Using the STA™ System to Produce Profound Anesthesia in a Variety of Routine Clinical Situations
Marty Jablow, DMD
With the vast array of digital or computer-controlled equipment in the dental office today, it is hard to believe there is one fundamental piece of equipment dentists use for virtually every type of procedure that has remained practically unchanged for over 150 years: the dental syringe.
Before its routine use in dentistry, the syringe had been used primarily by the medical profession during surgical procedures for local anesthesia, and also for the administration of drugs into the body. It was not until the late 1800s that Dr. William Halstead introduced the first pain-management techniques to dentistry.1,2 Using a slightly modified medical syringe, he demonstrated that an interstitial injection of aqueous cocaine into the trunk of a nerve resulted in the numbing of pain in all of the nerve’s branches (similar to a modern-day mandibular block).2 Many important developments have occurred in local dental anesthesia since then, particularly in the formulation and pharmacokinetics of dental anesthetics, but very few meaningful improvements have been made to the overall design and mechanics of the dental syringe itself.
That changed in 1997 with the introduction of a new computer-controlled local anesthetic delivery system (CCLAD) pioneered by Milestone Scientific (Livingston, NJ). The original product consisted of a computer-controlled drive unit and a separate, single-use, disposable handpiece/needle assembly. Ten years later, Milestone Scientific brought to market yet another advancement in CCLAD technology with the introduction of the STA™ Single Tooth Anesthesia System (Figure 1).3,4
THE DENTAL SYRINGE GOES DIGITAL
The dental syringe has been updated and substantially improved for the digital era. The injection procedures described herein were all performed using the STA System to produce profound anesthesia in a variety of routine cases and indications. The name of the device is a misnomer, as the system is capable of performing all of the injections that can be done with a conventional syringe, including the palatal anterior superior alveolar (P-ASA), anterior middle superior alveolar (AMSA), inferior alveolar nerve block (IANB), and a modified periodontal ligament (PDL) known as the STA-intraligamentary injection. In the author’s clinical experience, the STA System achieves all of these injections predictably and reliably with almost immediate onset of profound anesthesia.
Another difference between the STA System and a conventional syringe is in the design of the handpiece itself (Figure 2 and Figure 3). The STA handpiece is thin and flexible, allowing excellent needle visibility. Shaped like a pen, it is held between the thumb and forefinger, which allows precise control during all phases of injection. Additionally, the handpiece is easily rotated to help avoid needle deflection, and can be held close to the top of the syringe for even greater tactile response.
The STA System is a second-generation CCLAD device. The core technology behind the success of the system is a technology called DPS™, or Dynamic Pressure Sensing Technology (Milestone Scientific).5 This proprietary technology allows the dentist to easily and accurately identify specific tissue types at the needle position (needle tip), based on tissue compliance. During an injection, the system continuously monitors the exit pressure of the anesthetic liquid during all phases of drug administration.6-8 The measured pressure data becomes a feedback signal, which is then converted into an audible sound, as well as a visual display, so that the dentist is continuously aware of the tissue density encountered.
For example, during an STA-intraligamentary injection, the injection requires the needle tip to be physically guided to the appropriate tissue target: the PDL. The PDL possesses an interstitial pressure range that is unique to the surrounding tissues, such as bone and attached and unattached gingival tissues. Once the needle tip is located in the proper space, the STA System provides real-time confirmation that the needle tip has reached its target successfully. This feedback is user-selectable and can be in the form of audible tones, a visual light display located on the drive unit, and/or computer-generated voice alerts.
The STA unit is small and compact (about the size of a cable modem), and the author has it on a bracket table attached to the dental light pole. This makes the unit easy to reach and gives easy access to the visual indicators through the author’s peripheral vision.
CASE 1
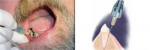
A 58-year-old man presented with the need for restoration on the mandi-bular right first molar and extraction of both abutments of a 3-unit bridge on the mandibular left. Using the STA System, a conventional IANB and long buccal infiltration were administered (1.8 ml 3% mepivacaine) on the left side using a 27-gauge long needle. This was done for procedural anesthesia along with postoperative pain control. An STA-intraligamentary injection was administered on the mandibular right first molar (0.9 ml 3% mepivacaine) using a 30-gauge extra-short needle (Figure 4 and Figure 5). This was done to allow bilateral treatment and reduce the concern for posttreatment trauma to the lip or tongue. The areas to be injected were dried with gauze and topical anesthetic was placed for 2 minutes. The IANB and long buccal infiltration were administered in a conventional manner with the STA System. The STA-intraligamentary injection was administered on both the distal and mesial of the molar. Anesthesia was achieved instantly. Treatment on the molar was started immediately and the restoration was completed. By the time the restoration was completed, the left side had achieved profound anesthesia and the author was able to proceed with the extractions. The use of the STA System allowed for a more efficient use of time, as it was not necessary to wait for bilateral anesthesia to take effect. The patient was more comfortable and did not have the increased risk of anesthesia-associated trauma. In many cases, dentists would have scheduled the restorative treatment at another appointment.
