You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Xerostomia-also referred to as dry mouth, mouth dryness, or oral dryness-is defined as subjective dryness of the oral cavity that is typically associated with salivary hypofunction (ie, decreased salivary flow).1,2 It is notable that even in the presence of normal salivary function, some patients experience subjective symptoms of oral dryness, which may be referred to as symptomatic xerostomia and can be differentiated from primary or true xerostomia-decreased salivary secretory function-through assessment of salivary flow rates.3,4In this way, xerostomia is both a sign and a symptom. In a patient who reports dry mouth, clinical assessment of the signs of xerostomia, including reduced salivary flow, thick or ropey saliva, salivary frothing, and/or glazing of oral mucosa, can identify quantitative reduction in saliva.5 In the absence of these symptoms, a significant number of patients still express the sensation of oral dryness. In such patients, qualitative changes in salivary composition and properties and/or alterations in the patient's perception may be the underlying causes for these reports.5
Given the frequency of patient reports of oral dryness, it is imperative that dental healthcare professionals understand this condition and its impact on oral and overall health. Proper screening for symptoms and determination of the underlying causes of xerostomia symptoms in clinical dental practice can allow for targeted treatment and improved oral health, general well-being, and quality of life. This article will review the diagnosis, prevalence, etiology, and oral complications associated with the condition and treatment of xerostomia and the opportunities for dental healthcare professionals to impact patients experiencing oral dryness.
What Is Xerostomia?
Xerostomia is defined as the subjective sensation of oral dryness.1,2,6 This is often, but not always, associated with hyposalivation-the objective finding of decreased salivary production. It is important to note that xerostomia may be present in patients with normal salivation rates and, conversely, individuals with very low salivary flow rates may not report xerostomia.7,8
The majority of saliva is produced by the paired major salivary glands. The parotid, submandibular, and sublingual glands account for approximately 90% of overall oral saliva production.5,9 Additionally, minor salivary glands located throughout the mouth on the cheeks, lips, palate, tongue, and oropharynx produce the remaining salivary flow. Salivary production is assessed at rest (unstimulated salivary flow) and with stimulation by mastication. Normal unstimulated salivary flow is, on average, 0.3 mL/minute.5, 10-12 This can increase to greater than
3 mL/minute when stimulated.5,10,11 Given these flow rates, it has been estimated that total daily salivary production in normal individuals is approximately 500-600 mL.5,11,13 It has also been suggested that flow rates that demonstrate a 45% decrease from normal levels can be considered a "cut off" for hyposalivation.12
In clinical practice, it is important to emphasize that many patients with subjective xerostomia may not show a decrease in salivary flow rates when assessed. Such patients may experience changes in salivary composition impacting the visco-elasticity of the saliva, alterations in oral fluid absorption rates, and/or altered perception which can impact the sensation of dry mouth that they experience.14,15 Patient reports of xerostomia symptoms are quite high and may vary based upon age and underlying medical conditions. Estimates of xerostomia prevalence in the general population are limited due to small samples and lack of consistent diagnostic criteria. It has been reported that xerostomia prevalence in the general population ranges from 0.9% to 64.8%.16 In people with some autoimmune conditions such as Sjögren disease or in those receiving radiation therapy for head and neck cancer, the prevalence approaches 100%.16
What Causes Xerostomia?
