Evolution of Impression-Free Techniques for Zirconia-Based Restorations
Gregg A. Helvey, DDS; and Keith Miolen
Computer technology has had an enormous impact in dentistry. The word “digital” implies a highly sophisticated technical level, whereas the word “analog” has an old-school connotation. For example, the days of slide film photography have been replaced with digital cameras that reveal data instantly. It would not be the norm today to find rolls of film still being sent off to be developed, just as it would be uncommon to find handwritten journal entries and appointment books still being used instead of computerized front office systems. Digital radiography is also replacing darkrooms and wet processing.
Another area where computer technology is starting to have an impact is the electronic transfer of data to the dental laboratory. Photographic data files containing “before” pictures of patients, including shade selections, can be sent to the laboratory in an instant. Computers are becoming a more common piece of equipment found in the dental laboratory and, along with its other advantages, the increasing use of zirconia has much to do with that.
The Role of Zirconia
Zirconia is increasingly replacing metal for single-tooth copings and fixed partial denture (FPD) frameworks. The literature reports short-term successes with zirconia-based restorations.1-4 In the only 5-year study on the clinical results of zirconia frameworks for posterior FPDs, a 97.8% success rate has been reported.5 Because of its strength and esthetics, and because fewer laboratory hours are required to produce a final restoration when it is used, zirconia is becoming the core substrate of choice.6,7 This can be seen in the rising number of CAD/CAM systems entering the marketplace.8 For clinicians using the CEREC® system (Sirona Dental Systems, Inc, Charlotte, NC), this electronic transfer of data has always been available but, until recently, has not been widely used. Scanned images of prepared individual and multiple single crowns and prepared abutments for FPDs can be sent electronically to a laboratory that has the inLab® system (Sirona Dental Systems, Inc). There are different scenarios where this data transfer can expedite the laboratory phase of indirect restorations.
The following case reports describe the evolution of electronically transferred data and the subsequent impression-free technique, beginning with the fabrication of a single zirconia coping, followed by the fabrication of a 3-unit FPD and an impression-free single crown, and finally the fabrication of an impression-free 4-unit FPD.
Case Report 1
A 63-year-old woman presented with an existing crown on the lower right first bicuspid. She was dissatisfied with the color and appearance of the crown, complaining of the brightness and that metal could be seen at the gingival margin. Examination of the crown revealed an intact, caries-free porcelain ceramo-metal crown that had been placed after endodontic therapy. The shade that had been selected was too bright and less saturated than the adjacent teeth (Figure 1). Options were discussed in terms of material selection for replacing the existing crown. The patient opted for a new ceramic restoration with a zirconia-based substrate.
A chamfer preparation with a beveled margin was revealed after the existing crown was removed. The chamfer portion of the preparation was suitable for fabrication of a zirconia core but the beveled margin was not. The beveled margin creates two problems in the production of a zirconia-based restoration.9 First, the bevel itself is difficult to scan, whether the scanning is done chairside or in thelaboratory on a stone model. Secondly, a beveled margin does not allow room for any porcelain material application without creating an over-contoured emergence profile.
Using an end-cutting diamond bur, the gingival floor was reduced to eliminate the bevel and to create a 90° exit angle (Figure 2 and Figure 3). To check for sufficient occlusal clearance, a 2-mm flexible tab was placed over the preparation with the patient closing into centric occlusion. The tab could be removed without resistance, signifying that a 2-mm reduction was present. Manufacturers of zirconia copings recommend at least 1.5 mm of occlusal reduction. More natural occlusal anatomy can be developed by the laboratory technician with 2 mm of reduction.
The crown margins were isolated with a laser diode. With the CEREC system, a reflective titanium dioxide powder must be applied evenly to the prepared tooth and the adjacent teeth for proper scanning. First, the preparation and the adjacent teeth were scanned. Then the antagonist, which is the occlusal surface of the opposing teeth depicted on the surface of a bite registration, was scanned. Take® 1 Bite™ registration (Kerr Corporation, Orange, CA) was used and then powdered with the titanium dioxide to create a reflective surface.
Once the required images were captured, the CEREC software stitched the images together, producing a virtual model on the monitor. On the virtual model the prepared tooth was trimmed from the adjacent teeth. Next, the ite registration was trimmed so that only the portion over the prepared teeth remained. The margin was marked on the preparation (Figure 4). This step essentially means that the clinician is ditching his or her own dies. Once this step was completed the file was saved.For security reasons the authors do not allow the CEREC computer to go online. Instead, the patient file is downloaded to a flash-drive removable device and then uploaded to a separate computer for the electronic transfer.
