Conservative Treatment of an Endodontic and Esthetic Failure in a Young Patient
Richard Trushkowsky, DDS
When a patient presents for treatment, the treating dentist should ascertain if there is a chief complaint that needs to be addressed. If the complaint isn’t of an immediate nature, a complete examination including chief complaint, medical history, radiographs, intraoral and extraoral examination of hard and soft tissues, and possibly photographs and study models should be obtained. After all the records are assessed, treatment options should be presented to the patient. The treatment may possibly involve different dental disciplines and may have to be extended over a period of time to achieve the best outcome.
Retreatment of dentistry performed by a previous dentist is always difficult for the current dentist and the patient. Because you are not aware of the circumstances of the initial treatment, it is best to present the current problem and your suggestions to correct the problem. Failing endodontic treatment can be treated by an apicoectomy or retreatment. In advanced cases, removal of the tooth and implant placement should be considered if the long-term prognosis is poor. Leaving the offending tooth may jeopardize subsequent implant placement. Large periapical lesions have healed with conservative treatment with calcium hydroxide dressing and even without the calcium hydroxide dressing, if a favorable environment is created for healing.1-3 If an apicoectomy is needed, the modern technique includes root-end resection with minimal or no bevel and retrograde preparation with retro-tips and possibly a dental operating microscope. The traditional technique includes root-end resection with a 45-degree bevel angle and a retrograde preparation using a carbide round bur.4
CASE REPORT
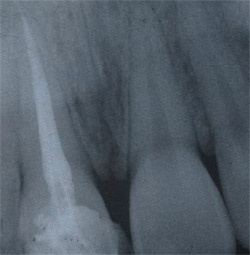
A 12-year-old girl presented with esthetics of tooth No. 8 that were unacceptable to the patient and her mother. The patient’s tooth had been traumatized and fractured several years before her visit. She had subsequent endodontic treatment and a porcelain crown fabricated at that time. Clinical and radiographic examination revealed a failing root canal in tooth No. 8 because of poor obturation (Figure 1) and a crown that was improperly contoured (Figure 2). The patient and parent were advised that before addressing the esthetic problem, the failed root canal would need to be retreated.
The gutta percha was removed from the canal and calcium hydroxide placed for a period of 2 weeks. Calcium hydroxide changes the pH of the canal, rendering it more basic and promoting periapical repair.1-3 The tooth was then filled with Resilon™ using the Epiphany® Soft Resin Endodontic Obturation System (Pentron Clinical Technologies, LLC, Wallingford, CT) (Figure 3). Torabinejad and associates demonstrated that bacteria can penetrate to the apex in coronally unsealed, endodontically treated teeth in only 18 days.5 Other studies have shown that removal of the smear layer and the placement of an epoxy resin or glass ionomer sealer decreases coronal microleakage, and even the placement of a 1-mm layer of a resin-modified glass ionomer, Vitrebond™ Plus Glass Ionomer Restorative (3M™ESPE™, St Paul, MN) over the openings to the canal decreases leakage to zero.6 The Resilon material was selected to minimize any microleakage and promote apical healing.7-10 Studies confirming the possibility of strengthening the root with the root canal filling material seems to be equivocal.11,12
The Resilon System technique is similar to gutta percha and sealer. After the last irrigation with sodium hypochlorite, EDTA should be placed in the canal to remove the smear layer and then the canal should be washed and dried with paper points. In this case the self-etching primer was placed into the canal with a small brush or paper points, and excess was removed with dry paper points. The dual-cure Resilon sealer was expressed from the automix syringe onto a coated pad. The canal was coated with lentulo, using a file or paper point. The Resilon point was also coated. The viscosity of the sealer can be modified with the thinning resin if desired. The point was placed to length and a radiograph was taken to ensure complete seating. In this case, the System B Element Obturation unit (SybronEndo, Orange, CA) was set at 150° C and power at 10. The excess was removed to the level of the orifice with the hot plugger. The coronal surface of the material was light-cured for 40 seconds, and the cement set in 25 minutes.10
A 6-month waiting period was elected to evaluate periapical repair before completing the definitive restoration (Figure 4). The patient wanted the teeth lightened, so they were bleached with a vital nightguard bleaching regimen for 2 weeks (Opalescence® 10%, Ultradent Products, Inc, South Jordan, UT). To evaluate the final shape of tooth No. 8, it was recontoured, etched with hydrofluoric acid, and composite was bonded (OptiBond® Solo Plus® Kerr Corporation, Orange, CA) and Simile® Nano-Hybrid Composite (Pentron) to the mesial and distal incisal edges to create more natural incisal embrasures (Figure 5). Teeth Nos. 9 and 10 were also bonded to close spaces and correct mesial?distal dimensions. An alternative would have been porcelain veneers, but the age of the patient precluded this; bleaching and interproximal bonding achieved the desired effect.
