A Multidisciplinary Approach to Implant Restoration and Provisionalization in the Esthetic Zone
Anthony M. Polimeni, DMD; Gary Alex, DMD
Implant restoration in the esthetic zone requires precise coordination between all members of the dental team. This coordinated approach to treatment is exemplified in the cases provided in this article, which required the expertise of an implant surgeon, an orthodontist, a restorative dentist, and a laboratory technician. Orthodontic extrusion for site development was used in both cases. Occasionally, planned immediate implant placement and provisionalization are found to not be possible at the time of surgery. These potential problems are also discussed in this article.
Recently, much of the focus and attention in implant dentistry has been on implant placement and provisionalization immediately after tooth extraction. Studies have shown that, under favorable conditions, the success rates of immediate implant placement and loading rival that of the traditional implant surgical/restorative protocols.1-3 When working in the esthetic zone, immediate implant placement and provisionalization after extraction has several advantages, including decreased treatment time, no need for removable temporaries, and better maintenance of the hard and soft tissue profile to help maximize esthetics. Although a case might initially be treatment-planned for immediate implants, there are times when, at the time of surgery, immediate implant placement and provisionalization may be risky or impossible. Compromised socket anatomy, the presence of active infection, the inability to control occlusal loads, and the inability to obtain a high level of initial stability upon implant placement are just a few contraindications to immediate implant placement and provisionalization.4 In such cases, it is important to have a secondary plan for temporization in place so that the dentist, who was planning on an immediate implant-supported provisional, is not scrambling to determine how to temporize the case after the tooth or teeth have been extracted.
The following case presentations illustrate two different clinical situations. The first case demonstrates immediate placement and provisionalization as was originally treatment-planned. In the second case, it was discovered at the time of surgery that immediate implant placement and provisionalization could not be carried out as originally planned. In this case, execution of a secondary contingency plan still enabled the case to be easily provisionalized with a removable appliance made in advance. In both cases, orthodontic extrusion was first performed on the teeth being extracted to optimize the hard and soft tissue profile and gingival levels.
First Case Presentation
The first case involved a 36-year-old woman with an unremarkable medical history who was initially referred to the office for a preorthodontic evaluation. Her periodontal status was deemed stable and healthy and she was cleared for orthodontic treatment. Approximately 18 months into orthodontic therapy, she began to experience extreme sensitivity and occasional pain of the upper right central incisor. The patient was referred to an endodontist and diagnosed with irreversible pulpitis that was subsequently treated with conventional endodontics. The patient’s pain persisted and ultimately an apicoectomy was required. The tooth soon developed clinical signs and symptoms consistent with root fracture. Two millimeters of recession and periodontal probing of 4 mm on the direct facial was noted. Because the patient was still in active orthodontic treatment, the decision was made to ortho-dontically erupt this tooth to develop the site for a single-tooth implant and create a more favorable bone crest/gingival margin relationship for subsequent implant placement (Figure 1A, Figure 1B, Figure 1C).5
The patient returned to the office after orthodontic treatment and debanding (Figure 1D). The treatment plan was to extract the tooth and immediately place the implant and provisional. It was assumed conditions would be favorable for this at the time of surgery. A temporary abutment and crown were prepared on a model before the scheduled surgery. If immediate placement and provisionalization could not be performed, the contingency plan was to graft the area for future implant placement and use an orthodontic retainer with an acrylic tooth built in for temporization.
The tooth was carefully extracted and the socket anatomy was checked to make sure the facial cortical plate was intact (Figure 1E). A 5-mm x 16-mm tapered implant (Replace® Select Implants, Nobel BioCare, Yorba Linda, California) was carefully placed in the extraction site. After placement to the desired depth, the implant was torque-tested to 35 Ncm with no evidence of rotation. This indicated good initial implant stability.
A temporary abutment was then placed and hand-tightened. The prefabricated temporary crown was relined with acrylic, smoothed and polished, then temporarily cemented onto the abutment (Figure 1F). Occlusion was checked so that the provisional did not contact in centric occlusion and was clear of any lateral and protrusive interference. Two sutures were placed to adapt the tissues around the temporary (Figure 1G). The sutures were removed after 2 weeks and the occlusion was again checked. The patient wore the provisional for 4 months to allow the tissues to heal and stabilize before the definitive restoration.
The implant was ultimately restored using a Procera® all-ceramic abutment and Procera® crown (Nobel BioCare). A Procera crown was also placed on tooth No. 9 to optimize the esthetic result (Figure 1H, Figure 1I, Figure 1J).
Second Case Presentation
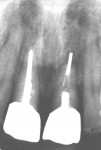
A 44-year-old woman was referred for evaluation of the upper right and left central incisors. Approximately 10 years earlier, these teeth experienced trauma and endodontic treatment. The teeth were restored with conventional posts, core build-ups, and unesthetic crowns. The patient had noticed progressive loosening of these teeth and the space between them “seemed to be getting worse” (Figure 2A and Figure 2B). Radiographs demonstrated a breakdown of osseous support and severely compromised and failing teeth (Figure 2C).