Zirconia Coping Fabrication
Once the file was downloaded at the laboratory to the CEREC inLab computer, the fabrication of the zirconia coping was completed. The laboratory opened the file and proceeded to the step where the margin had been indicated with the blue margin line. The antagonist view allowed the technician to adjust for the occlusal clearance and ceramic support. The prescription that accompanied the file had indicated a facial cut-back of 1 mm. Because the laboratory did not have a model in hand, raised dots at the mesial and distal embrasure were placed. After milling, the technician was able to cut back 1 mm from dot to dot. The coping was then sintered. At this point, the coping was returned to the author’s office laboratory for the ceramic application. Upon receiving the coping, it was tried on a working model that had been fabricated from an impression that was taken after the preparation had been scanned by the CEREC acquisition unit (Figure 5).
Ceramic Application
There are two methods of applying the veneering porcelain: layering and hot pressing.10,11 It is necessary that the veneering porcelains have matched coefficients of thermal expansion with the zirconia material. Several manufacturers produce compatible porcelains in both powdered and pressable ingot form. In this case, the author chose to use the pressing method using CZR pressable ingots (Noritake Dental, Aichi, Japan).
The first step in the pressing procedure was to apply two coats of a shade base stain, which increases the bond between the zirconia and the veneering porcelain. The next step was to apply wax to the full contour of the restoration. This can be accomplished using a drop method where wax is applied incrementally to the desired form of the crown. An alternate method of wax application is to use the wax injection method. Using this method, a preoperative impression was taken and poured. A silicone index was constructed over the selected tooth and the adjacent teeth. An injection hole was created in the silicone index over the selected tooth, and a separating medium (mineral oil) was painted on the die and the adjacent teeth of the working model. The zirconia coping was returned to the die and secured in place with a few drops of wax on the facial margin. The silicone index was then placed into position on the working model. Holding the silicone index in place, melted wax was injected through the injection hole. After a brief cooling period, the silicone index was removed. The excess wax was removed and the wax crown with the underlying zirconia coping was removed.
The margins of the crown were verified and smoothed along with the remaining parts of the crown. The finished wax crown was removed from the die and attached to the pressing sprue-former. The crown was invested with a pressing investment (Noritake Dental) and allowed to dry for 18 minutes. At that point the sprue-former base was removed and the invested crown was placed in an oven set at 1,565°C. After 35 minutes of burnout, the invested crown was removed from the oven and a selected pressable ingot was inserted into the pressing channel, followed by the pressing plunger. The entire assembly was thenplaced in the pressing oven.
After ample cooling the crown was divested by means of sandblasting using aluminum oxide at 60 psi. The sandblasting medium was changed to glass beads and the pressure was reduced to 30 psi. Microcrack damage can occur to the zirconia coping at pressures greater than 30 psi, which can subsequently lead to failure.12,13
The crown was removed from the sprue using a diamond wheel. The occlusal surface was cut back to allow for the layering porcelain. The crown was then steam-cleaned. LT Natural enamel was applied and baked at the appropriate temperature. E2 enamel was then applied and baked. Cervical 2 external stain, followed by glaze, was applied for the final bake cycle. The crown was polished using CeramiPro™ Dialite® polishing wheels (Brasseler USA, Savannah, GA) and diamond polishing paste (DiaShine, VHTechnologies LTD, Bellevue, WA).
The restoration was inserted with a luting cement containing phosphate monomer. Reports have shown this type of luting cement to provide a strong and resilient bond (Figure 6).14,15
Case Report 2
A 60-year-old man presented missing the maxillary left first molar and a portion of a ceramic crown on the maxillary left second molar. This tooth had been missing for some time. A previous attempt to place an implant fixture had failed, resulting in extreme bone loss. Different treatment options were presented to restore the area, including bone grafts to build up the defective pontic-receptive site. The patient did not want to engage in any further surgery. During treatment plan discussions it was decided that because the second molar would require a new crown, the restoration would be extended to include the second bicuspid, and a FPD would be placed. Material selection was also discussed with the patient. It was decided to fabricate the FPD using a zirconia framework and a pressable ceramic.
After a study model was made, a replacement tooth was placed in the edentulous area using a light-polymerized resin material (Figure 7). This mock-up model served as the template to fabricate a provisional restoration and to provide the milling laboratory with a correlated image. Using the CEREC chairside scanner, an image of the powdered mock-up model was captured to include the first bicuspid and canine. It was important to include these teeth so that the CEREC software program would be able to correlate or “stitch” the images of the prepared teeth model and the mock-up model together. After the powder was removed, a heated, vacuum-form stent was then fabricated on the model to be used for the provisional restoration.