Drug and/or Medical Treatment Related Causes
Medication use is often associated with subsequent hyposalivation.17 According to the Surgeon General's Report on Oral Health in America, over 400 over-the-counter (OTC) and prescription medications may be associated with increased xerostomia. The most common types of medications causing salivary dysfunction have anticholinergic effects, eg, tricyclic antidepressants, antihistamines, antihypertensive medications, and antiseizure/antispasmodic drugs.16-18 Polypharmacy (taking multiple medications) may also increase the risk of experiencing xerostomia.19,20 It is important to understand the potential effects of medications on xerostomia to allow for medical consultations and potential drug substitutions as a mechanism to reduce symptoms. For example, while both selective serotonin-reuptake inhibitors (SSRIs) and tricyclic antidepressants can be used to treat mental health disorders, the incidence of xerostomia associated with SSRIs is significantly lower, and substitution could improve drug compliance in a patient with severe symptoms.17,18Additionally, as salivary flow is decreased in the overnight hours, shifting when medications are taken or utilizing divided doses could improve symptoms for some patients.17,18
Oral complications of cancer chemotherapy and/or head and neck radiation are often reported to include acute, chronic, or delayed onset xerostomia.16,18,21Such treatments can affect salivary function by their direct toxicity on salivary tissues or may cause systemic toxicity that alters fluid balance throughout the body.18,21 Xerostomia symptoms associated with chemotherapies are generally acute, and most resolve after completion of treatment and a healing period for damaged tissues.21 Conversely, radiation therapy may result in chronic or delayed-onset oral toxicity, putting such patients at continued long-term risk of xerostomia after treatment.21
Physiological or Disease-Related Causes
Xerostomia prevalence increases with age, although it has been debated if age is a risk factor on its own, or if older individuals simply have a higher rate of cumulative risk factors for xerostomia.21Regardless, xerostomia affects 30% of patients older than 65 years and up to 40% of patients older than 80 years.20,22-25 The increase in xerostomia symptoms seen in an older population has primarily been attributed to an adverse effect of medication(s) and/or comorbid conditions.20,22
Autoimmune conditions, such as Sjögren disease, have also been highly associated with xerostomia. Sjögren disease is the second most common autoimmune connective-tissue disease and is the systemic condition most frequently associated with salivary dysfunction and xerostomia.24 Primary symptoms of Sjögren disease are dry mouth and dry eyes.24 The autoimmune dysfunction that results in tissue destruction in Sjögren disease is due to chronic inflammation within local tissues resulting in salivary gland damage.24Primary Sjögren disease (ie, Sjögren disease alone) affects approximately 1 in 70 people. Further, Sjögren disease is often observed in combination with other autoimmune disease (eg, rheumatoid arthritis, systemic lupus erythematosus, scleroderma, polymyositis, and polyarteritis nodosa).24
Xerostomia has also been associated with a number of other systemic diseases and conditions. These are summarized in Table 1. Additionally, emerging data have suggested that xerostomia has been seen as an early and/or prodromal symptom of primary COVID-19 infection.26 It is unknown how frequently xerostomia resolves after COVID-19 treatment and/or other symptoms, but this may be elucidated in the future.26,27It should also be noted that potential lifestyle causes of xerostomia include the use of alcohol or tobacco, or the consumption of excessive caffeine or spicy food.16
Oral and Overall Impacts of Xerostomia
Patients who report xerostomia have multiple oral and overall health consequences. Adequate quantity and quality of saliva is critical for maintenance of oral and gastro-intestinal health. In the presence of salivary dysfunction and/or subjective oral dryness, patients may experience increased rates or severity of dental caries, gingival inflammation, periodontitis, as well as other oral conditions.28 It is also notable that adequate quality and quantity of saliva is required to experience appropriate taste sensations and digestion. Xerostomia and taste disturbances may have an impact on patients' food and beverage choices and could therefore compromise nutritional status.29 Saliva is also required for the proper functioning of many fixed and removable dental prostheses. The lubrication provided by saliva allows for proper retention of removable dental appliances, and a lack of saliva can result in traumatic oral lesions.30
Dental caries and periodontitis are the two most prevalent oral diseases, and both are more common in older individuals.31,32Decreased salivary flow rates have been associated with increased caries rates with a particularly impactful association between xerostomia and radicular caries.33,34 Without adequate salivary flow to re-establish oral pH levels above critical demineralization values and to facilitate a healthy oral microbiome, low oral pH levels and dysbiotic biofilm can increase the development and progression of dental caries.28 Dental plaque induced gingivitis has been shown to be worsened by oral dryness35 and periodontal disease incidence and severity has been associated with xerostomia.36,37Poorer periodontal conditions in patients with xerostomia is attributed to the decrease in saliva and subsequent increase in plaque adherence and pathogenicity.38
Xerostomia has also been associated with a host of other oral conditions, including dysphagia, taste disturbances, impaired speaking abilities, halitosis, burning mouth sensation, and oral candidiasis.39-44Such alterations may impair the nutritional intake, communication, and social interactions of individuals with xerostomia and could lead to feelings of isolation, stigmatization, and overall decreased well-being in these patients. Many of the symptoms associated with xerostomia can have a negative impact on overall quality of life4-6,45 and a potential clustering of such symptoms in at-risk individuals could be particularly impactful on their mental and physical wellness.
