants into extraction sockets: rationale, outcomes, technique. Alpha Omegan. 2005;98(2):20-35.
5. Parel SM, Triplett RG. Immediate fixture placement: a treatment planning alternative. Int J Oral Maxillofac Impl. 1990;5(4):337-345.
6. Norton MR. A short-term clinical evaluation of immediately restored maxillary TiOblast single-tooth implants. Int J Oral Maxillofac Impl. 2004;19(2):274-281.
7. Chen ST, Wilson TG Jr, Hämmerle CH. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Impl. 2004;19(Suppl):12-25.
8. Chereli M, Sahin S, Akca K. Role of mechanical environment and implant design on bone tissue differentiation; current knowledge and future contexts. J Dent. 2004;32(2): 123-132.
9. Meyer U, Wiesmann HP, Fillies T, Joos U. Early tissue reaction at the interface of immediately loaded dental implants. Int J Oral Maxillofac Implants. 2003;18(4):489-499.
10. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodont Rest Dent. 2005;25(2):113-119.
11. Paolantonio M, Dolci M, Scarano A, et al. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J Periodontal. 2001;72(11): 1560-1571.
12. Grunder U. Stability of the mucosal topography around single-tooth implants and adjacent teeth: 1-year results. Int J Periodont Rest Dent. 2000;20(1):11-17.
 |  | |
| Figure 1A Preoperative retracted smile. | Figure 1B Preoperative radiograph. | |
 |  | |
| Figure 1C Gentle luxation. | Figure 1D Atraumatic slow rotary extraction motion. | |
 |  | |
| Figure 1E Initiation of pilot drill. | Figure 1F Radiograph of inserted fixture. | |
 | 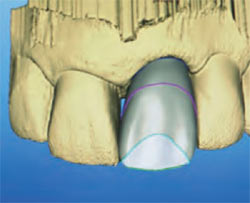 | |
| Figure 1G Ceramic esthetic abutment. | Figure 1H Virtual restoration ready for milling. | |
 |  | |
| Figure 1I Crown try-in. | ||
 | ||
| Figure 1J Seated glazed prosthesis. | Figure 1K Six-month postoperative view. | |
 |  | |
| Figure 2A Pretreatment radiograph. | Figure 2B Perilous lesion. | |
 |  | |
| Figure 2C Gentle subluxation. | Figure 2D Rotary motion root extraction. | |
 |  | |
| Figure 2E Osteotomy initiation. | Figure 2F Final drill sequence. | |
 |  Figure 2H Ceramic abutment torqued to 35 Ncm.  | |
| Figure 2G Radiograph of seated root form fixture. | Figure 2I Glazed, characterized restoration. | |
 Figure 2J Cleaning of excess cement. |  | |
| Figure 2K Radiograph 30 days postoperative. | ||
| About the Author | ||
 Mickel A Malek, DDS Mickel A Malek, DDS Comprehensive Advanced Aesthetic Dental Practice Smile Dental Spa Tucson, Arizona | ||