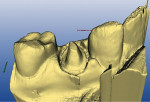
The abutment teeth were prepared and scanned. A bite registration was made using a rigid polyvinyl material that was powdered before scanning. All the information necessary to move forward was present: the prepared teeth, the bite registration, and images of the mock-up model. The program was then advanced to the next step, which displayed a virtual model of the prepared teeth. At times, for a number of different reasons, it is hard for the clinician to see every little detail in the preparation. In this case, the virtual model revealed a ledge that would compromise the fabrication of the restoration (Figure 8). All other areas of the prepared teeth were satisfactory. Therefore, only that portion of the preparation was modified. The abutment teeth were powdered again and rescanned. The program was advanced to the virtual model step, which revealed a more suitable preparation. The file was then saved to a flash-drive removable storage device and electronically transferred to the milling laboratory via e-mail on a different computer.
Zirconia Framework
The milling laboratory downloaded the file onto the CEREC inLab computer and initiated the framework fabrication. The same steps were followed as if the technician had just scanned the working model. The advantage to the electronic transfer is that the technician was able to bypass the time and labor involved in constructing the working model before scanning to proceed with the framework design. Another advantage with this technology is that the clinician has the opportunity to electronically transfer the patient file to the laboratory before the patient is dismissed. The laboratory and the clinician can review the file and make any necessary changes to the preparations that could impede the framework fabrication. This is the first time that such communication is possible without the laboratory technician being physically present at the clinician’s office.
Framework Try-in
Because the porcelain application to the framework was to be completed by the authors, the working model was constructed at the author’s in-house laboratory. The milling laboratory just had to send the framework. The most common scenario is for the clinician to outsource all dental laboratory work. Not all dental laboratories have milling equipment and must outsource zirconia-type frameworks for fabrication. In those cases, the clinician would electronically transfer the preparation file directly to the milling center while sending the impression to their laboratory. This would reduce the turnaround time to complete the restoration. The small laboratory could construct the working model while the milling laboratory was fabricating the framework.
Because of the novelty of this technique, it seemed appropriate to verify the fit of the framework before proceeding to the porcelain lamination phase. The patient returned to the office for the framework try-in (Figure 9 and Figure 10). After the fit was verified, the provisional restoration was replaced and the patient was dismissed.
Porcelain Application and Insertion
The porcelain application followed the same steps as previously described using the wax-injection method. In this situation the silicone index was made from the mock-up model. Once the porcelain was hot-pressed to the framework, the facial and lingual areas were cut back and layered with enamel porcelains. The occlusal surface was stained and glazed.
The intaglio surface of the restoration was cleaned with 50-µm aluminum oxide at 30 psi. The FPD was inserted with PANAVIA F resin cement (Kuraray America, Inc, New York, NY), which has been shown to provide a durable bond to densely sintered zirconia (Figure 11).16
Case Report 3
A 65-year-old patient presented with a defective crown on his upper left first molar. Treatment options were discussed. The impression-free technique was discussed and the patient agreed to participate. Using the CEREC scanner, an oc-clusion picture was captured in the correlation mode. The crown was removed and the tooth was prepared for a porcelain-fused-to-zirconia restoration. The preparation was scanned in the preparation mode and the bite registration was scanned in the antagonist mode. Using the CEREC program, the margin was placed on the prepared tooth and the bite registration was trimmed for the laboratory (Figure 12). The file was saved,transferred to a flash drive, and sent electronically to the milling laboratory.
Laboratory Fabrication
The milling laboratory proceeded to fabricate a zirconia coping. A virtual coping was made in the CEREC inLab program. Subsequently, a full-contoured restoration was designed over the prepared tooth with the coping virtually in place. Once the design process began on the full-contour restoration, the coping informationwas sent to the milling station.
The “die-spacer” parameter in the full-contour mode was increased to allow for two layers of a shade base stain that would be applied to the coping before the porcelain application. The full-contour restoration was milled using a clear, ash-free plastic material. After the coping was milled and sintered, a duplicate die was constructed using a light-polymerized material. The zirconia coping was used to create the margins for the die. Once the duplicate die was finished, the zirconia coping was cut back 360° to allow for a full-porcelain margin. All three parts were then sent back to the author (Figure 13).
Because this impression-free technique was in the developmental stages, the patient agreed to return to the office to verify the fit of the coping with the plastic full-contour portion (Figure 14 and Figure 15). This try-in appointment would not be necessary for future single restorations.
