You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
The AI Revolution: Transforming Dental Hygiene Care
Erin Kierce, RDH, MS, MPH; and Christopher Balaban, DMD, MSc
Unmet oral health needs continue to impact systemic health, remaining prevalent among the country's most vulnerable populations.1-5 Disparities, such as financial hardship, low health literacy, and inadequate access to care, result in higher rates of oral disease that often exacerbate other chronic conditions, including diabetes, cancer, and cardiovascular disease.1-3,6 In addition, considerations such as cultural and ethnic barriers and dental provider shortage areas further compound these inadequacies.1-7 Dental hygiene has long practiced on the standards of delivering comprehensive care through means reflective of emerging technology and scientific evidence. Innovative approaches to care, such as incorporating artificial intelligence (AI) technology into dental practice software, will assist dental providers in addressing these challenges by improving the standardization, method, and efficiency of each patient encounter.
Oral Health Disparities
Periodontal disease is evident in approximately 42% of American adults, with just under 8% exhibiting severe periodontitis.8 Approximately 92% of American adults between 20 and 64 years of age have had dental caries, while 26% have untreated decay.9 Among youth aged 2 to 19 years, the prevalence of total caries (untreated and treated) is about 45%, with 13% untreated. The prevalence was highest among youth between 12 and 19 years (53.8%), followed by 6-11 (50.5%) and 2-5 (21.4%).9 There is a higher prevalence of periodontitis and dental caries among African-Americans and Hispanics when compared to other racial or ethnic groups, and higher rates of disease are inversely correlated with an individual's level of income, education, and healthliteracy. This demonstrates that disparities remain for certain populations to obtain optimal oral health.5,10-13
The Institute of Medicine's 2011 Report, Im-proving Access to Oral Health Care for Vulnerable and Underserved Populations, was the first to reveal the systemic barriers facing vulnerable populations' access to oral health care. It specified how low health literacy, in addition to social, economic, and geographic factors, limits the capability of certain groups to understand the importance of oral health care, as well as recognize the risk for disease development and options for adequate treatment.14
A systematic review by DeWalt et al revealed low health literacy was associated with improper utilization of health resources, morbidity, and an increased risk of hospitalizations.15 Health literacy is defined by the Centers for Disease Control and Prevention as "the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others."
The approach to improving the health literacy of vulnerable populations must incorporate the proper provision of information, as well as utilize effective means of communication.10 For both approaches, it is necessary to first acknowledge the population's underlying determinants of health to tailor the delivery and content specific to the audience.6,7,10 The objective of improving health literacy is to empower individuals to promote sustained action towards health, promoting behavior by means of prevention or treatment.10,16
New technology and innovative approaches to care, such as artificial intelligence (AI), can address the barrier of health literacy by improving the method and means of patient education, standardizing care, facilitating clinical decision making, and promoting intra- and inter-professional collaboration. Using AI technology, dental providers can empower patients by means of presenting unambiguous and visual health information. This empowerment can improve comprehension irrespective of underlying determinants and ultimately increase rates of treatment acceptance and utilization.
AI and the Dental Hygiene Process of Care
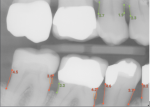
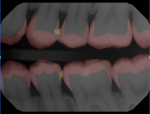
Since 2020, technological advancements have resulted in an exponential increase in the utilization of artificial intelligence in daily life, particularly in the field of dentistry. Leading dental clinicians are working with machine-learning scientists to develop and encode computer algorithms to measure and analyze radiographs, photographs, clinical assessments, and chart notes with dentist-level accuracy and understanding. This capability will result in a highly accurate output and clinically relevant results. Leading companies have developed algorithms to detect caries and periodontal disease, in addition to a wide array of clinical determinants. These algorithms and AI-enhanced software can help hygienists improve patient communication and demonstrate the necessity for treatment. The algorithms are built on millions of data points learned through rigorous clinical inputs, and are currently achieving equal to, and in some instances better than, single clinician accuracy.
Since 1985, dental hygiene has practiced on the standards of patient-centered, comprehensive care.17 The development and subsequent revisions of the Standards for Clinical Dental Hygiene Practice provides a framework for care reflective of competence, responsibility, and scientific evidence. The Standards describe a proficient level of dental hygiene practice that includes six components to the process of care: assessment, dental hygiene diagnosis, planning, implementation, evaluation, and documentation. 17 All components are correlated and dependent on the status of ongoing care, subsequent treatment outcomes, and patient needs. 17 The integration of AI technology into the dental hygiene process of care would improve the efficiency and efficacy of the assessment, dental hygiene diagnosis, planning, and evaluation. Navigating dental AI dashboards during patient care will become commonplace in the near future and will empower patients to be better informed in the decision process to accept warranted treatment.
Conclusion
While certain determinants for the development and progression of disease are well-understood (race/ethnicity, age, and gender), explicating the degree of understanding regarding other factors, such as health literacy, behavior, and social determinants, is limited.3-7,10 Low health literacy is associated with inadequate utilization of preventive services, higher rates of chronic disease, and poor health outcomes. Therefore, approaches to care that promote and improve health literacy should be prioritized. AI technology is a means by which dental providers can improve the approach to comprehensive and patient-centered care, reflective of underlying determinants of health, including low health literacy. AI can empower patients by standardizing the process of care and improving the accessibility of health information.
