Integrating Laser Technology Into a General Dental Practice
Martin Jablow
Martin Jablow, DMD
It has been almost 20 years since the first dental laser became available to treat oral soft tissue, and 10 years since dentists began treating tooth and bone with a laser. Once, lasers were considered complex technology with limited use in dentistry, and while there is still an ongoing debate about the benefits of dental laser therapies over conventional treatments, dentists are now aware of the many clinical applications for various dental lasers in the modern dental practice. This article will explore integrating a dental laser into a general dental practice.
LASERS IN DENTISTRY
Laser stands for "light amplification by stimulated emission of radiation." A laser must be evaluated by what effect occurs when the laser energy strikes the tooth. The light can be absorbed, reflected, scattered within the tissue, or transmitted. Light energy that is scattered or transmitted may cause damage to adjacent tissues. Reflected laser light usually dissipates quickly so it does no damage. In dentistry, the most common lasers are named after the component or crystal used in the laser’s optical cavity. A diode laser uses semi-conductors; the other lasers use crystals and are named after the chemical composition of the crystals. These lasers go by initials such as Nd:YAG, Er,Cr:YSGG, or Er:YAG. Manufacturers give trade names to their lasers so the same laser wavelength may be associated with multiple laser companies. Small differences in wavelengths between similar lasers are used by the companies to try to distinguish their products and market their lasers (Figure 1).
Nd:YAG and diode lasers are primarily used on soft tissue because at these wavelengths the targeted tissue is pigmented, allowing for absorption (Figure 2). These lasers provide good coagulation. They can penetrate a few millimeters into the tissue. Erbium-wavelength lasers can cut tooth, bone, and soft tissue. They have an affinity to water. They are not as good at providing hemostasis but only penetrate into tissue in microns. There are even low-power diagnostic lasers.
In most cases, laser energy is directed to the targeted tissue by a thin, flexible glass fiber. With Nd: YAG and diode lasers, the fiber is usually used by contacting the tissue directly. Erbium lasers can use glass fibers or hollow wave-guides (mirrors) to direct the laser energy at the tissue. The erbium laser handpiece has a sapphire or glass tip that is normally used in a non-contact mode while cutting.
When incorporating a dental laser into the office, there are several factors to consider. A clinician’s choice of laser and wavelengths will be dictated by the procedures that he or she intends to perform. Think of a laser as another tool in the tool box. Just as one would have both nails and screws to do similar but different jobs, a clinician may also have lasers of various wavelengths.
First, look at the laser’s footprint. Erbium lasers are on casters and the boxes are mobile, but most dentists do not drag them between operatories. Erbium lasers require a connection to compressed air and have bottles for distilled water to aid in cooling when cutting hard tissue. Nd:YAG lasers can be on casters and tabletop models do exist. So Nd:YAG lasers can be transported but, again, in most cases they are assigned to one treatment room. Diagnostic and diode lasers are getting small enough to be considered transportable. Some are just larger then an iPod (Apple, Inc, Cupertino, CA), so it is quite simple to move them between operatories to wherever they are needed.
THE RIGHT LASER FOR YOUR PRACTICE
How do clinicians choose the best dental laser for their practice? They need to know what they want to accomplish. Soft tissue laser procedures include periodontal treatments, destruction of aphthous ulcers, frenectomies, and biopsies. All lasers are not the best for each of these procedures. For those looking to incorporate lasers, the Nd:YAG would be the better choice for periodontal surgeries as there is significant literature on the use of this laser.1-5 Biopsies and frenectomies can easily be accomplished with Nd: YAG or diode lasers because of the ability to better visualize the surgical field because of the laser’s ability to coagulate and seal vessels (Figure 3 and Figure 4).
Periodontal procedures such as the laser-assisted new-attachment procedure allow for minimally invasive surgery as an alternative to conventional flap surgery.1 The laser is placed into the sulcus and removes the diseased epithelium. Scaling is performed to remove calcified plaque and calculus from the root surfaces. The Nd:YAG produces a bactericidal effect in the pocket. This results in pocket reductions of up to 3.4 mm, depending on initial pocket depth.1 There is currently much debate as to the effectiveness of laser periodontal surgery. In some individuals there is a regeneration of cementum, bone, and periodontal ligament.2 The American Academy of Periodontology conducted a review of literature for lasers in periodontics and concluded that some wavelengths of lasers used for treating chronic periodontitis may be equivalent to scaling and root planing with respect to reduction in pocket depth.3
Er:YAG, Nd:YAG, or diode lasers can be used for the destruction of aphthous ulcers and other lesions.4 A simple 30-second passing of laser energy can transform a sore that hurts into a sore that does not hurt with uneventful healing. The advantages of laser therapy for biopsies and other oral surgery include minimal postoperative pain, conservative site-specific minimally invasive surgeries, and, in many cases, the elimination of the need for sutures.5 Even a denture sore or a lacerated tongue from a broken cusp can be made painless after adjusting the prosthesis or tooth and by using the laser in a manner comparable to treating an aphthous ulcer.