Diagnosis and Management of Xerostomia in Clinical Practice
Given that patients experiencing symptoms of xerostomia may or may not have alterations in salivary flow and that not all patients with hyposalivation experience a sensation of oral dryness, a combination of subjective and objective assessments is recommended to fully assess patients' clinical presentation and treatment needs. Furthermore, patients have been shown to underestimate the importance and/or severity of their xerostomia symptoms and may not report them to their dental healthcare provider unless explicitly asked.6,46
Diagnosis and Assessment
Utilization of both objective and subjective tools can help practitioners best classify xerostomia, understand the sequelae related to oral dryness in a particular patient, and effectively treat the underlying causes. Deploying a screening questionnaire to all patients with suspected xerostomia can aid in adequately describing the symptoms that patients are experiencing and their frequency and severity.4,47,48Table 2 provides a summary of the questionnaire. In addition to subjective assessment, objective measurement of unstimulated (resting) and stimulated salivary flow rates are recommended in individuals with a complaint of dry mouth.49,50Equipment required for such measurements includes: a collection tube, funnel, pH paper strips, and Schirmer test strips. Prior to salivary testing, patients should present to the office NPO (ie, nothing by mouth) for 2 hours. It should also be requested that patients refrain from chewing gum, toothbrushing, or flossing during this time. Unstimulated saliva is collected with the patient sitting on the edge of the dental chair and the head of the patient tipped forward to allow passive flow of saliva into the funnel, which is placed on his/her open lips. The collection generally is undertaken for 5 minutes and the per-minute average assessed.51 Stimulated salivary flow measurements occur in much the same manner, but they would be made following chewing of a paraffin block for 1 minute or after a test dose of salivary stimulation medication has been administered. Salivary pH has been inversely correlated with flow rates and may be assessed with the use of pH paper strips. Normal salivary pH ranges between 7 and 7.5, which is neutral to slightly alkaline.52 Low salivary pH may indicate an increased risk of tooth erosion, mucosal irritation, or burning mouth symptoms. Average unstimulated salivary flow rates range between 0.3 mL/minute and
0.4 mL/minute.11,12In a symptomatic patient, flow rates below 0.3 mL/minute would indicate hyposalivation and those who demonstrate an unstimulated salivary flow rate below 0.1 mL/minute are considered to have severe salivary gland dysfunction.12,50
Management of Xerostomia in Dental Practice
Treatment of xerostomia is a complex process that may require multidisciplinary therapy to fully address. Careful assessment to determine the pharmacologic and nonpharmacologic mechanisms of treatment should be undertaken if a patient is diagnosed with xerostomia and/or hyposalivation.
Initially, identification of underlying causes may present strategies to address symptoms and decrease the incidence of development of severe dental diseases, including dental caries and periodontal disease. For example, in patients with medication-induced xerostomia, medical consultation to develop a plan that may alter medications, dosages, and/or time of administration may result in a reduction in xerostomia symptoms.53 Increased water intake and/or dietary analysis and nutritional counseling can also result in symptom reduction for some patients.54Drinking 64 to 80 ounces of non-caffeine, non-alcoholic beverages daily has been suggested as an average goal for most patients to achieve and maintain optimal hydration.55 Patients with xerostomia should also be counseled about carbohydrate consumption and between-meal snacking as well as oral hygiene measures, including fluoride use, to reduce the risks of dental caries. It has also been suggested that patients with xerostomia should be seen by their dental healthcare professional for regular assessments and maintenance visits at least every 3 to 4 months to reduce the risks for periodontal disease and dental caries development and progression.
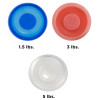
Other treatments for xerostomia include salivary replacement therapies (lubrication) and pharmacologic and nonpharmacologic therapies to optimize salivary flow rates. Salivary substitutes may increase comfort for patients when they are speaking at length or in those who have removable prostheses.50A summary of examples of OTC lubricating products is provided in Table 3. In some cases, pharmacologic and/or nonpharmacologic means must be employed to increase salivary flow rates to improve patients' symptoms. Cevimeline and pilocarpine are the best described and most commonly used medications to decrease xerostomic symptoms.6,56,57Both of these medications are parasympathomimetic agents with muscarinic and cholinergic-stimulating properties. Further, both require functional salivary glandular tissue that can be stimulated by their actions.58 Due to their mechanism of action, both medications have several untoward side effects that may be bothersome or even dangerous to some patients.58 Such cholinergic side effects include: nausea, emesis, bronchoconstriction, bradycardia, and hypotension.58 These medications are also contraindicated with several commonly prescribed medications, including parasympathomimetic drugs (eg, some antidepressants and clozapine) and beta-adrenergic agonists.58 Other medications that may be prescribed include bethanechol chloride, a cholinergic used to treat urinary retention due to bladder atony, and anethole trithione.59,60 Anethole trithione, in particular, may result in a synergistic effect when prescribed in combination with pilocarpine.59,60Prescription artificial saliva is also available as a salivary replacement in those who cannot tolerate a salivary stimulant or in whom a salivary stimulate fails to result in adequate salivary production.
