Optimizing Anterior Esthetics with Immediate Implant Placement and a Fixed Provisional Restoration: A Patient Presentation
George Priest, DMD
Implant placement immediately after tooth extraction, followed by an immediate provisional restoration of a single dental implant, provides significant benefits compared with traditional delayed protocols. Patients are not burdened with cumbersome removable interim prostheses,1 osseous anatomy may be preserved,2 sulcular form is optimized before definitive restoration,3 soft tissue has matured before implant integration,4,5 fewer surgical interventions are required,6 and treatment time is accelerated.7-9 A few authors noted a diminished implant success rate for immediately restored single implants with provisional crowns compared with delayed restoration.10,11 However, many researchers reported short-term success rates between 96% and 100%.12-18 Factors critical to success of immediate restoration include initial implant stability in good quality bone and patient compliance with instructions to avoid the provisional restoration during mastication.19-21
Immediate implant placement and restoration of single implants may demonstrate a positive effect on peri-implant soft tissue.22,23 Contours of the implant abutment and restoration dramatically affect sulcular form.24,25 The provisional crown can be used to prosthetically sculpt the tissue after implant surgery.26 It aids in developing the gingival tissue from a narrow cylindrical implant to the three-dimensional gingival form of a tooth as the implant emerges from the sulcus.27,28 The provisional restoration may control displacement of the available soft tissue around a single implant to create the desired soft tissue contour.29,30 Accomplishing optimal sulcular form with a metal alloy temporary cylinder may be technically challenging and time-consuming.
The author has observed that metal temporary cylinders have several limitations. They are not easily prepared, they are difficult to mask behind translucent temporary acrylic resins, and they can cast a gray hue through the peri-implant gingiva. Several manufacturers have recently introduced resin and polymer temporary cylinders to overcome these obstacles. Some of these cylinders include a plastic abutment connection (ie, Temporary Abutment; Nobel Biocare™ Yorba Linda, CA; Hex-Lock® Plastic Temporary Abutment; Zimmer Dental, Carlsbad, CA; and ProTect Abutment; Friadent/Xive®, DENTSPLY Friadent Ceramed, Lakewood, CO). PreFormance™ Provisional Components (3i, Implant Innovations, Inc, Palm Beach Gardens, FL), include a titanium insert for strength and precision fit (Figure 1). The Temporary Meso Abutment (Straumann®, Andover, MA) is another polymer temporary cylinder with a titanium insert.
The PreFormance Post for cement-retained provisional restorations and PreFormance Temporary Cylinder for screw-retained provisional restorations are made of a biocompatible, tooth-colored polymer called PEEK (polyetheretherketone). PreFormance Provisional Components are easily customized to a patient’s tissue contours and anatomic profile. Intraoral preparation is completed more quickly than with metal alloy temporary cylinders because polymer components are easily prepared with high-speed burs. Because of the elimination of gray-colored metallic components, the white hue of the PreFormance Post imparts both a natural color to the provisional restoration and warm tones through the translucent gingival tissues. The following patient example illustrates the use of the PreFormance Provisional Post for immediate restoration of a single implant in the esthetic zone.
Patient Presentation
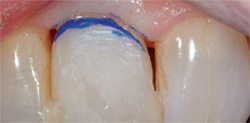
A 50-year-old woman presented with a failing maxillary right central incisor (Figure 2). Radiographic examination revealed root resorption of the endodontically treated tooth (Figure 3). Several metal-ceramic crowns had been placed over the previous 10 years. The patient was also unhappy with the esthetics of her smile, and did not want to have a removable provisional restoration during treatment. The recommended treatment plan accepted by the patient included immediate implant placement and an immediate implant-supported, fixed provisional restoration.
The failing tooth was atraumatically extracted using periotomes to maintain the cortical and interseptal bone. Instead of conventional implant placement involving a soft-tissue flap, the treating periodontist performed flapless surgery and used an osteotome technique to preserve the hard and soft tissues (Figure 4). An internally interfaced OSSEOTITE® Certain® 4 mm x 13 mm implant (3i Implant Innovations, Inc) was placed into the prepared site (Figure 5).
Immediately after implant placement, the restorative dentist seated a PreFormance™ Post into the internal interface of the implant for fabrication of a cement-retained provisional crown. The Certain® QuickSeat® Connection provided an audible and tactile click to verify complete seating of the post, which was verified radiographically. The post was marked intraorally, removed, placed onto a laboratory holder and modified using a coarse high-speed diamond bur (Figure 6).