Diagnostic lasers emit a visible red light from a diode laser and are combined with a detection system. These lasers are used to detect smooth surface and pit-and-fissure caries. These lasers operate at a wavelength of 655 nm. At this wavelength, healthy tooth structure has a "known" fluorescence, and the emission spectral shift in fluorescence determines the probability of decay. The laser light causes the carious area to fluoresce, and the fluorescence is then quantitatively measured to determine the quantity of decay (Figure 5). Laser caries detection offers greater sensitivity than conventional visual and tactile methods.6 If a problem cannot be properly diagnosed, there is no way to offer the correct treatment. Early diagnosis of carious lesions makes the treatment for both the patient and the dentist easier while conserving tooth structure.
Currently the most marketed lasers are the erbium-based lasers (Er,Cr:YSGG and Er:YAG). These lasers can handle both hard and soft tissue procedures. The hard tissue procedures most general dentists are looking for are cavity preparations. All cavity preparation types are amenable to laser treatment. Conventional GV Black preparations do not need to be followed when using a laser. Erbium lasers are effective in caries removal and cavity preparation while minimizing thermal and collateral damage and also keeping patients very comfortable.7-10 The use of erbium lasers allows many dental restorative procedures to be accomplished without anesthesia.11 The ability to move between quadrants without anesthesia improves the efficiency of many operative dentistry procedures. This makes the erbium laser an excellent choice for treating children.12 Erbium lasers are kinder to teeth than the high-speed handpiece because there is no microfracturing and no smear layer resulting in open dentinal tubules, thus enhancing bonding.13 The downside is that the erbium lasers do not cut as fast as high-speed handpieces, though they are much more conservative to tooth structure. Rotary handpieces cut in millimeters whereas erbium lasers cut in microns (Figure 6). Unfortunately, erbium lasers have little interaction with amalgam and no interaction with metal and porcelain. They cannot be used to remove amalgam restorations but can be used to very selectively remove recurrent decay around existing crowns or veneers. Erbium lasers are effective in removing composite restorations.
Erbium lasers are good for soft tissue surgery but do not provide the same coagulation effects as Nd:YAG or diode lasers (Figure 7 and Figure 8). Second-stage implant surgery with an erbium laser allows implants to be uncovered with either a reduced or no need for anesthesia, absence of postoperative pain, no damage to the implant, and improved tissue healing. This rapid healing allows for faster prosthetic fabrication.14 Other soft tissue surgery, such as the destruction of lesions, frenectomies, and biopsies, can be accomplished with limited need for anesthesia. Apical surgery performed with an erbium laser shows lower microleakage and, thus, may lead to better outcomes then a conventional apicoectomy performed with an ultrasonic or conventional handpiece.15
Lasers are also finding a place in endodontic therapy. The access and instrumentation of the root canal system has been ac-complished with lasers. For now, most laser use in endodontics involves disinfecting the canal. Irrigants such as sodium hypochlorite and ethylenediamine tetraacetic acid have been widely used to disinfect and remove the smear layer created by hand and rotary instrumentation. Er: YAG lasers have been shown to be more effective in disinfecting the canals than the commonly used liquid irrigants.16 Er:YAG, Nd:YAG, and diode lasers have all been shown to provide disinfection of the root canal system. Erbium lasers also open the dental tubules.17 Lasers are proving to be a valuable adjunct in endodontic therapy.
CONCLUSION
One objection that some dentists have to lasers is that they can only perform a limited number of procedures. Lasers lend themselves to minimally invasive dentistry. Laser dentistry is different from but also complementary to traditional dentistry. An example is being able to perform soft and hard tissue treatment in multiple quadrants at the same appointment. Consider doing interproximal tunnel preparations instead of a conventional Class II restorative preparation. The less healthy tooth structure removed during a restorative procedure, the better for the long-term health of the tooth. Destroying an apthous ulcer before starting patient treatment allows the patient to be more comfortable during the procedure. There are many ways that lasers change the way a dentist will look at the solution to the patient’s dental problems. The limits to the solutions are based on the dentist’s clinical experience and the laser wavelengths available.
More dentists are incorporating lasers into their practice of dentistry. Practitioners must become knowledgeable and proficient in the use of lasers. Deciding which laser to purchase should be based on the clinical needs of the practice. Learn as much as possible about lasers and how they can enhance the practice of dentistry by attending lectures, asking other dentists about how they use lasers, and checking the laser dentistry forum online at www.laserdentistryforum.com.
The biggest objection for most dentists is justifying the cost of a dental laser. The usual argument is that lasers are no better than rotary handpieces or a scalpel so why spend the money? What is being missed is the patient aspect of the equation. Many studies show that the patients are more comfortable when lasers are used for treatment.18 So it is really an economic decision by the dentist whether he or she will offer patients the latest treatment modality or not—just ask any child or many adults if they prefer to get a "shot" or not.