Nonpharmacologic therapies for salivary stimulation include electrical stimulation and acupuncture. Both therapies have shown marked improvement in saliva production in patients with severe glandular injury after head and neck radiation.61,62 Other, more invasive, nonpharmacologic therapies have been proposed for those individuals with severe destruction of salivary glandular tissue, including gene and stem cell therapies to essentially "regrow" glandular tissue in situ.63 Continued study of the function and turnover of salivary cells may help elucidate the best applications of such advanced therapies in the future.
Summary
Patients experiencing xerostomia or hyposalivation may be identified in the dental office through careful survey and objective assessment of clinical signs and symptoms. Treatment should be multidisciplinary and multi-pronged; it should involve behavioral modification, risk assessment and mitigation for related oral diseases, and treatment to reduce symptoms and increase and/or replace salivary flow. Addressing the needs of patients with xerostomia can be a challenge for dental healthcare professionals, and clinicians should be aware of the best practices to diagnose and treat this condition.
About the Authors
Maria L.
Geisinger, DDS, MS
Professor
Department of Periodontology
University of Alabama at Birmingham
Birmingham, Alabama
Jennifer H.
Doobrow, DMD
Private Practice
Cullman, Alabama
References
1. Plemons JM, Al-Hashimi I, Marek CL; American Dental Association Council on Scientific Affairs. Managing xerostomia and salivary gland hypofunction: executive summary of a report from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2014;145(8):867-873.
2. Wolff A, Joshi RK, Ekström J, et al. A guide to medications inducing salivary gland dysfunction, xerostomia, and subjective sialorrhea: a systematic review sponsored by the World Workshop on Oral Medicine VI. Drugs R D. 2017;17(1):1-28.
3. Wiener RC, Wu B, Crout R, et al. Hyposalivation and xerostomia in dentate older adults. J Am Dent Assoc.2010;141(3):279-284.
4. Tanasiewicz M, Hildebrandt T, Oberszytn I. Xerostomia of various etiologies: a review of the literature. Adv Clin Exp Med. 2016;25(1):199-206.
5. Eveson JW. Xerostomia. Periodontology 2000. 2008;48: 85-91.
6. Barbe AG. Medication-induced xerostomia and hyposalivation in the elderly: culprits, complications, and management. Drugs Aging. 2018;35(10):877-885.
7. Screebny LM. Saliva in health and disease: an appraisal and update. Int Dent J. 2000;50(3):140-161.
8. Guggenheimer J, Moore PA. Xerostomia: etiology, recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
9. Thakkar JP, Lane CJ. Hyposalivation and xerostomia and burning mouth syndrome: medical management. Oral Maxillofac Surg Clin N Am2022; 34: 135-146.
10. Watanabe S, Dawes C. The effects of different foods and concentrations of citric acid on the flow rate of whole saliva in man. Arch Oral Biol. 1988;33(1):1-5.5.
11. Watanabe S, Ohnishi M, Imai K, et al. Estimation of the total saliva volume produced per day in five-year-old children. Arch Oral Biol. 1995;40(8):781-782.
12. Ghezzi EM, Lange LA, Ship JA. Determination of variation of stimulated salivary flow rates. J Dent Res. 2000;79(11):1874-1878.
13. Whaites E. Essentials of Dental Radiography and Radiology. 4th ed. Churchill Livingstone; 2007:448.
14. Dawes C. How much saliva is enough for avoidance of xerostomia? Caries Res. 2004;38(3):236-240.
15. van der Putten GJ, Brand HS, Schols JMGA, de Baat C. The diagnostic suitability of a xerostomia questionnaire and the association between xerostomia, hyposalivation and medication use in a group of nursing home residents. Clin Oral Investig.2011;15(2):185-192.