About the Authors
Erin Kierce, RDH, MS, MPH
Chief Compliance Officer, New England Family Dentistry
Adjunct Faculty, MCPHS University
Christopher Balaban, DMD, MSc
Clinical Director, Overjet AI
Clinical Faculty, Boston University
Private Practice, Boston, MA
References
1. Liu Y, Li Z, Walker MP. Social disparities in dentition status among American adults. Int Dent J.2014;64(1):52-57.
2. Borrell LN, Beck JD, Heiss G. Socioeconomic disadvantage and periodontal disease: the Dental Atherosclerosis Risk in Communities study. Am J Public Health. 2006;96(2):332-339.
3. Malecki K, Wisk LE, Walsh M, et al. Oral health equity and unmet dental care needs in a population-based sample: findings from the Survey of the Health of Wisconsin. Am J Public Health. 2015;105(Suppl 3):S466-S474.
4. Lee PH, McGrath CPJ, Kong AYC, Lam TH. Self-report poor oral health and chronic diseases: the Hong Kong FAMILY project. Community Dent Oral Epidemiol.2013;41(5):451-458.
5. Northridge ME, Kumar A, Kaur R. Disparities in Access to Oral Health Care. Annu Rev Public Health. 2020;41:513-535.
6. VanWormer JJ, Acharya A, Greenlee RT, Nieto FJ. Oral hygiene and cardiometabolic disease risk in the survey of the health of Wisconsin. Community Dent Oral Epidemiol.2013;41(4):374-384.
7. Liu, L., Qian, X., Chen, Z. et al. Health literacy and its effect on chronic disease prevention: evidence from China's data. BMC Public Health 2020;20(1):690.
8. Eke PI, Thornton-Evans GO, Wei L, et al. Periodontitis in US adults: National Health and Nutrition Examination Survey 2009-2014. J Am Dent Assoc.2018;149(7):576-588.e6.
9. Dental Caries (Tooth Decay) in Adults (Age 20 to 64). National Institute of Dental and Craniofacial Research Web site. July 2018.https://www.nidcr.nih.gov/research/data-statistics/dental-caries/adults. Accessed March 29, 2021.
10. van der Heide I, Poureslami I, Mitic W, et al. Health literacy in chronic disease management: a matter of interaction. J Clin Epidemiol. 2018;102:134-138.
11. Eke PI, Dye BA, Wei L, et al. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res.2012;91(10):914-920.
12. National Institute of Dental and Craniofacial Research. Dental Caries (Tooth Decay) in Adults (Age 20 to 64). NIDCR; 2018. https://www.nidcr.nih.gov/research/data-statistics/dental-caries/adults
13. Fleming E, Afful J. Prevalence of total and untreated dental caries among youth: United States, 2015-2016. NCHS Data Brief. 2018;(307):1-8.
14. Rasu RS, Bawa WA, Suminski R, et al. Health literacy impact on national healthcare utilization and expenditure. Int J Health Policy Manag. 2015;4(11):747-755.
15. Dewalt DA, Berkman ND, Sheridan S, et al. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228-1239.
16. What is health literacy? Centers for Disease Control and Prevention Web site. January 28, 2921. https://www.cdc.gov/healthliteracy/learn/index.html. Accessed March 26, 2021.
17. Standards for Clinical Dental Hygiene Practice. American Dental Hygienists' Association. 2016. https://www.adha.org/resources-docs/2016-Revised-Standards-for-Clinical-Dental-Hygiene-Practice.pdf. Accessed March 29, 2021.
18. Borrell LN, Crawford ND. Socioeconomic position indicators and periodontitis: examining the evidence. Periodontol 2000. 2012;58(1):69-83.
19. Office of Disease Prevention and Health Promotion. Health literacy in Healthy People 2030. U.S. Department of Health and Human Services Web site. https://health.gov/our-work/healthy-people/healthy-people-2030/health-literacy-healthy-people-2030. Accessed March 26, 2021.
20. 9th Global Conference on Health Promotion, Shanghai 2016. The role of governments in promoting health literacy. World Health Organization Web site.https://www.who.int/healthpromotion/conferences/9gchp/health-literacy-government-role/en/. Accessed March 26, 2021.
21. Eke PI, Thornton-Evans GO, Wei L, et al. Periodontitis in US Adults: National Health and Nutrition Examination Survey 2009-2014. J Am Dent Assoc. 2018;149(7):576-588.e6.
22. Committee on Oral Health Access to Services, Institute of Medicine and National Research Council. (2011). Improving access to oral health care for vulnerable and underserved populations. Washington, D.C.: The National Academies Press. https://www.hrsa.gov/sites/default/files/publichealth/clinical/oralhealth/improvingaccess.pdf. Accessed March 29, 2021.
23. Kutner M, Greenberg E, Jin Y, Paulsen C. (2006). The Health Literacy of America's Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006-483). U.S. Department of Education. Washington, DC: National Center for Education Statistics. https://nces.ed.gov/pubs2006/2006483.pdf. Accessed March 29, 2021.