Improving Mandibular Denture Retention with Mini-Implants
Gregori M. Kurtzman; Douglas F. Dompkowski
Mini-implants have become a common treatment option for improving retention of lower dentures.1-3 They can provide improvement in the patient’s quality of life when traditional implant treatment is not within the patient’s financial means.
Patients are now living longer, and they expect a higher quality of life as they age. As nutrition is tied to masticatory ability, patients with poorly retained mandibular dentures may suffer from nutritional deficiencies because of their inability to chew food. With a decrease in nutrition, the patients’ general health is affected and their quality of life suffers.4-6 This can be corrected with improved denture retention, allowing patients to improve their diet.
The immediate-load nature of mini-implants gives patients immediate satisfaction without delays in treatment to accommodate conventional healing, permitting full osseointegration.7-9
Case Report
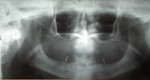
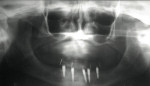
A 62-year-old woman with full maxillary and mandibular dentures presented at a recall appointment with a chief complaint of insufficient retention on the lower arch without a denture adhesive. The patient’s dentures had been fabricated within the previous 6 months. The patient wanted to eliminate the use of a denture adhesive and inquired about dental implants. A panoramic radiograph was taken (Figure 1) along with a clinical examination. It was determined that adequate osseous height and width were present to accommodate implant placement (Figure 2). Her finances were limited and the use of standard implants was not within her financial means.
Kromopan™ alginate (Kromopan, Des Plaines, IL) was mixed and placed into one half of a Lang Denture Duplicator (Lang Dental, Wheeling, IL), and the patient’s lower denture was placed tooth side down into the alginate and allowed to set. A second batch of Kromopan alginate was mixed and placed into the tissue side of the denture sitting in the lower half of the Lang Denture Duplicator. The upper half was filled with alginate, and the duplicator was closed, allowing the material to set. The duplicator was then opened, and the denture was removed from the alginate. Clear orthodontic acrylic (Lang Dental) was mixed to a thin consistency and poured into the mold formed in the duplicator, then closed and immersed in hot water. Immersion in hot water accelerates the set of the acrylic and provides a transparent denture replica when completed. After the acrylic set, it was removed from the duplicator, and flanges were adjusted to remove any flash of material. Vertical grooves were made on the buccal/facial surface at the ideal sites for implant placement, and then short pieces of wire were fixated in the grooves to act as radiographic markers. A panoramic radiograph was obtained, and the location of the mental foramina was identified in relation to the locations of the intended implants. Any modification of the implant locations relative to anatomic structures could be made at that time.
Placement of the implants in a fully edentulous arch without a stent to guide the process has the potential to position the implants too far buccal or lingual and hamper the esthetics of the prosthesis. The use of a duplicate of the patient’s denture allows the practitioner to know the outlines of the denture and permit placement of the implants within its confines, eliminating prosthetic complications, such as the retentive heads showing through or the bulging of the male retentive head in the denture.
Once the final implant locations were determined, the tooth at each implant site on the clear duplicate denture stent was ground to provide a flat horizontal area. Every implant site was adjusted on the stent so that there was a height of approximately 3 mm of acrylic between the crest of the ridge and the superior aspect of the horizontal area. A 3/32-inch twist drill was used to place a pilot hole through the clear stent into the underlying stone model. A paralleling pin was placed into this site, and the adjacent site was prepared using the twist drill to parallel the pin placed into the first site. A paralleling pin was then placed into the second site, and the process was repeated until a pilot hole was placed in all five sites (Figure 3).
The surgical stent was then tried in intraorally, and the occlusion opposing the maxillary arch was verified (Figure 4). Local anesthetic was administered via infiltration into the buccal vestibule from the distal of the far right implant position through the distal to the far left implant position. A 1.6-mm pilot drill was placed into a surgical headpiece, and then introduced through the surgical stent at each site, piercing the soft tissue and entering the crestal bone 3 mm to 4 mm with sterile water irrigation (Figure 5).
The surgical stent was removed; the perforation through the gingival tissue at the implant site in the anterior was identified; and the stationary pilot drill was used to explore the osteotomy at this location. The pilot hole was deepened to a depth not exceeding the length of the implant intended for that site (Figure 6). A paralleling pin was placed at this osteotomy site. Then the adjacent site was explored with the stationary pilot drill, and the process was repeated for this site (Figure 7). This was repeated for each site using the paralleling pins to align each of the five pilot holes.
Next, a 3-mm disposable tissue punch was pressed over each perforation to the osseous crest, and a gingival tissue plug was removed (Figure 8). Paralleling pins were replaced into the anterior implant sites. A 1.6-mm drill was introduced into the far right site and then prepared to the intended depth, paralleling the drill with the pins placed adjacently (Figure 9). The process was repeated at the next site, continuing until all sites had been prepared with the 1.6-mm drill to the desired depth and paralleled the other osteotomy sites. Because of the width of ridge available in this patient, 3.25-mm diameter fixtures were selected (in narrower ridges, a 2.2-mm diameter fixture may be selected).
