A General Practitioner’s Perspectives on Oral Cancer Diagnosis and Management
Scott D. Benjamin, DDS
Tufts University Symposium on ORAL CANCER part three
Dentists have a unique opportunity to make a difference in the quality of life and health for many people. The general practitioner treats some of the most common diseases affecting a majority of adults in North America: dental caries and periodontal disease. Over the years, significant advances have been made in the prevention, diagnosis, and treatment of these diseases. The dentist has at hand the appropriate equipment, technology, and education to address the needs of patients appropriately.
However, the dental practitioner is also on the front line of another disease: oral cancer. It is important that dentists and all oral health practitioners begin to recognize and become involved in efforts to improve the diagnosis and management of this critical disease. This is another opportunity to make a significant contribution to the health of many people.
The general population is not aware of their risk for oral cancer. Some educational materials from health and cancer organizations do not even include it in their list of common cancers. Most people are astonished to learn that oral cancer is the sixth most common cancer in the world1 (and the sixth most common cancer in US men2). Information and realization are the first steps in confronting this problem. All dental professionals need to initiate and be actively involved in this dialogue with their patients to raise public awareness of oral cancer and to educate everyone on the associated risk factors. Performing an enhanced comprehensive oral evaluation on all adult patients is imperative if we are ever going to be able to manage this horrible disease. This examination should be looking for anything abnormal, from a simple cheek bite to a malignancy, and should be performed at every hygiene visit. Awareness, education, and early detection are the foundation on which a change in this disease state can be made.
For example, women’s healthcare practitioners and advocates are better than the dental profession at disseminating essential information. The education and response to the threat of cervical cancer is a good example of what is possible. Women in the United States are now aware of their risk for cervical cancer and committed to their yearly examinations. However, oral cancer had over three times more cases (34,360) diagnosed than cervical cancer last year.3 There are more than 7,550 deaths per year from oral cancer, vs 3,670 for cervical cancer.3 In spite of that, the majority of people do not consider an oral exam necessary to their overall health.
Perhaps one of the reasons that oral cancer is overlooked is that it is one of the most physically disfiguring diseases. This deformity often prevents patients from returning to work; people treated for head or neck cancer have the highest rate of work disability and unemployment. Oral cancer has a devastating affect on a person’s quality of life, affecting their ability to speak, eat, breathe, and socialize. Therefore, their situation—and their disease—is virtually unknown to the public. If their cancer were caught at an earlier stage, the disease could possibly be treated more conservatively, producing fewer complications and less permanent physical and emotional disability.
There is another important fact about oral cancer: the mortality rate has not decreased in the last 50 years. It is the only form of cancer in that position. Dental practitioners need to address this issue, to figure out the means to change this sobering statistic. Decreasing the morbidity rate of oral cancer significantly over the next 10 years is essential.
The role of the dentist in this effort is fundamental: to screen patients, detect problems at a potentially malignant stage, and aggressively manage diagnosis and treatment. This is the ground work of oral healthcare. However, in the past, dentists have been trained to focus on teeth and ignore the mucosa. Studies have shown that dentists miss a majority of oral cancer cases presented to them;4,5 however, this can change as the dental community focuses its resources on oral cancer education.
A standard comprehensive oral exam should include an oral cancer exam. However, screening is not yet routinely performed in many dental practices. Only 14% of US adults over 40 claim to have been screened for oral cancer, and only 7% claim to be screened in the last 12 months.6 There are many reasons that dentists are not using this method to reduce oral cancer rates:
Awareness. Patients are not aware of the disease, and dentists do not want to alarm them unnecessarily by mentioning the word "cancer." However, it is the dentist’s responsibility to explain the process to the patient. The dentist may accurately describe the procedure as a complete oral healthcare examination of teeth, gums, and soft tissues. As a result, the patient may come to think of scheduling a dental examination as they do a yearly physical: primarily for their health and pre-vention of disease, not for a "cleaning." Also, some dentists may not yet be aware themselves of the seriousness and prevalence of oral cancer.