Clinical examination revealed Class 2 mobility with significant fremitus on both central incisors in centric closure. Various options were discussed with the patient and the decision was made to extract these teeth and replace them with dental implants.
A key component to implant therapy in the maxillary anterior is proper evaluation of the future implant sites. Several important hard and soft tissue considerations should be evaluated before implant placement.6-8 After evaluating the existing height of the central papilla, the position of the free gingival margins, and the existing bony architecture, it was determined that orthodontic extrusion of the centrals before extraction would help optimize the hard and soft tissue profile and allow for the best possible final esthetic result (Figure 2D).
As the orthodontic phase of treatment was nearing completion, the plan was to extract both central incisors and replace them immediately with implants, temporary abutments, and provisionals. Upon extraction and placement of two 5-mm x 16-mm tapered Replace Select Implants, the implant in the tooth No. 8 position did not torque-test to 35 Ncm. Failure of an implant to resist torque-testing indicates poor initial stability and is a contraindication for immediate loading and provisionalization.4 Because of this, the decision was made to fall back on the contingency plan for temporization. Healing abutments measuring 3 mm high were placed rather than cover screws to help develop and support the soft tissue profile during the integration phase of healing (Figure 2E). A removable temporary appliance replacing the central incisors had already been fabricated before the surgery and was ready to use as part of the back-up plan. This appliance was constructed with clasps and definitive occlusal stops on the lateral incisors to avoid pressure on the implants during healing (Figure 2F and Figure 2G).
Because the implants were not immediately loaded and provisionalized on the day of surgery, the temporary removable appliance was placed and adjusted. Occlusion was carefully checked and the underside of the pontics was adjusted to clear the underlying tissue drape and healing abutments. The patient was able to leave the office with a well-fitting removable temporary appliance, which satisfied the initial esthetic and functional requirements of the case (Figure 2H). Typically, only the laboratory cost of the temporary appliance is transferred to the patient. This additional fee is negligible compared to the importance of having a contingency temporary available for the patient should it be required as seen in this case.
After 4 months, excess tissue was cleared from around the healing abutments using a biopsy punch (Figure 2I) and the prosthetic component of the case was completed. The central incisors were restored with ceramic abutments and Procera crowns (Figure 2J, Figure 2K, Figure 2L). Careful treatment planning and attention to detail ultimately led to an excellent final esthetic and functional result.
Conclusion
Immediate placement and provisionalization of implants in the maxillary anterior after extraction is almost always the treatment of choice when conditions are favorable. Shortened treatment time in conjunction with fixed provisionals is always preferable. The esthetic and functional advantage of this treatment is clear. Occasionally, immediate provisionalization may be impossible or risky at the time of surgery. The two cases presented in this article were both treatment-planned for immediate placement and immediate provisionalization. However, at the time of surgery it was determined that one case did not meet the criteria for immediate loading and provisionalization. In that instance, the importance of having a contingency plan for provisionalization, which does not require implant support, has been demonstrated.
Acknowledgment
The authors wish to thank Dr. Rob Schindel and Dr. Alan Gibbs for their fine orthodontic contributions to the success of these cases. We would also like to thank Frank Saccente of Roslyn Dental Laboratories for his beautiful ceramic work.
References
1. Wohrle PS. Single-tooth replacement in the esthetic zone with immediate provisionalization: fourteen consecutive case reports. Pract Periodontics Aesthet Dent. 1998;10(9):1107-1114.
2. Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year retrospective study. Int J Oral Maxillofac Implant. 2003;18(1);31-39.
3. Ericsson I, Nilsson H, Lindh T, et al. Immediate functional loading of Branemark single tooth implants. An 18 months’ clinical pilot follow-up study. Clin Oral Implants Res. 2000;11(1):26-33.
4. Immediate Function Guidelines. Prerequisites for Immediate Function. A Protocol for One Stage Branemark Implants. NobelBiocare Web site. Available at: https://www.nobelbiocare.com/global/en/ClinicalProcedures/ImmediateFunction/prerequisites.htm. 2004.
5. Salama H, Salama M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: a systematic approach to the management of extraction site defects. Int J Periodontics Restorative Dent. 1993;13(4): 312-333.
6. Tarnow DP, Chao SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
7. Kan JY, Rungcharassaeng K, Umezu K, et al. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol. 2003;74(4):557-562.
8. Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001;22(3): 199-206.
About the Authors
Anthony M. Polimeni, DMD
Private Practice Limited to Periodonticsand Dental Implant Surgery
Huntington, New York
Gary Alex, DMD
Private Practice
Huntington, New York