The post was reseated intraorally. A vacuum-formed matrix was filled with bis-acryl resin, seated over the post, and removed before final setting of the resin. The provisional restoration was trimmed and reseated intraorally, and flowable composite resin was then used to fill in the deficient contours (Figure 7). The post and provisional crown were removed and the contours were refined and polished on a laboratory holder (Figure 8). The restorative dentist developed subgingival contours to optimize soft-tissue support. A Titanium Hexed Retaining Screw (3i, Implant Innovations, Inc) tightened to 20 Ncm with a Restorative Torque Indicator (3i, Implant Innovations, Inc) secured the PreFormance Post to the implant. Following the protocol for immediate nonocclusal loading, the absence of occlusal contacts in centric and eccentric positions were verified. The provisional crown was then cemented with temporary cement (Figure 9).
The patient initially requested a diastema between the central incisors to match her original natural dentition; however, after wearing the provisional crown for 3 months, she preferred to have the diastema closed for the definitive restoration. Four months after implant placement and immediate provisionalization, the restorative dentist placed an Encode® Patient Specific Final Abutment (3i, Implant Innovations, Inc) and a ceramic crown (Figure 10 and Figure 11). Optimal occlusion was developed with centric contacts and protrusive disclusion with the contralateral maxillary central incisor.
Discussion
Today the demand for optimal esthetics is coupled with the desire for faster, easier techniques that minimize chairtime. Seating a provisional restoration at the time of surgical implant placement benefits both the clinician and the patient by eliminating a second surgical procedure and immediately providing a secure and esthetic restoration.
PreFormance Provisional Components provide an easy and efficient way to fabricate cement- or screw-retained provisional restorations on the same day as implant placement. These components can be easily customized for optimal sulcular form and anatomic profiles. In the clinical example presented, an immediate provisional restoration allowed the patient to assess her smile and clarify her expectations for the design of the definitive restoration. Technological advancements such as PreFormance Provisional Components provide clinicians with the ability to offer patients esthetically pleasing, immediate fixed restorations supported by dental implants. Intraoral preparation is faster and easier than with titanium components. The Emergence Profile (EP®, 3i, Implant Innovations, Inc) contours of the posts provide for soft-tissue support and more natural toothlike contours, which improve treatment outcomes. PreFormance Provisional Components offer dentists an additional tool to enhance implant results and meet the esthetic demands of their patients.
DISCLOSURE
George Priest, DMD, is a consultant and mentor for 3i, Implant Innovations, Inc, Palm Beach Gardens, Florida.
References
1. Castellon P, Casadaban M, Block MS. Techniques to facilitate provisionalization of implant restorations. J Oral Maxillofac Surg. 2005;63(9 Suppl 2):72-79.2. Jivraj S, Reshad M, Chee WWL. Immediate loading of implants in the esthetic zone. J Esthet Dent. 2005;17(5):320-325.
3. De Kok IJ, Chang SS, Moriarty JD, Cooper LF. A retrospective analysis of peri-implant tissue responses at immediate load/provisionalized microthreaded implants. Int J Oral Maxillofac Implants. 2006;21(3): 405-412.
4. Jemt T. Restoring the gingival contour by means of provisional resin crowns after single-implant treatment. Int J Periodont Restorative Dent. 1999;19(1): 21-29.
5. Schropp L, Isidor F, Kostopoulos L, Wenzel A. Interproximal papilla levels following early versus delayed placement of single-tooth implants: A controlled clinical trial. Int J Oral Maxillofac Implants. 2005;20(5): 753-761.
6. Moy PK, Parainter PE. Chairside preparation of provisional restorations. J Oral Maxillofac Surg. 2005;63(9 Suppl 2):80-88.
7. Saadoun AP, Sebbag P. Immediate implant placement and temporization: Literature review and case studies. Compend Cont Educ Dent. 2004;25(4): 277-298.
8. Covani U, Bortolaia C, Barone A, Sbordone L. Bucco-lingual crestal bone changes after immediate and delayed implant placement. J Periodontol. 2005;75(12):1605-1612.
9. Rosenquist B, Grenthe B. Immediate placement of implants into extraction sockets: Implant survival. Int J Oral Maxillofac Implants. 1996;11(2):205-209.
10. Chaushu G, Chaushu S, Tzohar A, Dayan D. Immediate loading of single-tooth implants: Immediate versus non-immediate implantation. A clinical report. Int J Oral Maxillofac Implants. 2001;16(2):267-272.
11. Ericsson I, Nilson H, Lindh T, et al. Immediate functional loading of Brånemark single tooth implants. An 18 month clinical pilot follow-up study. Clin Oral Impl Res. 2000;11(1): 26-33.
12. Cornelini R, Cangini F, Covani U, Wilson TG Jr. Immediate restoration of implants placed into fresh extraction sockets for single-tooth replacement: A prospective clinical study. Int J Periodontics Restorative Dent. 2005;25(5): 439-447.
13. Proussaefs P, Kan J, Lozada J, et al. Effects of immediate loading with threaded hydroxyapatite-coated root-form implants on single premolar replacements: A preliminary report. Int J Oral Maxillofac Implants. 2002;17(4): 567-572.