Experience. One method of reducing oral cancer would be to build and maintain the confidence of dentists in their ability to detect this disease at an early stage. In one study, up to 75% of recent graduates from dental school felt that they lacked the ability to recognize malignant and premalignant lesions.7 However, even more alarming was that another study showed the dentists with the highest level of knowledge on risk factors and screening techniques were the recent graduates.8 These studies show that all clinicians need to remain aware of and adopt technological advances in adjunctive screening as they become available.
Once the dentist has detected something that needs further investigation, a number of decisions need to be made and explained. The dentist should be prepared to discuss the need for a biopsy with the patient simply and directly, without causing alarm over something that may be benign.
Often, a less-experienced dentist is unsure how to proceed: how to elevate the appropriate cases as quickly as possible to being looked at by a pathologist, and how to manage the cases that do not need to be elevated. There needs to be documentation of the findings, and communication with an oral surgeon, oral pathologist, or primary physician. The dentist may not be certain how or where to refer the patient for a surgical biopsy, which may be especially complicated if the patient’s insurance requires the patient to get a referral from the primary physician.
When in doubt, refer the patient to someone with more experience. Developing appropriate relationships with specialists and laboratory facilities in advance is extremely beneficial. The oral pathologist is an underused and valuable resource in dentistry today. All dentists should become knowledgeable about the role of and available services of the oral pathology laboratory. A complete list of these laboratories is available on the Web site of the American Academy of Oral Maxillofacial Pathology (www.AAOMP.org).
Commitment. Oral cancer screening is often opportunistic: the patients are there for other purposes. People do not routinely come to dentist for a general oral health examination. Most patients are probably not aware that the dentist is the one most qualified to check for oral cancer; they assume that their primary physician would notice any problems during the throat exam. However, most general physicians receive little training in oral health.
Whatever the original purpose of the patient visit, the dentist should be prepared to use the opportunity, if possible, to provide additional service. This screening process needs to become routine for the dentist, as well as the patient. Extra time may need to be scheduled during regular visits to talk with the patient and perform the exam.
Dentists who are committed to providing this care need to be prepared, and devise a system before they are faced with a patient with oral cancer. Seamless, efficient documentation, communication, and follow-up procedures should be designed and practiced in advance. The necessary information and forms to develop an appropriate system are available online.
Even the fee schedules need to be considered. Many insurance plans are beginning to pay for adjunctive screening as part of a comprehensive oral exam. In the 2007-2008 edition of Current Dental Terminology,9 these codes have been updated:
• D0120 periodic oral evaluation: "includes an oral cancer evaluation and periodontal screening where indicated, and may require interpretation of information acquired through additional diagnostic procedures."
• D0150 comprehensive oral evaluation: "includes an evaluation for oral cancer where indicated, the evaluation and recording of the patient’s dental and medical history and a general health assessment... periodontal conditions (including periodontal screening and/or charting), hard and soft tissue anomalies, etc."
• The D0170 re-evaluation is limited, and may be used for the 2-week follow-up examination: "assessing the status of a previously existing condition" and "soft tissue lesion requiring follow-up evaluation."
SCREENING: THE FIRST STEP
The goal of oral cancer screening is to find disease at the earliest possible stage. The entire oral cavity should be examined visually, tacitly, and with an enhanced visualization modality (such as the VELscope [LED Dental Inc, White Rock, BC, Canada]) to assist in the differentiation between normal healthy tissue, inflammation, and abnormal tissue that may be undergoing atypical cellular changes (Figure 1; Figure 2; Figure 3). Adjunctive screening aids help to locate changes that are not obvious to the human eye. Discovery at an early stage in the disease process will hopefully enable treatments that can be minimally invasive and lead to improved outcomes.
While the screening process and tools for periodontal disease have been widely available to dental practices for decades (and used very successfully), mucosal screening, until recently, has not been as advanced. Screening techniques for oral cancer have only recently begun to improve over the basic gauze, mirror, and human eye. One of the improvements is the more routine use of magnification. It is estimated that 20% of oral hygienists and 80% of clinicians are wearing magnification.