CASE 2
A 68-year-old man required scaling and root planing of the maxillary arch. The patient was missing all his maxillary molars. The areas to be injected were dried with gauze and topical anesthetic was placed for 2 minutes. Bilateral AMSA injections (0.9 ml 3% mepivacaine) were given with the STA System using a 30-gauge short needle (Figure 6). Using a conventional syringe for the buccal and palatal infiltration technique, up to eight injections may have been necessary. Anesthesia of both buccal and palatal soft tissue was achieved and the periodontal procedure completed. The patient received fewer injections and probably less local anesthesia compared to conventional infiltrations; plus, the patient did not have to suffer from altered orofacial sensations.
CASE 3
A 27-year-old woman presented with pain associated with the mandibular left second premolar. A diagnosis of irreversible pulpitis was made. After discussing treatment options with the patient, a decision to initiate endodontic therapy was made. Using the STA System, a conventional IANB was administered (1.8 ml 3% mepivacaine) on the left side using a 27-gauge long needle (Figure 7). This was done for procedural anesthesia along with postoperative pain control. The patient indicated she had achieved profound anesthesia, which was corroborated by clinical observations. A rubber dam was placed and treatment initiated. The patient was complaining of pain during the attempt to access the pulp ("hot tooth"). The rubber dam was removed and a decision was made to use the STA- intraligamentary injection. The technique was the same as in the first case. The rubber dam was replaced and the pulpectomy procedure was completed without any further discomfort for the patient.
DISCUSSION/CONCLUSION
While any of these injections could have been performed with a conventional syringe, the STA System provides many benefits to both doctor and patient. Employing the STA-intraligamentary injection results in profound anesthesia of a single tooth with just two injections, typically performed as one injection on the distal side of the tooth and one on the mesial side. Collateral numbness of the lips and face is avoided, and onset of anesthesia is immediate, allowing the tooth restoration procedure to begin at once, without the typical 5- to 10-minute waiting period associated with a conventional injection. Hot teeth can be treated with greater patient comfort with a predictable way to supplement other anesthesia techniques. Multiple-quadrant dental treatment is easily facilitated with the STA-intraligamentary injection, especially in comparison to traditional injection techniques that typically require anesthetizing an entire mandibular quadrant, and patients have been enthusiastic about not going home with that numb-lip feeling.
References
1. Jacek B. Man behind the instrument(2): Halstead, William Stewart (1852-1922). Br J Theatre Nurs. 1994;4(2):25.
2. Ingle JI. William Halstead, surgeon, pioneer in oral nerve block injection, and victim of drug experimentation. J Am Dent Assoc. 1971;82(1):46-47.
3. Hochman M, Chiarello D, Hochman CD, et al. Computerized local anesthesia delivery vs. traditional syringe technique. Subjective Pain Response. NY State Dent J. 1997;63(7):24-29.
4. Friedman MJ, Hochman MN. A 21st century computerized injection for local pain control. Compend Contin Educ Dent. 1997;18(10):995-1003.
5. Hochman M. [inventor] Pressure/Force computer controlled drug delivery system and the like. United States Patent Office 2001; US Patent #6,200,289. www.freepatentsonline.com/6200289.html. Accessed June 11, 2007.
6. Pashley EL, Nelson R, Pashley DH. Pressures created by dental injections. J Dent Res. 1981;60(10):1742-1748.
7. Pertot WJ, Dejou J. Bone and root resorption: Effects of the force developed during periodontal ligament injections in dogs. Oral Surg Oral Med Oral Path. 1992;74(3): 357-365.
8. Ghelber O, Gebhard R, Adebayo G, et al. Utilization of the CompuFlo™ in determining the pressure of the epidural space: A pilot study. Anesth Analg. 2005;100: S-189.
About the Author
Marty Jablow, DMD
Green Street Dental Group
Woodbridge, New Jersey