Next, the countersink bur for the 3.25-mm ERA mini-implant (Sterngold Dental, Attleboro, MA) was used at each site. Because of higher bone density at the anterior three sites, it was necessary to use the 3.25-mm bone tap run at 45 Ncm and 20 rpm to allow placement of the anterior implants to the desired depth. The ERA driver was placed into the implant handpiece, and torque was set at 45 Ncm and a speed of 20 rpm. An ERA mini-implant package was opened, and the sterile titanium cylinder containing the ERA mini-implant was removed. The clinician slid the ERA Insertion Tool onto the hex area of the ERA attachment (gold nitrite-coated portion) and was removed from the titanium sleeve (Figure 10 and Figure 11). The implant was carried to the osteotomy site and, under irrigation, the implant was rotated apically until the surgical unit stopped at the present 45 Ncm or the correct depth was achieved (Figure 12).
If the desired depth was not achieved with the handpiece, a mini-ratchet wrench was placed fully on the ERA attachment of the mini-implant, and a clockwise rotation was applied until the implant reached the correct depth (Figure 13). The use of the mini-wrench vs a standard torque wrench decreased the forces placed on the mini-implant because of the shorter-level arm of the wrench and eliminated any deformation of the ERA attachment that may occur. Placement of the ERA mini-implants continued until all fixtures were placed, being careful not to exceed 60 Ncm of torque (Figure 14).
From the patient’s cast, a vacuform stent was fabricated. This was taken intraorally, and marks were made over each fixture location with a marker. A hole, which was the width of the implant, was made at each mark and taken back to the mouth to verify positioning. This stent was then inverted into the tissue side of the denture and a black mark made at each implant location to assist in the relief of the denture resin, to accommodate the ERA Micro OV (Sterngold Dental) metal housing. ERA Micro OV males in the metal housing were placed onto each fixture (Figure 15 ), and the denture was tried in to verify clearance (fit at this stage should be passive with no contact with the attachment housing). Pieces of non-latex dental dam with a central hole were placed over each mini-implant fixture and the ERA housing snapped down over the attachment (Figure 16). The dam acted as a block-out preventing any resin from getting between the implant and soft tissue during pick-up in the denture.
The denture was dried, and SternVantage Varnish LC primer (Sterngold Dental) was brushed onto each receptor site in the denture and light-cured for 1 minute. To aid in the clean-up of excess material, it is advisable to avoid placement of the primer in areas other than the receptor sites. ERA PickUp resin (Sterngold Dental) was expressed from an automix syringe into the receptor sites, being careful not to overfill each site (Figure 17 ). The denture was inserted intraorally, and the patient was guided into occlusion and allowed to set. The patient was instructed to keep her teeth together without excessive pressure to avoid tissue compression that could prevent engagement of the attachments upon reinsertion of the denture. As the anesthetized patient will lack proprioception at this stage, it is suggested that while waiting for the acrylic to set, a staff member should place a finger under the patient’s chin to help it remain closed. Upon setting, the denture was removed along with the pieces of dam placed earlier. As primer was not applied outside the receptor sites, the removal of excess material did not require the use of an acrylic bur, and the extra material could be flaked off with an instrument. A Micro ERA core-cutter bur (Sterngold Dental) was used to remove the black processor male in each housing, and a white ERA male was snapped into each location using a Micro ERA seating tool (Sterngold Dental) (Figure 18). The denture was then returned to the mouth and the retention was evaluated. Before dismissing the patient, a postoperative panoramic radiograph was taken to evaluate the implant positions (Figure 19).
Conclusion
Patients who present with lower full-arch dentures with poor retention may not be candidates for conventional implant treatment because of financial issues. The use of four to six ERA mini-implants can secure the denture and improve the patient’s quality of life while fitting within their financial budget.
Disclosure
The author has received an honorarium from Sterngold Dental.
References
1. Feine JS, Carlsson GE. Implant Overdentures: The Standard of Care for Edentulous Patients. Carol Stream, IL; Quintessence Publishing: 2003.
2. Misch K, Neiva R. Small-diameter implants for optimal stabilization of implant-supported overdentures. Pract Proced Aesthet Dent. 2007;19(7): 428-431.
3. Bulard RA. Mini implants. Part I. A solution for loose dentures. J Okla Dent Assoc. 2002;93(1):42-46.
4. Morais JA, Heydecke G, Pawliuk J, Lund JP, Feine JS. The effects of mandibular two-implant overdentures on nutrition in elderly edentulous individuals. J Dent Res. 2003;82(1):53-58.
5. Steele JG. National diet and nutrition survey people aged 65 years and over. Vol 2: Report of the oral health survey. London, UK: The Stationary Office, 1998.
6. MacEntee MI, Hill PM, Wong G, Mojon P, Berkowitz J, Glick N. Predicting concerns for the mouth among institutionalized elders. J Public Health Dent. 1991;51(2):82-90.
7. Nazarian A. Mini dental implants: immediate gratification for patient and provider. Dent Today. 2005;24(10):110-112.
8. Bulard RA. Mini dental implants: enhancing patient satisfaction and practice income. Dent Today. 2001;20(7): 82-85.
9. Ahn MR, An KM, Choi JH, Sohn DS. Immediate loading with mini dental implants in the fully edentulous mandible. Implant Dent. 2004;13(4):367-372.
About the Authors
Gregori M. Kurtzman, DDS
Private Practice
Silver Spring, Maryland
Douglas F. Dompkowski, DDS
Private Practice
Periodontics and Implant Dentistry
Bethesda, Maryland
Clinical Associate Professor
University of Maryland Dental School
Baltimore, Maryland