Crown Fabrication
In the author’s laboratory, the zirconia coping was placed on the duplicate die, which was short of the margins because of the cutback. The full-contour restoration was then placed over the coping to verify the fit. The two pieces were then luted together with wax. The plastic crown was attached to the sprue-former and invested. The investment ring was placed in a burnout oven for the appropriate time and then removed. The selected shade ingot (CZR) was placed in the sprue channel followed by the pressing plunger, and the entire assembly was placed in the ceramic pressing furnace.
After completion of the pressing cycle and adequate cooling time, the crown was devested using a sandblasting unit with 50-µm aluminum oxide at 50 psi. To prevent damage to the zirconia coping, the investment was removed from the inner surface of the crown at 30 psi. The crown fit was verified on the duplicate die. A silicone index was made of the occlusal surface. The mesial/distal buccal and lingual cusps were then cut back to allow for the enamel layering porcelains. The cusps were restored back to the original contours using the silicone index as a guide. The occlusal surface was polished and stained. The entire crown was then glazed, finished, and prepared for insertion. The restoration was inserted using PANAVIA F resin cement (Figure 16).
Case Report 4
The most challenging situation would be to fabricate a multi-unit FPD using this impression-free technique. Because of the size of the file and the accuracy of the scanned images, this scenario presented the most testing obstacles. A 50-year-old woman presented with a dislodged 4-unit anterior FPD where two of the abutments had fractured (Figure 17). After discussing the treatment options, it was decided to replace the existing 4-unit porcelain-fused-to-metal FPD with a zirconia-based restoration. The patient understood the novelty of the proposed impression-free technique and agreed to participate.
The present FPD was secured with temporary cement and a study model was taken. After application of a reflective powder, a complete scan of the study model was made. The composite virtual model did not reveal a distinct gingival margin of the pontic area (tooth No. 9) because of the loss of osseous tissue from the previous tooth extraction. Composite material was added to build out the gingival tissue to provide a reflective surface for scanning. The area was powdered and then scanned. This modification provided the necessary reflective information to ascertain a complete image of the study model.
The maxillary right and left lateral incisors had fractured, leaving inadequate tooth length to provide sufficient mechanical retention17,18 Endodontic therapy was completed followed by the placement of a prefabricated post with glass ionomer build-ups.
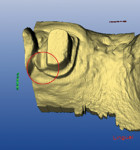
The teeth had been prepared with beveled margins for the previous FPD. As mentioned in the first case report, the beveled margins were converted to butt-joint margins, leaving a 90° exit angle. The preparations were then scanned, and also included the adjacent unprepared teeth. A bite registration was taken, powdered, and then scanned. The scanned images included the preparation, and occlusal and antagonist folders (Figure 18).
The milling laboratory began the same process as previously described in the third case report using the quadrant mode. After the framework was designed, the quadrant mode was selected to fabricate a full-contour version of the FPD. In this mode, the framework becomes part of the “virtual stone model” and the full-contour version is then designed to fit over the framework and teeth. The zirconia framework was milled and then sintered. The full-contour version was milled froman ash-free plastic that was burnable so that the hot ceramic pressing technique could be employed.
The milled plastic version had all of the margins intact of the individual abutments. A duplicate die model was created to preserve the margins. The interproximal areas of the plastic version were then ground out to allow full seating over the zirconia framework. A duplicate die model was made from the preparation side of the bite registration. This model was used to fill in the open area on the tissue side of the pontic with wax (Figure 19). The open areas between the framework and plastic full-contour portion were alsofilled in with wax.
At this point, the restoration can proceed to ceramic pressing or, in other cases, be sent to a clinician who prefers a try-in appointment. If a try-in appointment is favored, then verification of the fit, occlusion, and phonetic testing can be accomplished. The restoration would then be returned to the laboratory for ceramic pressing.
In the laboratory, the entire restoration was attached to the ceramic pressing sprue-former and invested. The ceramic pressing protocol was followed using compatible pressing ingots. After the pressing cycle was complete, the investment was allowed to cool (Figure 20). The restoration was then devested and separated from the sprue base. A silicone index of the entire restoration was fabricated. The incisal portions of the restoration were then cut back to allow for layering of enamel porcelains (Figure 21). Using the original study model, an incisal silicone index was created to verify the length of the teeth (Figure 22).19The final glaze and external stains were then applied. Upon the patient’s return, the FPD was inserted with PANAVIAF resin cement. The final results can be seen in Figure 23 and Figure 24.