The old ceramic crown was removed after the 6-month radiograph revealed good healing. It was felt a post would be needed to retain the core build-up that was required. If sufficient tooth structure remains (half the height of the new crown) a crown can be fabricated without a post and a tooth-colored composite bonded into the access opening.13 Considerations for post selection have to be predicated upon functional and esthetic needs. If an adequate ferrule is present, it will negate most of the problems (root fracture) associated with a metal post.14
The next consideration is esthetics. Light transmission is facilitated by use of a ceramic (zirconium) or fibered (quartz or glass fiber) post.15 A prefabricated metal post (ParaPost®, Coltène/Whaledent, Cuyahoga Falls, OH) was selected because of the author’s many years of success with this system. The patient didn’t have a high smile line and didn’t have a thin gingival biotype, so a dark shadow wouldn’t be noticed at the gingival margin. However, a tooth-colored post would have made crown fabrication easier for the laboratory and allowed more versatility in material choices for the crown.
The shade was selected by the laboratory (Figure 6). Procera® (Noble Biocare™ USA Inc, Yorba Linda, CA) was selected to mask any shadow from the post and discolored tooth structure (Figure 7). The root of tooth No. 8 was tilted slightly labially and caused the post to be angled toward the labial. To keep an adequate length of the post, the labial reduction was limited. This allowed the laboratory only 0.7 mm to 0.8 mm of thickness on the labial for ceramic material (Figure 8). The other alternative would have required a cast post to change the emergence angle from the canal. The marginal accuracy of the Procera crown would also eliminate or reduce any microleakage. The crown can also be luted by conventional or adhesive techniques.16,17 RelyX® Luting Plus (3M™ESPE™) was used because of its adhesive qualities. Then tooth No. 9 had the mesial restored (Figure 9) with OptiBond Solo Plus and Filtek™ Supreme Plus shades B1 and WE (3M™ESPE™) to match the diameter, shape, and shade of tooth No. 8 (Figure 10A and Figure 10B).
CONCLUSION
Treatment planning for a patient often involves several viable options. Depending on the individual patient and dentist, these may vary considerably. In this case report, the chief complaint was the esthetic appearance of the right central incisor. To expedite the case, an apicoectomy could have been performed on tooth No. 8 rather than retreatment. The varieties of posts available, if they are needed to support the core, have many advantages and disadvantages. The individual situation should dictate the appropriate choice. The same is true of the crown selected. In the case presented, an opaque core was needed to mask the preparation yet provide good optical qualities. A Captek Crown (Precious Chemicals, Inc, Altamonte Springs, FL) would also have been a feasible alternative. There are often many treatment options that can provide good results. Understanding the desires of the patient and the skills of the restorative dentist are key factors in the final treatment recommended.
ACKNOWLEDGEMENT
The author wishes to thank Peter Pizzi, CDT, MDT, of Pizzi Dental Studio, Inc, for the Procera restoration and some of the photographs.
References
1. Lee MT. Conservative endodontic management of teeth associated with extensive periapical pathology: report of two cases. Aust Endod J. 2004;30(3): 103-109.2. Oztan MD. Edodontic treatment of teeth associated with a large periapical lesion. Int Endod J. 2002;35(1):73-78.
3. Weiger R, Rosenhahl R, Lost C. Influence of calcium hydroxide intracanal dressings on the prognosis of teeth with endodontically induced periapical lesions. Int Endod J. 2000;33(3):219-226.