Digital cameras are now available for photographic documentation and follow-up comparison, either at the 2-week period or for a longer time frame. The dentist and oral hygienist also have access to better illumination during the exam. One example is the fiber-optic transilluminator, a good, consistent light source already used in many practices to aid in viewing dental caries. The second illumination option is direct optical fluorescence visualization, a non-invasive technique for assessing the chemical and morphologic composition of tissue. This technique is useful for early-discovery screening and subsequent surveillance and monitoring. It also may be used to guide biopsy/tissue sampling and assist in surgical margin delineation.
The screening method employed should have certain qualities. First, it should enhance the early discovery of abnormal cells. The method should be scientifically proven to be effective, with verifiable claims. It should be safe and non-invasive, and not interfere with any other care or treatment. The method should have FDA clearance for screening and surgical guidance. In addition, it should be easy for the dentist to use—efficient, with minimal steps. It should also be cost-effective over the long term.
Also, the screening method needs to be accepted by the patient. It should have no rinses, chemicals, stains, interactions, aftertaste or discoloration (even temporary) that would cause the patient to be uncomfortable or resistant. It must also be affordable.
SURGICAL BIOPSY: THE STANDARD
It is important to remember that surgical biopsy of intact tissue with a microscopic examination is still the only accepted method of diagnosing cancer. All other modalities are adjunctive procedures to aid in the determination of if and where a surgical biopsy would be appropriate and most beneficial. The role of a surgical biopsy is to confirm or exclude carcinoma, assess the grade of dysplasia, and identify known specific conditions.
A TEAM APPROACH
Preventing and treating oral cancer is a team effort, in which a number of specialists contribute their insights and experience. It begins with the oral hygienist, who does the initial discovery and educates the patient on risk factors. Next is the general practitioner, who focuses on detection and evaluation, and decides on the next step, which may be an enhanced, detailed clinical evaluation that includes an oral surgeon, an oral pathologist, or an ears, nose, and throat specialist. This invaluable group process is the core of the effort to reduce the disabling affects and mortality rate of oral cancer, one patient at a time.
DISCLOSURE
Dr. Benjamin is paid consultant for LED Dental, Inc.
References
1. National Institutes of Health. Fact Sheet: Oral Cancer. Available at: https://www.nih.gov/about/researchresultsforthepublic/OralCancer.pdf. Accessed on December 19, 2007.2. National Institute of Dental and Craniofacial Research. Oral Cancer. Available at: https://www.nidcr.nih.gov/HealthInformation/DiseasesAndConditions/OralCancer/OralCancer.htm. Accessed December 19, 2007.
3. American Cancer Society. Cancer Facts and Figures 2007. Available at: https://www.cancer.org/docroot/STT/content/STT_1x_Cancer_Facts__Figures_2007.asp. Accessed December 19, 2007.
4. Pogrel MA. The dentist and oral cancer in the North East of Scotland. Br Dent J. 1974;137(1): 15-20.
5. Coffin F. Cancer and the dental surgeon. Br. Dent J. 1964;161: 191-202.
6. Horowitz AM, Drury TF, Goodman HS, Yellowitz JA. Oral pharyngeal cancer prevention and early detection. Dentists’ opinions and practices. J Am Dent Assoc. 2000;131(4): 453-462.
7. Burzynski NJ, Rankin KV, Silverman S Jr, Scheetz JP, Jones DL. Graduating dental students’ perceptions of oral cancer education: results of an exit interview of seven dental schools. J Cancer Educ. 2002;17(2):83.
8. Patton LL, Elter JR, Southerland JH, Strauss RP. Knowledge of oral cancer risk factors and diagnostic concepts among North Carolina dentists. Implications for diagnosis and referral. J Am Dent Assoc. 2005;136(5): 602-610.
9. CDT Current Dental Terminology: 2007-2008. Chicago, IL: American Dental Association; 2006.
 | 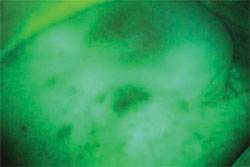 | |
| Figure 1 A suspicious area seen without diagnostic aid. | Figure 2 Visualization is improved with the use of the VELscope. | |
 | ||
| Figure 3 Close up view of the patient examination using the VELscope. | ||
| About the Author | ||
 Scott D. Benjamin, DDS Scott D. Benjamin, DDS Private Practice Sidney, New York | ||