Impact of the Impression-free Technique
The four scenarios that have been described share a common denominator: the electronic transfer of data to fabricate indirect restorations. Two cases involved taking impressions that were used for porcelain application while the restoration frameworks were constructed entirely by electronic transmission. In the third case report, the restoration was fabricated entirely from a data file electronically transmitted to the laboratory. In the fourth case report only the bite registration and the preoperative study model (or a model of the provisional restorations) needed to be sent to the laboratory. The advantages of electronic data transfer include shorter turnaround time, the elimination of any impression distortion, instant communication with the dental technician, and the clinician’s ability to designate the restoration margins. Further development of the software will expedite the fabrication process. In the authors’ opinion, this technology opens the door to a new approach in the fabrication of indirect restorations.
Acknowledgment
The authors wish to thank Jonathan Williams at Oral Arts Dental Laboratories, Huntsville, AL, for his contributions.
References
1. Raigrodski AJ, Chiche GJ, Potiket N, et al. The efficacy of posterior three-unit zirconium-oxide-based ceramic fixed partial dental prostheses: A prospective clinical pilot study. J Prosth Dent. 2006;96(4):237-244.
2. Sailer I, Fehér A, Filser F, et al. Prospective clinical study of zirconia posterior fixed partial dentures: 3-year follow-up. Quintessence Int. 2006;37(9):685-693.
3. Sturzenegger B, Fehér A, Lüthy H, et al. Clinical study of zirconium oxide bridges in the posterior segments fabricated with the DCM system [in German]. Schweiz Monatsschr Zahnmed.2000;110(12):131-139.
4. Vult von Steyern P, Carlson P, Nilner K. All-ceramic fixed partial dentures designed according to the Zirkon technique. A 2-year clinical study. J Oral Rehabil.2005;32(3):180-187.
5. Sailer I, Fehér A, Filser F, et al. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont.2007;20(4):383-388.
6. Hauptmann H, Suttor D, Frank H, et al. Material properties of all-ceramic zirconia prosthesis. J Dent Res.2000;79:271.
7. Roundtree P, Nothdurft F, Pospiech P. In-vitro investigations on the fracture strength of all-ceramic bridges of ZrO2- ceramic[abstract]. J Dent Res. 2001(Special Issue);80:57.
8. Forward Trends: CAD/CAM Congress Roundtable. Dental Lab Products. 2007;32(5):20-25.
9. Kurbad A. Clinical aspects of all-ceramic CAD/CAM restorations. Int J Comput Dent. 2002;5(2-3):183-197.
10. Helvey GA. Press-to-zirconia: a case study utilizing cad/cam technology and the wax injection method. Pract Proced Aesthet Dent.2006;18(9):547-553.
11. McLaren EA, Giordano RA. Zirconia-based ceramics: Material properties, esthetic and layering techniques of new veneering porcelain, VM9. Quintessence Dent Technol.2005;28:100.
12. Guazzato M, Quach L, Albakry M, et al. Influence of surface and heat treatments on the flexural strength of Y-TZP dental ceramic. J Dent.2005;33(1):9-18.
13. Curtis AR, Wright AJ, Fleming GJ. The influence of surface modification techniques on the performance of a Y-TZP dental ceramic. J Dent.2006;34(3):195-206.
14. Blatz MB, Sadan A, Martin J, et al. In vitro evaluation of shear bond strengths of resin to densely-sintered high-purity zirconium-oxide ceramic after long-term storage and thermal cycling. J Prosthet Dent. 2004;91:356-362.
15. Wegner SM, Kern M. Long-term resin bond strength to zirconia ceramic. J Adhes Dent. 2000;2(2):139-147.
16. Wolfart M, Lehmann F, Wolfart S, et al. Durability of the resin bond strength to zirconia ceramic after using different surface conditioning methods. Dent Mater. 2007;23(1):45-50.
17. Blatz MB. Comprehensive treatment of traumatic fracture and luxation injuries in the anterior permanent dentition. Pract Proced Aesth Dent.2001;13(4):273-280.
18. Dietschi D, Jacoby T, Dietschi JM, et al. Treatment of traumatic injuries in the front teeth: restorative aspects in crown fractures. Pract Proced Aesthet Dent. 2000;12(8):751-760.
19. Romeo G. Aesthetic stratification of metal-ceramic crown restorations for natural manipulation of light. Pract Proced Aesthet Dent. 2001;13(5):411-415.
About the Author
Gregg A. Helvey, DDS
Adjunct Associate Professor
Virginia Commonwealth University
Richmond, Virginia
Private Practice
Middleburg, Virginia
Keith Miolen
CAD/CAM Projects Manager
Oral Arts Dental Laboratory
Huntsville, Alabama