REFERENCES
1. Harris DM, Gregg RH, McCarthy DK, et al. Laser-assisted new attachment procedure in private practice. Gen Dent. 2004;52(5):396-403.
2. Yukna RA, Evans GH, Vastardis S, et al. Laser-assisted Periodontal Regeneration in Humans. Paper presented at: 81st General Session of the International Association for Dental Research; June 27, 2003; Louisiana State University, New Orleans, LA.
3. Cobb CM. Lasers in periodontics: a review of the literature. J Periodontal. 2006;77(4):545-564.
4. Asgari A, Jacobson BL, Mehta M. Aphthous ulcers: treatment and case report. Dent Today. 2006;25(9):128-129.
5. White JM, Chaudhry SI, Kudler JJ, et al. Nd:YAG and CO2 laser therapy of oral mucosal lesions.J Clin Laser Med Surg. 1998;16(6):299-304.
6. Lussi A, Megert B, Longbottom C, et al. Clinical performance of a laser fluorescence device for detection of occlusal caries lesions. Eur J Oral Sci. 2001;109(1):14-19.
7. Hibst R, Keller U. Experimental studies of the application of the Er:YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg Med. 1989;9(4):338-344.
8. Keller U, Hibst R. Experimental studies of the application of the Er:YAG laser on dental hard substances: II. Light microscopic and SEM investigations. Lasers Surg Med. 1989;9(4):345-351.
9. Walsh JT, Flotte TJ, Deutsch TF. Er:YAG laser ablation of tissue: effect of pulse duration and tissue type on thermal damage. Lasers Surg Med. 1989;9(4):314-326.
10. Walsh JT, Deutsch TF. Er:YAG laser ablation of tissue: measurement of ablation rates. Lasers Surg Med. 1989;9(4):327-337.
11. Matsumoto K, Wang X, Zhang C, et al. Effect of a novel Er:YAG laser in caries removal and cavity preparation: a clinical observation. Photomed Laser Surg. 2007;25(1): 8-13.
12. Liu JF, Lai YL, Shu WY, et al. Acceptance and efficiency of Er:YAG laser for cavity preparation in children. Photomed Laser Surg. 2006;24(4):489-493.
13. Pelagalli J, Gimbel CB, Hansen RT, et al. Investigational study of the use of Er:YAG laser versus dental drill for caries removal and cavity preparation—phase I. J Clin Laser Med Surg. 1997;15(3): 109-115.
14. Arnabat-Domínguez J, España-Tost AJ, Berini-Aytés L, et al. Erbium:YAG laser application in the second phase of implant surgery: a pilot study in 20 patients. Int J Oral Maxillofac Implants. 2003;18(1):104-112.
15. Karlovic Z, Pezelj-Ribaric S, Miletic I. Erbium:YAG laser versus ultrasonic in preparation of root-end cavities. J Endod. 2005;31(11): 821-823.
16. Takeda FH, Harashima T, Kimura Y, et al. A comparative study of the removal of smear layer by three endodontic irrigants and two types of laser. Int Endod J. 1999;32(1): 32-39.
17. Schoop U, Kluger W, Dervisbegovic S. Innovative wavelengths in endodontic treatment. Lasers Surg Med. 2006;38(6):624-630.
18. Jacboson B, Berger J, Kravitz R, et al. Laser pediatric crowns performed without anesthesia: a contemporary technique. J Clin Pediatr Dent. 2003;28(1):11-12.
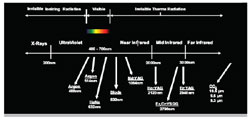 | 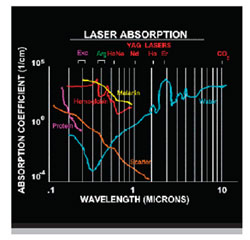 |
| Figure 1 Dental laser wavelengths on the electromagnetic spectrum. | Figure 2 Dental laser wavelengths and their absorption spectrum. |
 |  |
| Figure 3 Preoperative image of a lower lip fibroma. | |
 | |
| Figure 4 Immediate postoperative image of the fibroma excisional biopsy made with an Nd:YAG laser. Note the lack of bleeding. | Figure 5 Diagram of the DIAGNOdent® (KaVo Dental Corp, Lake Zurich, IL) examining for caries fluorescence. |
 |  |
| Figure 6 Er:YAG laser restoration preparation. | Figure 7 Preoperative view of a maxillary canine exposure. |
 | |
| Figure 8 Exposure of a maxillary canine with only topical anesthesia using an Er:YAG laser. Notice the slight bleeding, as Er:YAG lasers are not as good as Nd:YAG or diode lasers at coagulating. | |
 | Martin Jablow, DMD Private Practice Woodbridge, New Jersey |