16. Anil S, Vellapppally S, Hashem M, et al., Xerostomia in geriatric patients: a burgeoning global concern. J Invest Clin Dent. 2016; 7(1): 5-12.
17. Terrie YC. Dry mouth: more common and less benign than thought. Pharmacy Times. 2016;82(2). https://www.pharmacytimes.com/view/dry-mouth-more-common-and-less-benign-than-thought. Published February 10, 2016. Accessed August 17, 2022.
18. Dawes C, Pedersen AML, Villa A, et al. The functions of human saliva: a review sponsored by the World Workshop on Oral Medicine VI. Arch Oral Biol.2015;60(6):863-874.
19. Agostini BA, Cericato GO, da Silveira ER, et al. How common is dry mouth? Systematic review and meta-regression analysis of prevalence estimates. Braz Dent J.2018;29(6):606-618.
20. Tan ECK, Lexomboon D, Sandborgh-Englund G, et al. Medications that cause dry mouth as an adverse effect in older people: a systematic review and metaanalysis. J Am Geriatr Soc. 2018;66(1):76-84.
21. Ouanounou A. Xerostomia in the geriatric patient: causes, oral manifestations, and treatment. Compend Contin Educ Dent. 2016;37(5):306-311.
22. Villa A, Connell CL, Abati S. Diagnosis and management of xerostomia and hyposalivation. Ther Clin Risk Manag. 2015;11:45-51.
23. Gupta A, Epstein JB, Sroussi H. Hyposalivation in elderly patients. J Can Dent Assoc2006; 72(9): 841-846.
24. Parisis D, Chivasso C, Perret J, et al. Current state of knowledge on primary Sjögren's syndrome, an autoimmune exocrinopathy. J Clin Med. 2020;9(7):2299.
25. American Dental Association Oral Health Topics. Xerostomia (Dry Mouth). Available at: https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/xerostomia Accessed August 2, 2022.
26. Fantozzi PJ, Pampena E, Di Vanna D, et al. Xerostomia, gustatory and olfactory dysfunctions in patients with COVID-19. Am J Otolaryngol. 2020;41(6):102721.
27. Fathi Y, Hoseini EG, Atoof F, Mottaghi R. Xerostomia (dry mouth) in patients with COVID-19: a case series. Future Virol.2021;16(5):315-319.
28. Turner MD, Ship JA. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc.2007;138(Suppl):S15-S20.
29. Hoffman HJ, Cruickshanks KJ, Davis B. Perspectives on population-based epidemiological studies of olfactory and taste impairment. Ann NY Acad Sci. 2009;1170:514-530.
30. Chandu GS, Hombesh MN. Management of xerostomia and hyposalivation in complete denture patients. Indian J Stomatol.2011;2(4):263-266.
31. Eke PI, Dye BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015;86(5):611-622.
32. Marthaler TM. Changes in dental caries 1953-2003. Caries Res. 2004;38(3):173-181.
33. Thompson WM. Epidemiology of oral health conditions in older people. Gerodontology. 2014;31(Suppl 1): 9-16.
34. Hayes M, Da Mata C, Cole M, et al. Risk indicators associated with root caries in independently living older adults. J Dent. 2016;51:8-14.
35. Chapple ILC, Mealey BL, Van Dyke TE, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S74-S84.
36. Lin CY, Tseng CF, Liu JM, et al. Association between periodontal disease and subsequent Sjögren's syndrome: a nationwide population-based cohort study. Int J Environ Res Public Health. 2019;16(5):771.
37. Mendes JJ, Viana J, Cruz F, et al. Radiographically screened periodontitis is associated with deteriorated oral-health quality of life: a cross-sectional study. PLoS One. 2022;17(6):e0269934.
38. Rhodus NL, Michalowicz BS. Periodontal status and sulcular Candida albicans colonization in patients with primary Sjögren's syndrome. Quintessence Int.2005;36(3):228-233.[CJ1]
39. Samnieng P, Ueno M, Shinada K, et al. Association of hyposalivation with oral function, nutrition and oral health in community-dwelling elderly Thai. Community Dent Health. 2012;29(1):117-123.
40. Brochier CW, Hugo FN, Rech RS, et al. Influence of dental factors on oropharyngeal dysphagia among recipients of long-term care. Gerodontology. 2018;35(4):333-338.