4. Tsesis I, Rosen E, Schwartz-Arad D, et al. Retrospective evaluation of surgical endodontic treatment: traditional versus modern technique. J Endod. 2006;32(5):412-416.
5. Torabinejad M, Ung B, Kettering JD. In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod. 1990;16(12):566-569.
6. Chailertvanitkul P, Saunders WP, Saunders EM, et al. An evaluation of microbial coronal leakage in the restored pulp camber of root-canal treated multirooted teeth. Int Endod J. 1997;30(5):318-322.
7. Ezzie E, Fleury A, Solomon E, et al. Efficacy of retreatment techniques for a resin-based root canal obturation material. J Endod. 2006;32(4):341-344.
8. Shipper G, Orstavik D, Teixeira FB, et al. An evaluation of microbial leakage in roots filled with a thermoplastic synthetic polymer-based root canal filling material (Resilon) J Endod. 2004;30(5):342-347.
9. Shipper G, Teixeira FB, Arnold RR, et al. Periapical inflammation after coronal microbial inoculation of dog roots filled with gutta-percha or resilon. J Endod. 2005;31(2):91-96.
10. Aptekar A, Ginnan K. Comparative analysis of microleakage and seal for 2 obturation materials: Resilon/Epiphany and gutta-percha. J Can Dent Assoc. 2006;72(3):245.
11. Chivian N. Resilon?the missing link in sealing the root canal. Compend Contin Ed Dent. 2004;25(10A):823-824.
12. Teixeira FB, Teixeira EC, Thompson JY, et al. Fracture resistance of roots endodontically treated with a new resin filling material. J Am Dent Assoc. 2004:135(5):646-652.
13. Gesi A, Rafaelli O, Gorracci C, et al. Interfacial strength of Resilon and gutta-percha to intraradicular dentin. J Endod. 2005;31(11):809-813.
14. Zalkind M, Hochman N. Esthetic considerations in restoring endodontically treated teeth with posts and cores. J Prosthet Dent. 1998;79(6): 702-705.
15. Rosentritt M, Furer C, Behr M, et al. Comparison of in vitro fracture strength of metallic and tooth-coloured posts and cores. J Oral Rehabil. 2000;27(7):595-601.
16. Ritter RG. Selecting from post-and-core options to ensure anterior esthetic continuity. Inside Dentistry 2006;2(4):41-42.
17. Albert FE, El-Mowafy OM. Marginal adaptation and microleakage of Procera allCeram crowns with four cements. Int J Prosthodont. 2004;17(5);529-535.
18. Quintas AF, Oliveira F, Bottino MA. Vertical marginal discrepancy of ceramic copings with different ceramic materials, finish lines, luting agents: an in vitro evaluation. J Prosthet Dent. 2004;92(3): 250-257.
 |  | |
| Figure 1 Tooth No. 8 with large area and gutta percha removal. | Figure 2 Poor esthetics of original crown creates a negative central viewing focus. | |
 |  | |
| Figure 3 Tooth No. 8 immediately after filling with Resilon. | Figure 4 Tooth No. 8 after 6 months demonstrates healing. | |
 | ||
| Figure 5 Mesial and distal of original crown on tooth No. 8 recontoured and added to with composite to create a more pleasing and natural shape. Tooth No. 9 mesial bonded with composite to close diastema. | ||
 |  | |
| Figure 6 Shade is selected from cervical one third. | Figure 7 Initial try-in of crown demonstrates stump darkened by post. | |
 |  | |
| Figure 8 A caliper demonstrates the thickness of the Procera crown. | Figure 9 Procera crown on model demonstrates the space that needs to be closed with bonding to create the correct proportions. | |
 |  | |
| Figure 10A Normal smile reveals excellent esthetics of teeth Nos. 8 and 9. | Figure 10B Parted lips demonstrates incisal edge touching the vermillion border of the lip. | |
| About the Author | ||
 Richard Trushkowsky, DDS Richard Trushkowsky, DDSPrivate Practice Staten Island, New York | ||