14. Lorenzoni M, Pertl C, Zhang K, et al. Immediate loading of single-tooth implants in the anterior maxilla. Preliminary results after one year. Clin Oral Impl Res. 2003;14(2):180-187.
15. Norton MR. A short-term clinical evaluation of immediately restored maxillary TIOblast single-tooth implants. Int J Oral Maxillofac Implants. 2004;19(2):274-281.
16. Kan JYK, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003;18(1):31-39.
17. Covani U, Crespi R, Cornelini R, Barone A. Immediate implants supporting single crown restorations: A 4-year prospective study. J Periodontol. 2004;75(7):982-988.
18. Wohrle PS. Single-tooth replacement in the aesthetic zone with immediate provisionalization: Fourteen consecutive case reports. Pract Periodont Aesthet Dent. 1998;10(9):1107-1114.
19. Del Fabbro M, Testori T, Francetti L, et al. Systematic review of survival rates for immediately loaded dental implants. Int J Periodontics Restorative Dent. 2006;26(3):249-263.
20. Gapski R, Wang H-L, Mascarenhas P, Lang NP. Critical review of immediate implant loading. Clin Oral Impl Res. 2003;14(5):515-527.
21. Otonni JMP, Oliveira ZFL, Mansini R, Cabral AM. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants. 2005;20(5):769-776.
22. Andersen E, Haanæs HR, Knutsen BM. Immediate loading of single-tooth ITI implants in the anterior maxilla: a prospective 5-year pilot study. Clin Oral Impl Res. 2002;13(3):281-287.
23. Kan JYK, Rungcharassaeng K. Site development for anterior single implant esthetics: The dentulous site. Compend Contin Educ Dent. 2001;22(3): 221-231.
24. Jemt T, Lekholm U. Measurements of buccal tissue volumes at single-implant restorations after local bone grafting in maxillas: A 3-year clinical prospective study case series. Clin Implant Dent. 2003; 5(2): 63-70.
25. Kois JC, Kan JYK. Predictable peri-implant gingival aesthetics: Surgical and prosthodontic rationales. Pract Proced Aesthet Dent. 2001;13(9):691-698.
26. Myenberg KH, Imoberdorf MJ. The aesthetic challenges of single tooth replacement: A comparison of treatment alternatives. Pract Proced Aesthet Dent. 1997;9(7): 727-735.
27. Cobb GW, Reeves GW, Duncan JD. Guided tissue healing for single-tooth implants. Compend Contin Educ Dent. 1998;20(6):571-582.
28. Macintosh DCT, Sutherland M. Method for developing an optimal emergence profile using heat-polymerized provisional restorations for single-tooth implant-supported restorations. J Prosthet Dent. 2004;91(3):289-292.
29. Mitrani R, Phillips K, Kois JC. An implant-supported, screw-retained, provisional fixed partial denture for pontic site enhancement. Pract Proced Aesthet Dent. 2005;17(10): 673-678.
30. Touati B. Biologically driven prosthetic options in implant dentistry. Pract Proced Aesthet Dent. 2004;16(7):517-520.
|  Figure 3 A periapical radiograph revealed extensive root resorption of the endodontically treated tooth. | |
 |  | |
| Figure 4 After atraumatic tooth removal, osteotomes were used to prepare the implant site. | Figure 5 An OSSEOTITE Certain Implant was placed immediately into the extraction site without raising a soft-tissue flap. | |
 |  | |
| Figure 6 The PreFormance Post was marked intraorally and then easily modified on a laboratory holder with a coarse high-speed diamond bur. | Figure 7 With the modified post reseated intraorally, a vacuum-formed matrix was filled with bis-acryl resin, seated over the post, and removed before final setting of the resin. | |
 |  | |
| Figure 8 The post and provisional crown were removed from the mouth and placed onto a laboratory holder to refine the contours and finish the restoration. | Figure 9 The provisional crown, with a mesial diastema initially requested by the patient, was cemented with temporary cement over the modified PreFormance Post. | |
 Figure 10 An Encode Patient Specific Final Abutment and ceramic crown, with the diastema closed, were seated on the internally interfaced OSSEOTITE Certain Implant. | 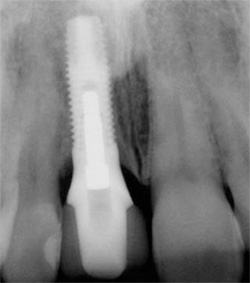 | |
| Figure 11 Continuity of the emergence profile from implant to abutment to crown is displayed on a postoperative periapical radiograph. | ||
| About the Author | ||
 George Priest, DMD George Priest, DMD Private Practice in Prosthodontics Atlanta, Georgia Former Clinical Professor Department of Graduate Prosthodontics Emory University President Priest Prosthodontic Productions Atlanta, Georgia | ||