41. Koshimune S, Awano S, Gohara K, et al. Low salivary flow and volatile sulfur compounds in mouth air. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(1):38-41.
42. Bergdahl M. Salivary flow and oral complaints in adult dental patients. Community Dent Oral Epidemiol. 2000;28(1):59-66.
43. Nadig SD, Ashwathappa DT, Manjunath M, et al. A relationship between salivary flow rates and Candida counts in patients with xerostomia. J Oral Maxillofac Pathol. 2017;21(2):316.
44. Rawal S, Hoffman HJ, Bainbridge KE, et al. Prevalence and risk factors of self-reported smell and taste alterations: results from the 2011-2012 US National Health and Nutrition Examination Survey (NHANES). Chem Senses. 2016;41(1):69-76.
45. Botelho J, Machado V, Proença L, et al. Perceived xerostomia, stress and periodontal status impact on elderly oral health-related quality of life: findings from a cross-sectional survey. BMC Oral Health. 2020;20(1):199.
46. Barbe AG, Bock N, Derman SHM, et al. Self-assessment of oral health, dental health care, and oral health-related quality of life among Parkinson's disease patients. Gerodontology. 2017;34(1):135-143.
47. Glore RJ, Spiteri-Staines K, Paleri V. A patient with dry mouth. Clin Odolaryngol. 2009;34(4):358-363.
48. Al-Dwairi Z, Lynch E. Xerostomia in complete denture wearers: prevalence, clinical findings, and impact on oral functions. Gerodontology. 2014;31(1):49-55.
49. Sreebny LM, Vissink A. Dry Mouth, The Malevolent Symptom: A Clinical Guide.Wiley-Blackwell; 2010;35-45.
50. Zunt SL. Xerostomia/salivary gland hypofunction: diagnosis and management. Compend Contin Educ Dent.2018;39(6):365-372.
51. Fontana M, Zunt S, Eckert GJ, Zero D. A screening test for unstimulated salivary flow measurement. Oper Dent. 2005;30(1):3-8.
52. Whelton H. Introduction: the anatomy and physiology of salivary glands. In: Edgar M, Dawes C, O'Mullane D, eds. Saliva and Oral Health. 4th ed. Stephen Hancocks; 2012:11.
53. Sreebny LM, Valdini A. Xerostomia. A neglected symptom. Arch Intern Med.1987;147(7):1333-1337.
54. Kleiner SM. Water: an essential but overlooked nutrient. J Am Diet Assoc. 1999;99(2):200-206.
55. Ship JA, Fischer DJ. The relationship between dehydration and parotid salivary gland function in young and older healthy adults. J Gerontol A Biol Sci Med Sci. 1997;52(5):M310-M319.
56. Iwabuchi Y, Katagiri M, Masuhara T. Salivary secretion and histopathological effects after single administration of the muscarinic agonist SNI-2011 in MRL/lpr mice. Arch Int Pharmacodyn Ther. 1994;328(3):315-325.
57. Wiseman LR, Faulds D. Oral pilocarpine: a review of its pharmacologic properties and clinical potential in xerostomia. Drugs. 1995;49(1):143-155.
58. Villa A, Wolff A, Aframian D, et al. World Workshop on Oral Medicine VI: a systematic review of medication-induced salivary gland dysfunction: prevalence, diagnosis, and treatment. Clin Oral Investig. 2015;19(7):1563-1580.
59. Grisius MM. Salivary gland dysfunction: a review of systemic therapies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.2001;92(2)156-162.
60. Epstein JB, Decoteau WE, Wilkinson A. Effect of Sialor in treatment of xerostomia in Sjögren's syndrome. Oral Surg Oral Med Oral Pathol. 1983;56(5):495-499.
61. Simcock R, Fallowfield L, Monson K, et al. ARIX: a randomized trial of acupuncture v oral care sessions in patients with chronic xerostomia following treatment of head and neck cancer. Ann Oncol. 2013;24(3):776-783.
62. Aggarwal H, Pal-Singh M, Mathur H, et al. Evaluation of the effect of transcutaneous electrical nerve stimulation (TENS) on whole salivary flow rate. J Clin Exp Dent. 2015;7(1):e13-e17.
63. Pringle S, Van Os R, Coppes RP. Concise review: adult salivary gland stem cells and a potential therapy for xerostomia. Stem Cells. 2013;31(4):613-619.